The study of the increasing incidence of melanoma over the past few decades is essential regarding prevention and optimization of health resources.
We collected cases of melanoma from Hospital son Llàtzer from the Migjorn health sector of Mallorca, Spain from 2003 through 2021, and calculated the incidence of melanoma adjusted to the standard European population. In addition, other demographic and clinicopathological data were descriptively analyzed too.
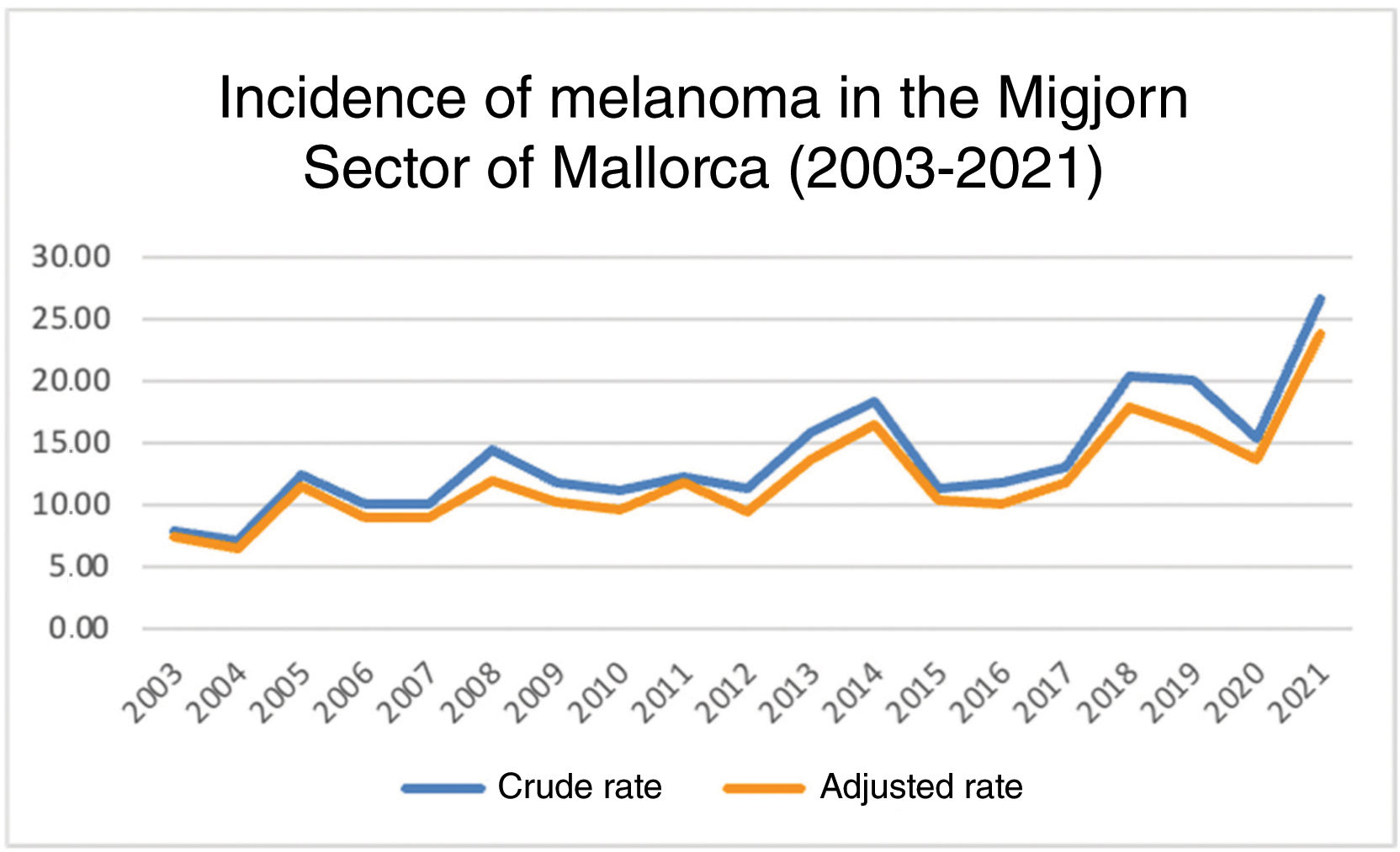
A total of 690 new cases of melanoma were detected with a progressive increase in the age-standardized incidence from 7.47 cases per 100,000 inhabitants/year in 2003 up to 23.84 in 2021 mainly due to early stages of the disease.
The incidence of melanoma has increased significantly in Mallorca probably due to the increasing population coming from northern Europe (low phototypes), sun exposure habits (tourism, fishing, agriculture), and improved early diagnosis.
El estudio del incremento de la incidencia del melanoma durante las últimas décadas es fundamental para su prevención y la optimización de recursos sanitarios.
Se recogieron los casos de melanoma en el Hospital Son Llàtzer, en el sector Migjorn de Mallorca, desde 2003 a 2021 y se calculó la incidencia ajustada a la población europea estándar. Además, se analizaron descriptivamente otros datos demográficos y clínico-patológicos.
Se detectaron 690 nuevos casos de melanoma con un aumento progresivo de la tasa de incidencia estandarizada por edad de 7,47 casos por 100.000 habitantes/año en 2003 a 23,84 en 2021, fundamentalmente a expensas de estadios tempranos.
La incidencia de melanoma ha aumentado significativamente en Mallorca, probablemente por el incremento de la población originaria del norte de Europa (fototipos bajos), los hábitos de exposición solar (turismo, pesca, agricultura) y la mejora en el diagnóstico temprano.
Although melanoma accounts for 4% of skin cancers, it is responsible for most skin cancer-related deaths.1 Its incidence has increased in recent decades both in the United States and Europe. Specifically, within the European territory, Spain has the lowest incidence and mortality rates. Still, some studies show a growing trend in the incidence of melanoma in this country too.2–5
Furthermore, understanding the incidence of melanoma in each region, as well as its distribution by age, sex, Breslow index, histological subtype, and location, is essential for organizing public health campaigns for the prevention or early detection of melanoma.
Therefore, the objective of this study was to analyze the epidemiological changes of melanoma in a region of Mallorca, Spain—the Migjorn sector—which falls within the coverage area of Hospital Son Llàtzer, which covers approximately 270,000 people, representing 25% of the overall population living in the island.
Case reports/PatientsThe study included all patients diagnosed with melanoma at Hospital Universitario Son Llàtzer from January 1st, 2003 through December 31st, 2021.
Material and methodsWe conducted a cross-sectional study that analyzed a database including patients diagnosed with cutaneous melanoma from 2003 through 2021 in Hospital Son Llàtzer coverage area (Migjorn sector, Mallorca). Epidemiological data were obtained from the Spanish National Institute of Statistics and the Balearic Islands Institute of Statistics as well.6,7 The study database included the patients’ age and sex, melanoma location and histological subtype, Breslow index, and stage at diagnosis.
We conducted a descriptive analysis, and the rate of crude and age-adjusted rate of in-hospital melanoma was calculated based on the reference European population.8 All cases of invasive and in situ cutaneous melanoma, including all ages, were analyzed from the diagnostic records of our hospital Pathology Department. Mucosal melanomas or other extracutaneous locations were not included.
The standardized European population and the direct method were used to age-standardize the in-hospital melanoma rate to avoid any confounding effects from age and compare it with the incidence rates from studies conducted in different countries and regions.8
We conducted a descriptive analysis of all variables, expressing qualitative variables as frequency and percentage of the total. Normality studies (Kolmogorov-Smirnov test) were conducted for quantitative variables for the subsequent selection of parametric and non-parametric tests. These variables were expressed as median and interquartile range in case of non-normality. The age-adjusted incidence rate associated with the reference European population was calculated. Statistical analyses were performed using SPSS version 23 (IBM, NY, United States). All statistical analyses were bilateral, with p values <0.05 being statistically significant.
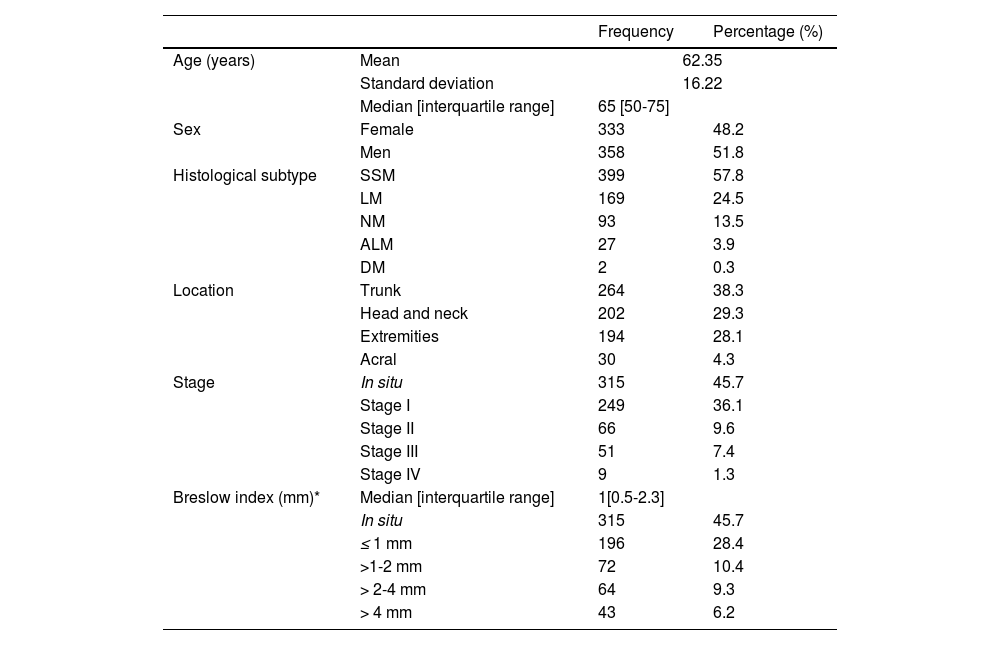
ResultsA total of 690 new cases of cutaneous melanoma were recorded over the 19-year study period (2003-2021). A total of 45.5% of melanomas were in situ, and 51.9% of the patients were men. The median age at diagnosis was 65 years, with the youngest patient being 19 years old and the oldest one, 97 years old. Regarding location, the trunk was the area with the highest rate of melanomas (38.26%), followed by the head and neck (29%) and extremities (28%). The most common histological subtype was superficial spreading melanoma (57.82%), followed by lentigo maligna (24.49%). The median Breslow index was 1mm (Table 1).
Baseline characteristics of the cohort of patients diagnosed with melanoma from 2003 through 2021.
| Frequency | Percentage (%) | ||
|---|---|---|---|
| Age (years) | Mean | 62.35 | |
| Standard deviation | 16.22 | ||
| Median [interquartile range] | 65 [50-75] | ||
| Sex | Female | 333 | 48.2 |
| Men | 358 | 51.8 | |
| Histological subtype | SSM | 399 | 57.8 |
| LM | 169 | 24.5 | |
| NM | 93 | 13.5 | |
| ALM | 27 | 3.9 | |
| DM | 2 | 0.3 | |
| Location | Trunk | 264 | 38.3 |
| Head and neck | 202 | 29.3 | |
| Extremities | 194 | 28.1 | |
| Acral | 30 | 4.3 | |
| Stage | In situ | 315 | 45.7 |
| Stage I | 249 | 36.1 | |
| Stage II | 66 | 9.6 | |
| Stage III | 51 | 7.4 | |
| Stage IV | 9 | 1.3 | |
| Breslow index (mm)* | Median [interquartile range] | 1[0.5-2.3] | |
| In situ | 315 | 45.7 | |
| ≤ 1 mm | 196 | 28.4 | |
| >1-2 mm | 72 | 10.4 | |
| > 2-4 mm | 64 | 9.3 | |
| > 4 mm | 43 | 6.2 | |
ALM, acral lentiginous melanoma; DM, desmoplastic melanoma; LM, lentigo maligna; NM, nodular melanoma; SSM, superficial spreading melanoma.
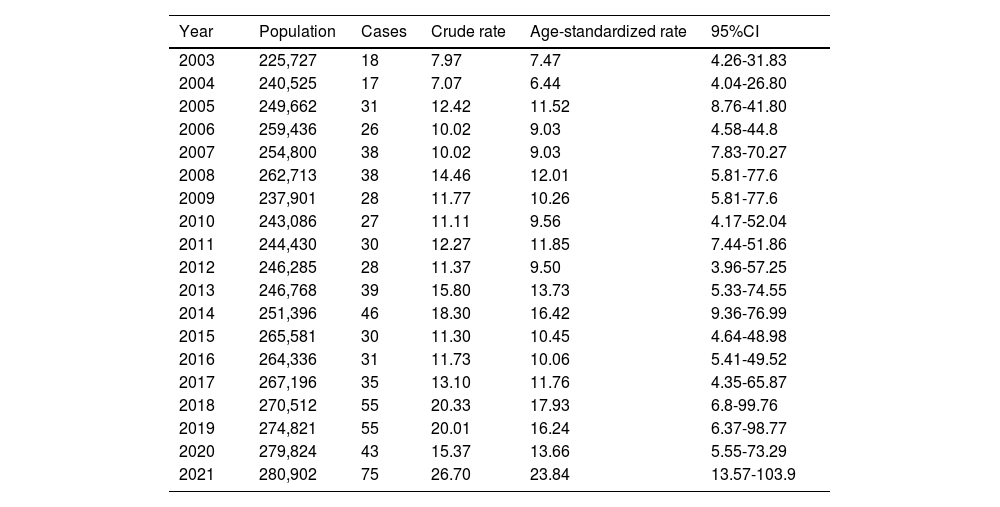
The age-standardized in-hospital rate is summarized in Table 2. During the study period (2003-2021), an increasing trend was observed in the age-standardized incidence of melanoma cases per 100,000 inhabitants, increasing from 7.47 (95% confidence interval [CI], 4.26–31.83) cases in 2003 up to 23.84 (95%CI, 13.57-103.9) in 2021 (Figure 1). However, from 2019 through 2020, this incidence dropped from 16.24 (95%CI, 6.37-98.77) cases down to 13.66 (95%CI, 5.55-73.29), before rising again in 2021 up to 23.84 (95%CI, 13.57-103.9). The increased incidence rate of melanomas in situ is significant. In 2021, they accounted for 44% of all melanoma diagnoses vs 33% in 2003.
Age-adjusted melanoma incidence rates.
| Year | Population | Cases | Crude rate | Age-standardized rate | 95%CI |
|---|---|---|---|---|---|
| 2003 | 225,727 | 18 | 7.97 | 7.47 | 4.26-31.83 |
| 2004 | 240,525 | 17 | 7.07 | 6.44 | 4.04-26.80 |
| 2005 | 249,662 | 31 | 12.42 | 11.52 | 8.76-41.80 |
| 2006 | 259,436 | 26 | 10.02 | 9.03 | 4.58-44.8 |
| 2007 | 254,800 | 38 | 10.02 | 9.03 | 7.83-70.27 |
| 2008 | 262,713 | 38 | 14.46 | 12.01 | 5.81-77.6 |
| 2009 | 237,901 | 28 | 11.77 | 10.26 | 5.81-77.6 |
| 2010 | 243,086 | 27 | 11.11 | 9.56 | 4.17-52.04 |
| 2011 | 244,430 | 30 | 12.27 | 11.85 | 7.44-51.86 |
| 2012 | 246,285 | 28 | 11.37 | 9.50 | 3.96-57.25 |
| 2013 | 246,768 | 39 | 15.80 | 13.73 | 5.33-74.55 |
| 2014 | 251,396 | 46 | 18.30 | 16.42 | 9.36-76.99 |
| 2015 | 265,581 | 30 | 11.30 | 10.45 | 4.64-48.98 |
| 2016 | 264,336 | 31 | 11.73 | 10.06 | 5.41-49.52 |
| 2017 | 267,196 | 35 | 13.10 | 11.76 | 4.35-65.87 |
| 2018 | 270,512 | 55 | 20.33 | 17.93 | 6.8-99.76 |
| 2019 | 274,821 | 55 | 20.01 | 16.24 | 6.37-98.77 |
| 2020 | 279,824 | 43 | 15.37 | 13.66 | 5.55-73.29 |
| 2021 | 280,902 | 75 | 26.70 | 23.84 | 13.57-103.9 |
CI, confidence interval.
The present study describes the Spanish series of melanoma cases with the longest observation period to this date. We studied the population with primary cutaneous melanoma in the sector covered by Hospital Universitario Son Llàtzer. Over the 19 years of data collection, we reported a total of 690 new diagnoses of primary cutaneous melanoma in a population of more than 250,000 inhabitants. The patients’ demographic characteristics of and the clinicopathological features of the tumors described in this study are consistent with what former studies have reported to this date4,5,9–13 (Appendix Table 3).
We observed an increase in the total incidence rate during the study period (7.47 cases per 100,000 inhabitants in 2003 up to 23.84 cases per 100,000 inhabitants in 2021). This increase could be related to various causes such as cumulative lifetime sun exposure habits of the population currently at higher risk of developing melanoma and improved diagnostic accuracy over this period, especially with the widespread use of dermoscopy among others. In 2020, a drop of 2.58 cases per 100,000 inhabitants (from 16.24 cases per 100,000 inhabitants in 2019 down to 13.66 per 100,000 inhabitants in 2020) was reported, which was consistent with the national skin tumor incidence rate for that period.14 This incidence decrease is consistent with the start of the COVID-19 pandemic, a time during which access to primary and hospital health care became more complicated.
We should mention that the largest increase in incidence corresponds to early stages, probably due to improved early detection of cases for reasons such as greater public awareness, and improved knowledge among dermatologists and non-dermatologists (Appendix Figures 2 and 3).
Furthermore, incidence rates higher than the Spanish national average were reported too4,5,11,15,16 (Appendix Table 4). However, our incidence rates probably underestimate the actual incidence rate since almost 30% of the population in Mallorca has private health insurance, and it is precisely in this population in which melanomas—that have gone unreported this his series—are indeed detected. This may explain why the reported incidence rates are lower than expected, given some of characteristics inherent to our population such as widespread sun exposure habits (fishermen, farmers, sun and beach tourism), high UV radiation levels in the region, increasing immigration from countries with high melanoma rates (Central and Northern Europe), and the intermingling of the local population with people born in these countries.
The main limitations of our study are that it is a cross-sectional study without patient follow-up. Additionally, we only studied part of the island population, corresponding to the coverage area of one single hospital, and we lack data on melanoma diagnoses made in private clinics and hospitals, which we estimate could be significant.
In conclusion, the population with melanoma from the Migjorn sector has similar demographic characteristics to the rest of Spain. We saw a progressive increase in the incidence rates reported during the study period, which is consistent with data from other series. This incidence increase is due to early-stage melanomas, likely thanks to improved diagnostic techniques and awareness campaigns among health care professionals and the general population too.