Cutaneous apocrine carcinoma is a rare malignant tumor with a poor prognosis.1 Invasive extramammary Paget disease (EMPD) is an uncommon form of adenocarcinoma that mainly arises in the area of the apocrine glands; it has a worse prognosis than EMPD in situ and a higher risk of underlying malignancy.2 Pagetoid epidermal spread is rare in apocrine carcinoma.1 Very few cases have been described and the histogenesis is unknown.2–5 HER2/neu (c-erbB-2) is overexpressed in approximately 20% to 60% of EMPD cases, and few patients have responded favorably to the recombinant anti-HER2 monoclonal antibody trastuzumab, either alone or in combination with paclitaxel.2,3 As occurs in HER2-positive breast cancer, overexpression of HER2/neu in EMPD leads to increased tumor cell proliferation and is associated with more aggressive behavior and more recurrences.2,4
We describe the case of a patient with invasive metastatic apocrine adenocarcinoma and inguinal EMPD who showed a near-complete response to dual HER2 blockade (trastuzumab and pertuzumab) that enabled him to undergo salvage surgery.
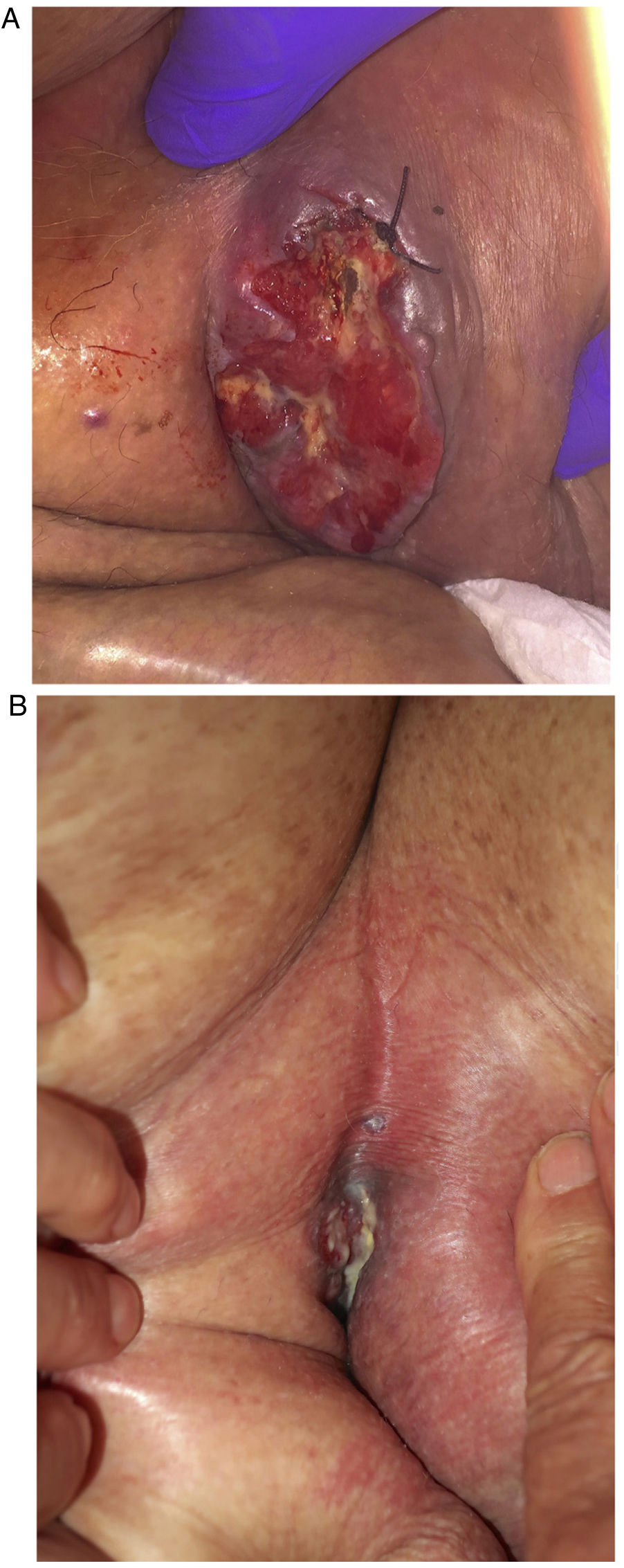
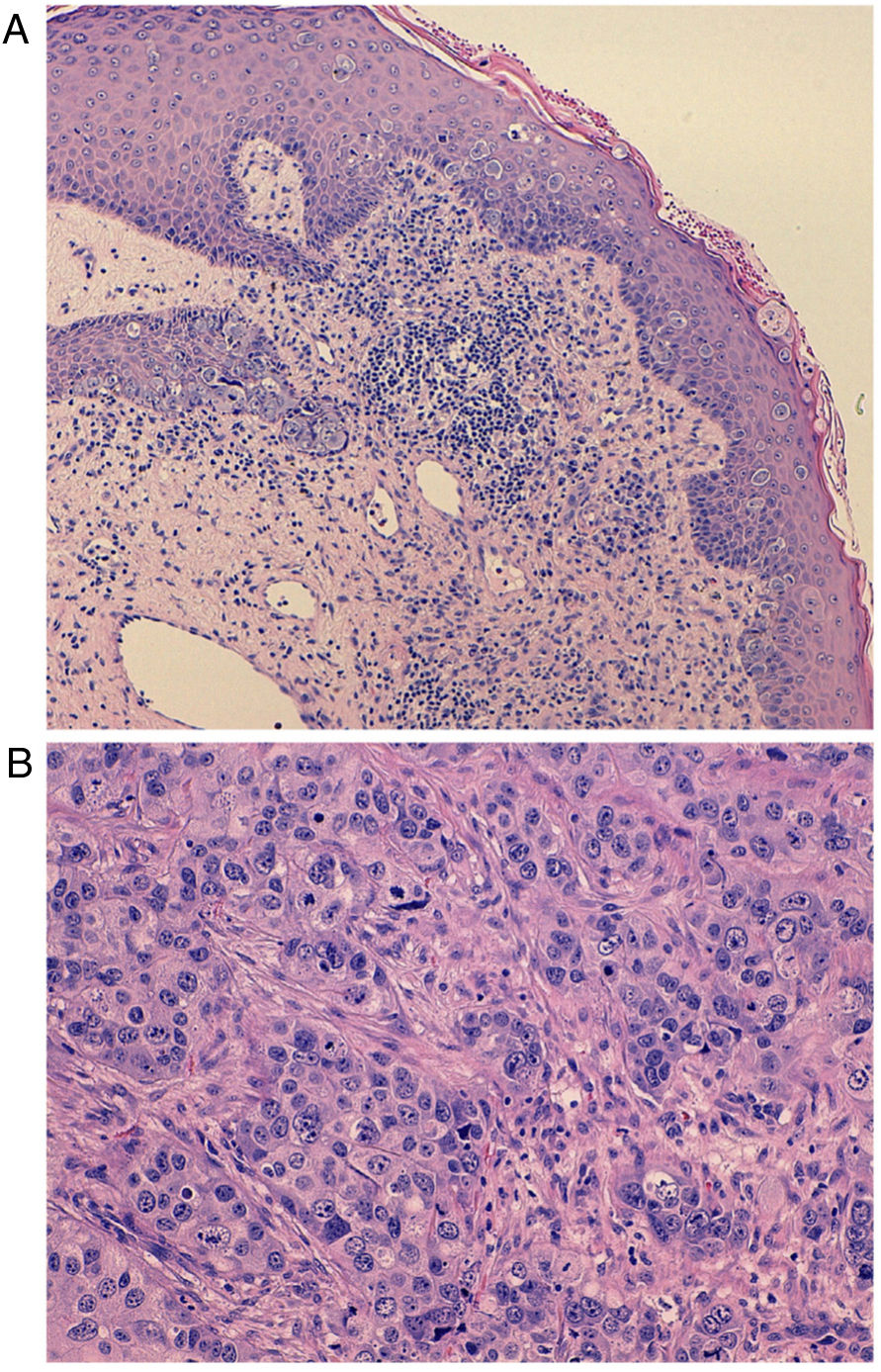
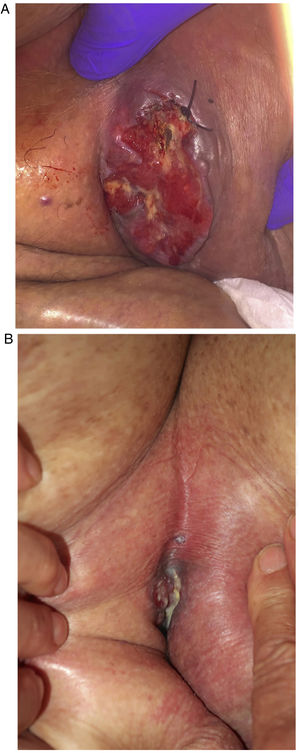
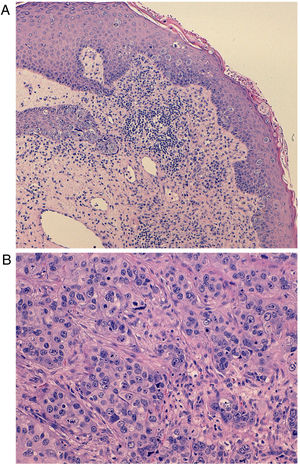
An 80-year-old man presented with a 9-cm left inguinal mass of 8 months’ duration that was fixed to the deep planes (Fig. 1A). He was on multiple medications and had a history of hypertension, diabetes mellitus, ischemic heart disease, chronic heart failure, atrial fibrillation, chronic renal failure, and morbid obesity. Microscopic examination of a partial biopsy specimen showed features suggestive of Paget cells: atypical polygonal cells with round nuclei and clear granular cytoplasm at the dermal-epidermal junction (Fig. 2A). In the dermis, there was a well-circumscribed, nonencapsulated tumor nodule with dilated lumina and a nested tubular-cribriform pattern (Fig. 2B). The tumor cells were pleomorphic and had a granular eosinophilic cytoplasm with apocrine-like changes, significant mitotic activity, and comedonecrosis. The cells stained diffusely for cytokeratin (CK) 7, CAM5.2, GATA3, carcinoembryonic antigen; focally for Ber-EP4; and negatively for CK20, MART-1, prostate-specific antigen, uroplakin-III, and S100 protein, confirming their apocrine nature. HER2/neu was also expressed in 90% of the tumor cells. These findings were consistent with adnexal apocrine adenocarcinoma and cutaneous EMPD. Magnetic resonance imaging showed a heterogeneous tumor measuring 8cm×9cm in the left groin with invasion of the dermis and subcutaneous tissue. Also visible were enlarged left inguinal and retroperitoneal metastatic lymph nodes. No breast lesions or other primary malignant lesions were found on positron emission tomography. Due to the unresectable, inoperable nature of the tumor, it was decided to administer palliative treatment with compassionate use of dual HER2 blockade with trastuzumab and pertuzumab as an alternative to potentially more toxic chemotherapy. The dosing regimen was a standard regimen used in metastatic breast cancer (subcutaneous trastuzumab at a fixed dose of 600mg every 21 days and intravenous pertuzumab with a loading dose of 840mg followed by 420mg every 3 weeks).6 The treatment was well tolerated. Regular echocardiographic assessment of left ventricular function showed no evidence of dysfunction. By the end of the third cycle, the mass had almost completely resolved (reduction of 7cm) (Fig. 1B). MRI also showed normal-sized lymph nodes. This favorable response enabled complete excision of the residual tumor with negative margins. No recurrences were observed over 12 months of follow-up.
A, Intraepithelial proliferation of large, round, pale cells (Paget cells) dispersed through the epidermis with basophilic cytoplasm and enlarged central nuclei with nuclear atypia (hematoxylin-eosin, original magnification ×40). B, Underlying adenocarcinoma cells with mild nuclear pleomorphism. Note the deep invasion of the subcutaneous tissue and the nest and tubule arrangement (hematoxylin-eosin, original magnification ×100).
Just 6 cases of cutaneous apocrine carcinoma and inguinal EMDP have been described to date.1–3 Distinguishing between cutaneous apocrine adenocarcinoma and metastatic mammary apocrine carcinoma in the skin can be difficult because of overlapping histopathologic and immunohistochemical features.4 Clinically, cutaneous apocrine carcinoma and EMPD typically appear as an isolated mass in the apocrine areas (axilla, groin, scrotum, or perineal region) in patients aged between 46 and 82 years.1–5 They are locally aggressive and frequently spread to the regional lymph nodes (30%–60% of all cases).1–5 HER2/neu expression in Paget cells is associated with a poor prognosis in EMPD, but it also has therapeutic implications.2 A deep biopsy prior to surgery is required to assess depth of tissue invasion and rule out an underlying apocrine adenocarcinoma. The treatment of choice is wide surgical excision with regional lymph node dissection.7 Due to the rareness of this entity, there is no consensus regarding pharmacologic treatments. Both chemotherapy and hormone therapy have been shown to be ineffective.7–9 In HER2-positive metastatic breast cancer, by contrast, pertuzumab combined with trastuzumab and docetaxel is associated with longer progression-free survival than trastuzumab plus docetaxel or paclitaxel alone.8,9 Apocrine cutaneous glands are likely evolutionary precursors of mammary glands and could share HER2/neu pharmacological targets.10
We have described for the first time the use of neoadjuvant dual blockade to treat metastatic EMPD with an underlying apocrine adenocarcinoma. This treatment can be considered in selected patients, as there are no approved standard treatment regimens available to treat locally advanced, unresectable disease. This case illustrates the need to perform deep biopsies and evaluate HER2/neu expression in all cases of metastatic or invasive EMPD in order to determine the possibility of dual HER2 blockade with monoclonal antibodies as neoadjuvant therapy before surgery.
Conflicts of InterestThe authors declare that they have no conflicts of interest.