The increase in the number of cosmetic procedures in recent years means that in our daily practice we are seeing ever more side effects of the different techniques. One of these is the formation of granulomas secondary to dermal fillers; the etiology of these lesions can be difficult to determine, not only because patients neglect to inform us they have undergone cosmetic treatment or they are unaware of the type of material used, but also because the clinical presentation can be similar to that of certain dermatologic diseases.1 When medicolegal issues arise, the most useful additional test is biopsy, as each material presents a specific histologic pattern,2 but this is an invasive technique and patients may sometimes reject such tests. Skin ultrasound is an alternative, non-invasive test that, through specific sonographic patterns, can identify the type of material involved and its exact site.
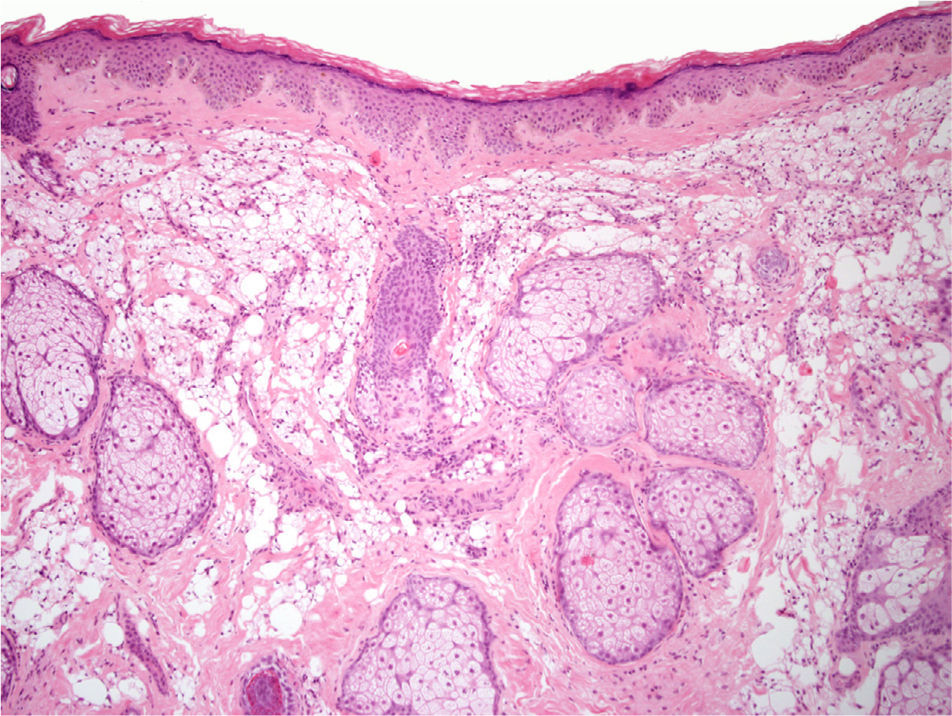
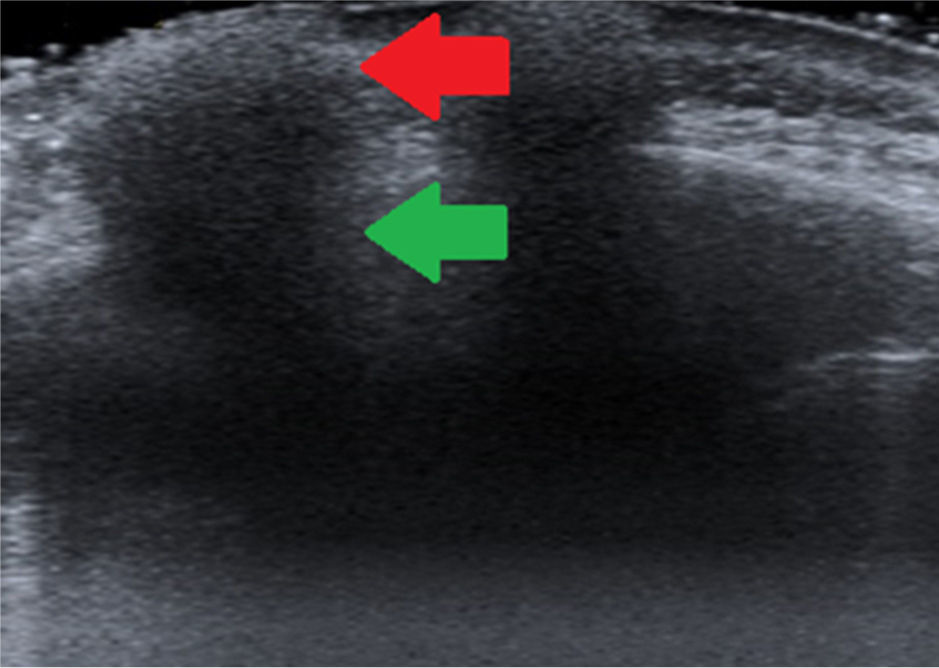
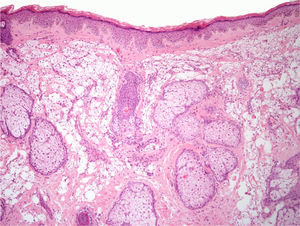
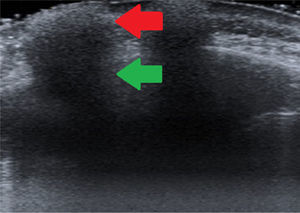
We present the case of a 52-year-old woman who came to outpatients for multiple asymptomatic lesions on the forehead. The first lesions had appeared in the glabellar region 8 years earlier and had remained stable until the year prior to consultation when, coinciding with the appearance of new lesions, she developed recurrent episodes of inflammation that persisted for several days and resolved spontaneously. Physical examination revealed yellowish-pink plaques of 1-2cm diameter, with well-defined borders, a firm consistency, and a peau d’orange appearance (Fig. 1). The only finding of interest in the patient's past history was the injection of a filler material 14 years earlier; she was unable to specify what the material was. On biopsy there were abundant foamy histiocytes suggestive of a histiocytic reaction to the filler material (Fig. 2). Due to the lack of specific findings, we decided to perform skin ultrasound to identify the filler material employed. The study revealed hyperechoic images that had no clearly visible border and that left an acoustic shadow; the images were present in the skin and deeper tissues of the frontal and malar regions and of the chin. The sonographic pattern corresponded to the so-called snowstorm sign (Fig. 3), which is compatible with a diagnosis of siliconomas. In this case, skin ultrasound enabled us to define the type of material employed and its presence in other areas in addition to those in which the patient stated the injections had been performed. This made it possible to plan management. At the time of writing, the patient had completed 3 months of treatment with isotretinoin, 0.4mg/kg/d, which has led to a partial improvement in the lesions.
High-frequency ultrasound is a simple and rapid non-invasive technique with a good cost-efficacy relationship. The technique enables us to identify the nature, volume, and site of the injected material. The thickness of the soft tissues does not affect image quality, and the material in question can be identified in 97.5% of cases.3
Ultrasound can differentiate between reabsorbable and permanent filler materials, though it cannot distinguish between different materials of the same class. Absorbable materials are seen as anechoic or hypoechoic masses with the appearance of cysts whereas permanent materials produce a hyperechoic pattern; semiabsorbable materials are seen as hypoechoic areas that contain foci of variable echogenicity. Liquid silicone can produce a specific pattern known as a snowstorm pattern because of the presence of multiple hyperechoic collections with an acoustic shadow.2
We consider that skin ultrasound can be very useful when filler materials give rise to complications and it can provide a valid alternative for those patients who, for whatever reason, do not wish to undergo biopsy. Ultrasound establishes the clinical diagnosis more accurately than other imaging studies—the presence of a permanent material, such as calcium hydroxyapatite, can give false positive results with magnetic resonance, computed tomography, and positron emission tomography.4 In addition, ultrasound can aid decision-taking regarding subsequent treatment as, for example, the presence of a permanent filler material would contraindicate treatment with interferon.5,6 Ultrasound can also help us to orient patients about the prognosis as, in contrast to reabsorbable filler materials, granulomatous reactions to permanent materials are unlikely to resolve in less than 6 months. Furthermore, knowledge of the site and nature of a filler material will make it possible to avoid future complications if further interventions are to be performed at the same site. Finally, some authors consider that ultrasound study improves the patient's awareness of the cosmetic results achieved and, in those patients not convinced of the persistence of an injected material, the ultrasound images can reinforce their perception of the definitive results.7
In our opinion, although biopsy continues to be the gold standard for the definitive diagnosis of the side effects of an injected filler material, skin ultrasound is a valid and useful alternative diagnostic method in patients who reject invasive diagnostic tests.
Please cite this article as: Menis D, Castellanos-González M, Llamas-Martín R, Vanaclocha Sebastián F. Utilidad de la ecografía cutánea en el diagnóstico de las complicaciones por materiales de relleno. Actas Dermosifiliogr. 2014;105:797–798.