Teledermatology was introduced in Chile to make up for the lack of dermatologists and improve the primary care system's ability to resolve problems. This strategy was implemented in the province of Palena in 2013, but outcomes were not analyzed and reported until now.
Material and methodsDescriptive, cross-sectional study with analysis of inter-rater agreement on diagnoses. All the teledermatology consultations made on behalf of patients in Ayacara, Chaitén, Futaleufú, and Palena from 2013 through 2017 were analyzed. Data were extracted from the MINSAL platform. The κ statistic was used to assess diagnostic agreement.
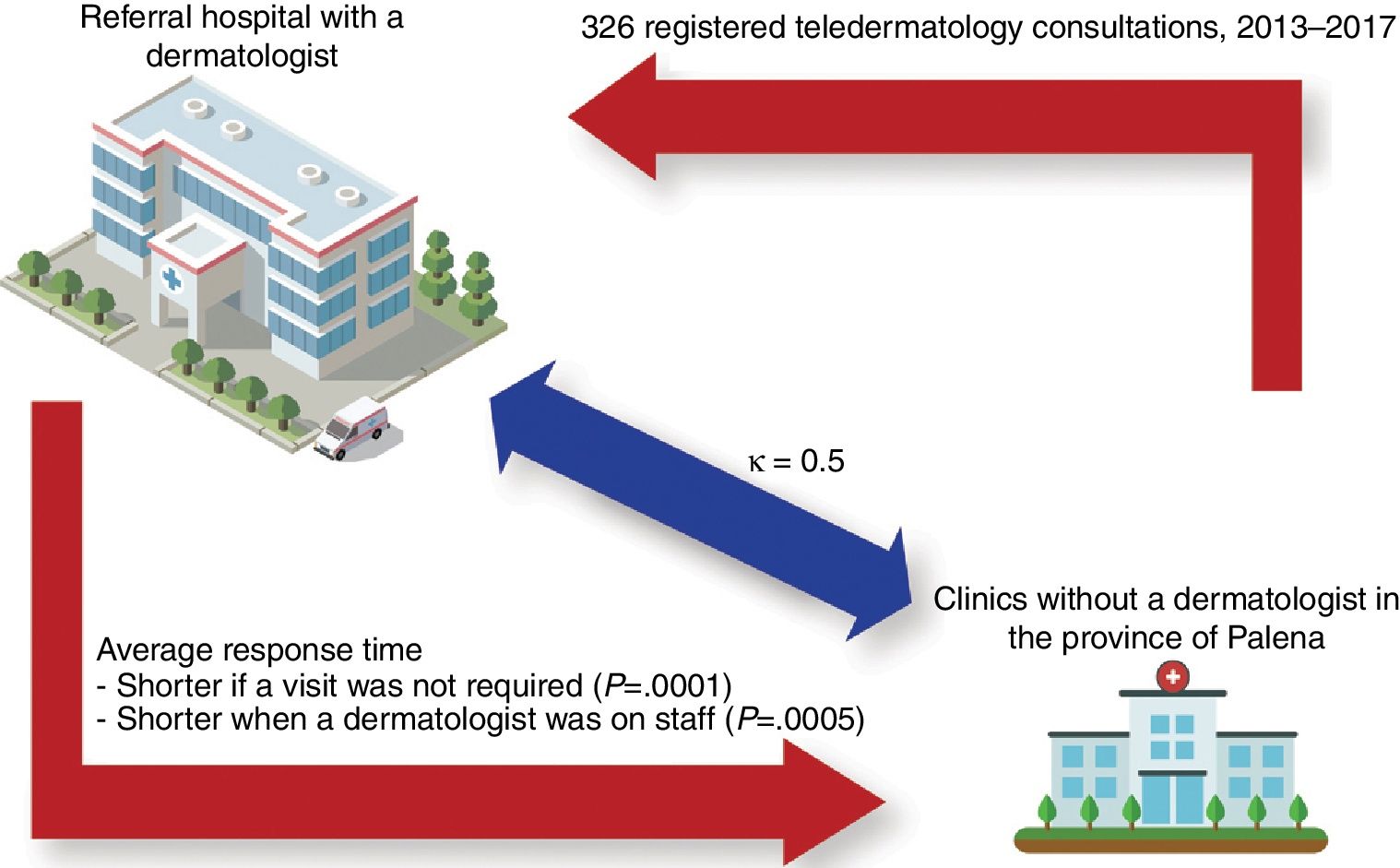
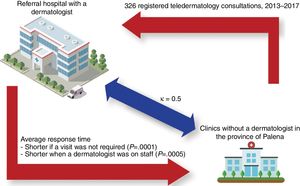
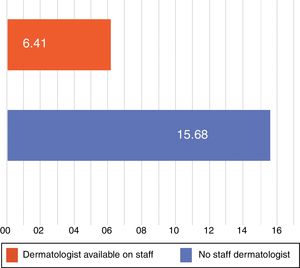
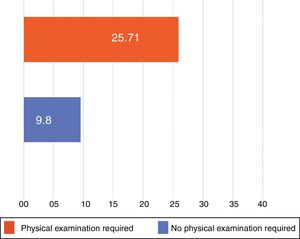
ResultsA total of 326 teledermatology consultations were made. The mean (SD) age of the patients was 35.8 (22.4) years. The majority (59.8%) were female. Palena generated the largest volume of cases (40.8%). The mean time until a teledermatology diagnosis was given was 12.6 (22.8) days. This response time decreased to 6.4 (5.2) days after a staff dermatologist from Hospital Puerto Montt joined the program (P=.0005). Diagnosis concordance between the general practitioner and the dermatologist was moderate (κ=0.5). Physical examination by the dermatologist at the hospital of reference (Puerto Montt) was necessary for 20.6% of the patients, and time until a definitive diagnosis for the patient took longer in such cases (25.7 [41.2] days) than for the cases that didn’t need a physical evaluation at the Hospital of Puerto Montt (P<.0001).
ConclusionsTeledermatology provides a necessary diagnostic and therapeutic resource for general practitioners in isolated locations. Diagnostic agreement is moderate between the generalist and the specialist, similar to agreement in international studies but lower than agreement reported in other Chilean studies. The reduction in diagnostic response time after incorporation of a dermatologist on staff at the hospital of Puerto Montt was significant. The significant difference between the time for diagnosis under teledermatology and the delay when physical examination is required at the hospital of Puerto Montt identifies an aspect of care management to improve.
La teledermatología (TD) ha sido implementada en Chile como estrategia de salud para suplir el déficit de dermatólogos y aumentar la resolutividad de la atención primaria. Esta estrategia fue implementada en la Provincia de Palena en 2013, sin un análisis de las atenciones brindadas hasta la fecha.
Material y métodosEstudio descriptivo, transversal, de concordancia inter-observador. Se analizan todas las consultas por TD de Ayacara, Chaitén, Futaleufú y Palena desde 2013 a 2017. Datos obtenidos de plataforma MINSAL. Concordancia diagnóstica calculada con índice kappa.
ResultadosTotal 326 consultas de TD con promedio de edad de 35,8 años (DE: 22,4), en su mayoría de sexo femenino (59,8%). Mayoría de TD originadas en Palena, con un 40,8%. Tiempo de respuesta promedio de 12,6 días (DE: 22,8), disminuyendo a 6,4 días (DE: 5,2) tras la incorporación de dermatólogo en el Hospital de Puerto Montt (p=0,0005). Concordancia diagnóstica moderada entre el médico general y el dermatólogo, con índice kappa de 0,5. Un 20,6% de las consultas requirió evaluación presencial. Tiempo de respuesta promedio de 12,6 días (DE: 22,8), aumentando a 25,7 días (DE: 41,2) sí requirió evaluación presencial (p<0,0001).
ConclusionesLa TD es una herramienta diagnóstica y terapéutica necesaria para el médico general en zonas aisladas. La concordancia diagnóstica moderada es similar a estudios internacionales, pero inferior a estudios nacionales. Es relevante el menor tiempo de respuesta al incorporar un dermatólogo al servicio. La diferencia significativa entre el tiempo de respuesta de la consulta presencial versus la teleasistida requiere una mejor gestión asistencial.
Dermatologic diseases are among the most frequent reasons for consulting a primary care physician in Chile1 and first-world countries,2 with reported frequencies ranging from 5% to 19%.3 The scarcity of dermatologists in Chile's public health care system has an impact on access to prompt evaluation of skin lesions. Specialists are concentrated in the largest cities in the central areas of the country,4 a situation that has led to waiting lists and is difficult to remedy using the conventional resources available to health system managers.
Teledermatology has emerged as a tool that can help geographically isolated communities, where access to health care requires the investment of considerable amounts of time and expense.5 Telemedicine has been widely applied in other health care settings such as intensive care,6 palliative care,7 emergency services,8 and pediatrics.9 The Chilean Ministry of Health developed a store-and-forward teledermatology system in 2009 with the aim of increasing access to dermatologic evaluation for patients in primary care settings,10 and the system was launched in the Reloncaví area in 2013.
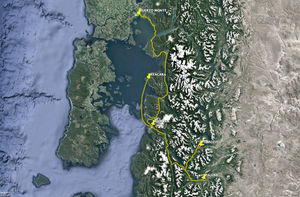
The Reloncaví province of Palena in the region of Los Lagos is one of the largest in Chile. Communities are widely dispersed across a territory that includes islands and peninsulas as well as villages on the main coast and in the mountains. The province has 4 communes, or administrative districts, as follows: Palena, Chaitén, Futaleufú, and Hualaihué. This study concentrates on teledermatology in the first 3 districts, where the delivery of services is complex due to the great dispersion of the population and extreme isolation (Fig. 1). Each of these districts has a hospital, or clinic, that manages several rural health care outposts, or stations. Communities in Chaitén are the most widely dispersed and it therefore has the largest number of outposts. In response to this district's geographic complexity, Chaitén also has a Community Family Health Center (known by its Spanish abbreviation, CECOSF) in Ayacara.
This study aimed to analyze the teledermatology support provided to 4 clinics in these 3 districts in terms of the demographic characteristics of the users, the mean time until a specialist diagnosis was reached, the need for direct physical evaluation by the dermatologist or not, and agreement between the diagnoses of the general practitioner and the dermatologist. We also explored possible associations between variables.
Material and MethodsThis was a descriptive, cross-sectional study with analysis of inter-rater diagnostic agreement. The data sample included all teledermatology consultations carried out between January 2013 and December 2017 registered in the 4 public health clinics belonging to the Reloncaví Health Care Services of the province of Palena in the region of Los Lagos, Chile. The clinics were the CECOSF in Ayacara, the Hospital de Chaitén, the Hospital de Futaleufú, and the Hospital de Palena. All are primary care clinics that manage health conditions of low levels of complexity. They are also the only providers of health care in their respective catchment areas. Their teledermatology reference center is Hospital de Puerto Montt.
Data were extracted from the digital teledermatology platform of the Reloncaví Health Care Services and input into a spreadsheet (Microsoft Excel, version 2016). The inclusion criteria were that a registered user of the platform had input the case and that the users worked at one of the 4 aforementioned primary health care clinics. Registered cases with missing data were excluded. Also excluded were cases rejected by the referral dermatologist because of lack of information (eg, an attached photograph).
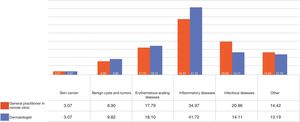
The following variables were analyzed: age, gender, health clinic initiating the consultation, general practitioner's diagnosis, dermatologist's diagnosis, need for direct physical examination by the dermatologist, and response time (time until the dermatologist's diagnosis was registered on the teledermatology platform). Diagnoses were grouped for analysis into 5 categories: skin cancer, benign cysts and tumors, erythematous-scaling diseases, inflammatory skin conditions, infectious diseases, and other.
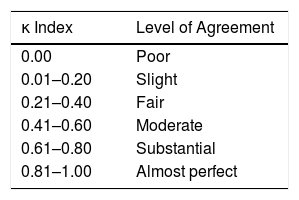
Quantitative variables were described as mean (SD) and qualitative variables by absolute and relative frequency. Inter-rater diagnostic agreement was calculated with the κ index and interpreted according to the scale proposed by Landis and Koch (Table 1).11 Statistical significance was set at a value of P<.05. The STATA program (version 10) was used for statistical analysis.
ResultsA total of 9405 persons live in the catchment areas of the 4 studied clinics of the province of Palena. A total of 326 teledermatology consultations were analyzed after application of the exclusion criteria (Fig. 2). The mean (SD) age of the patients was 35.8(22.4) years; 59.8% were women and 40.2% were men. Thirty-nine (12%) were being treated at the CECOSF in Ayacara, 82(25.2%) at Hospital de Chaitén, 72(22.1%) at Hospital de Futaleufú, and 133(40.8%) at Hospital de Palena.
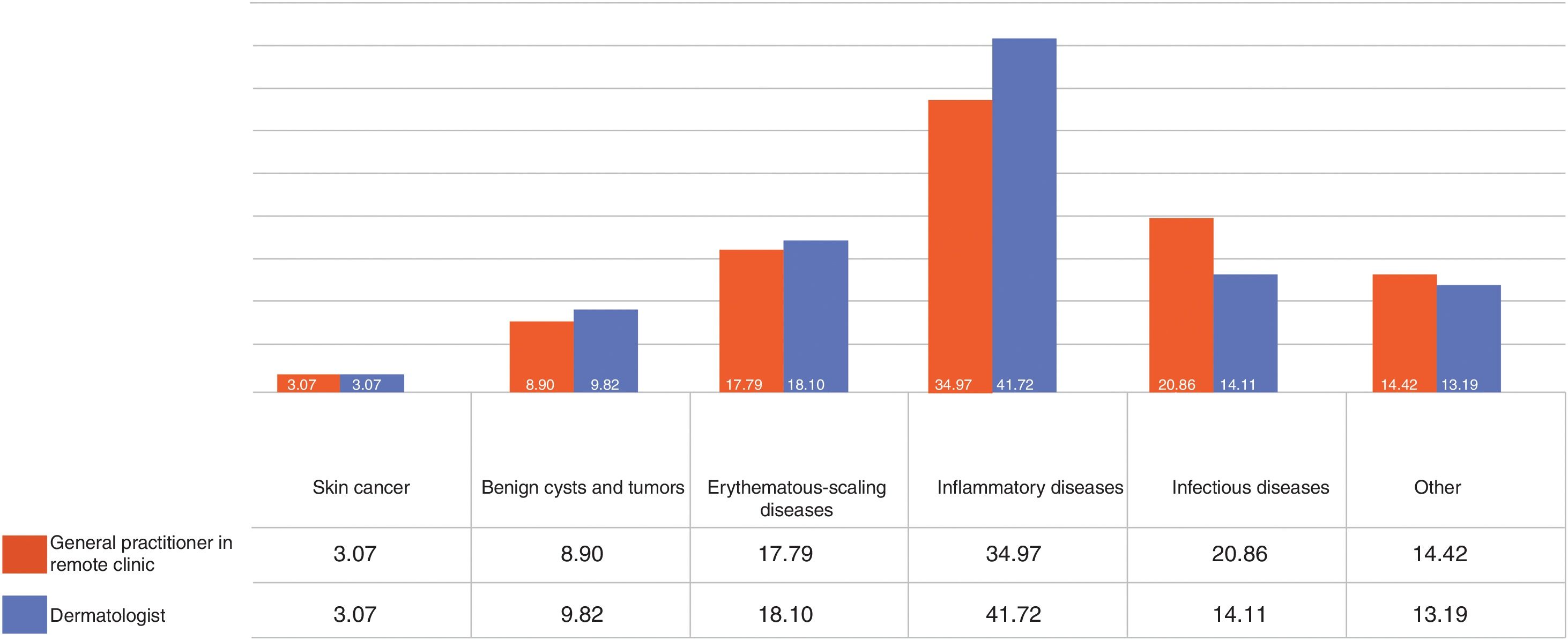
The general practitioners in the centers diagnosed some type of skin cancer in 3.1% of the cases, benign cysts or tumors in 8.9%, erythematous-scaling diseases in 17.8%, inflammatory skin conditions in 35%, infectious diseases in 20.9%, and other conditions in 14.4% (Fig. 3). The dermatologists, on the other hand, while also finding some type of skin cancer in 3.1% of the cases, diagnosed benign cysts or tumors in 9.8%, erythematous-scaling diseases in 18.1%, inflammatry skin conditions in 41.7%, infectious diseases in 14.1%, and other conditions in 13.2% (Fig. 3). The κ index of concordance between the 2 sets of diagnoses was 0.5, corresponding to moderate agreement according the scale proposed by Landis and Koch.11 Nine out of 10 cases of skin cancer were suspected by the general practitioner who initiated the teledermatology consultation.
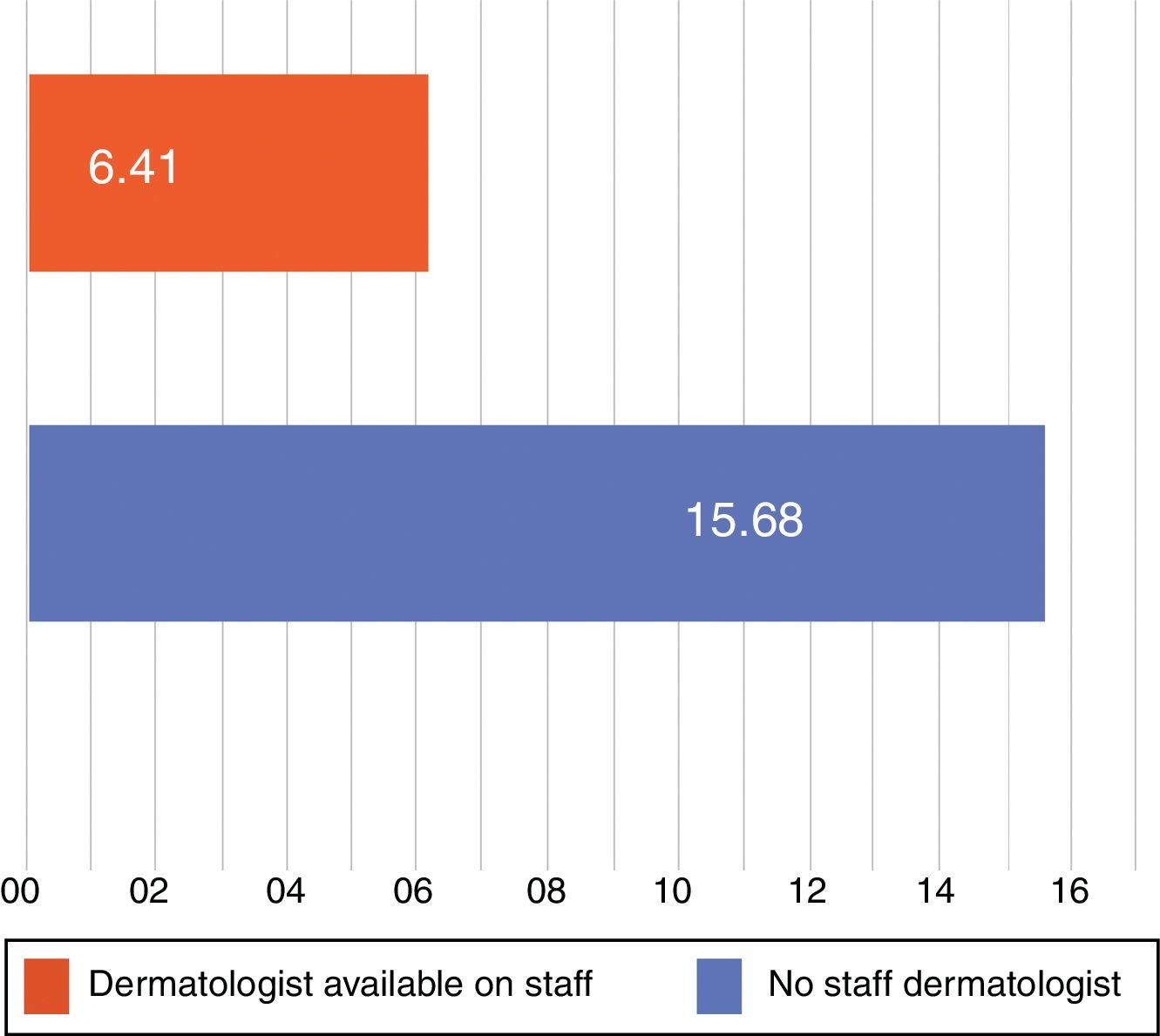
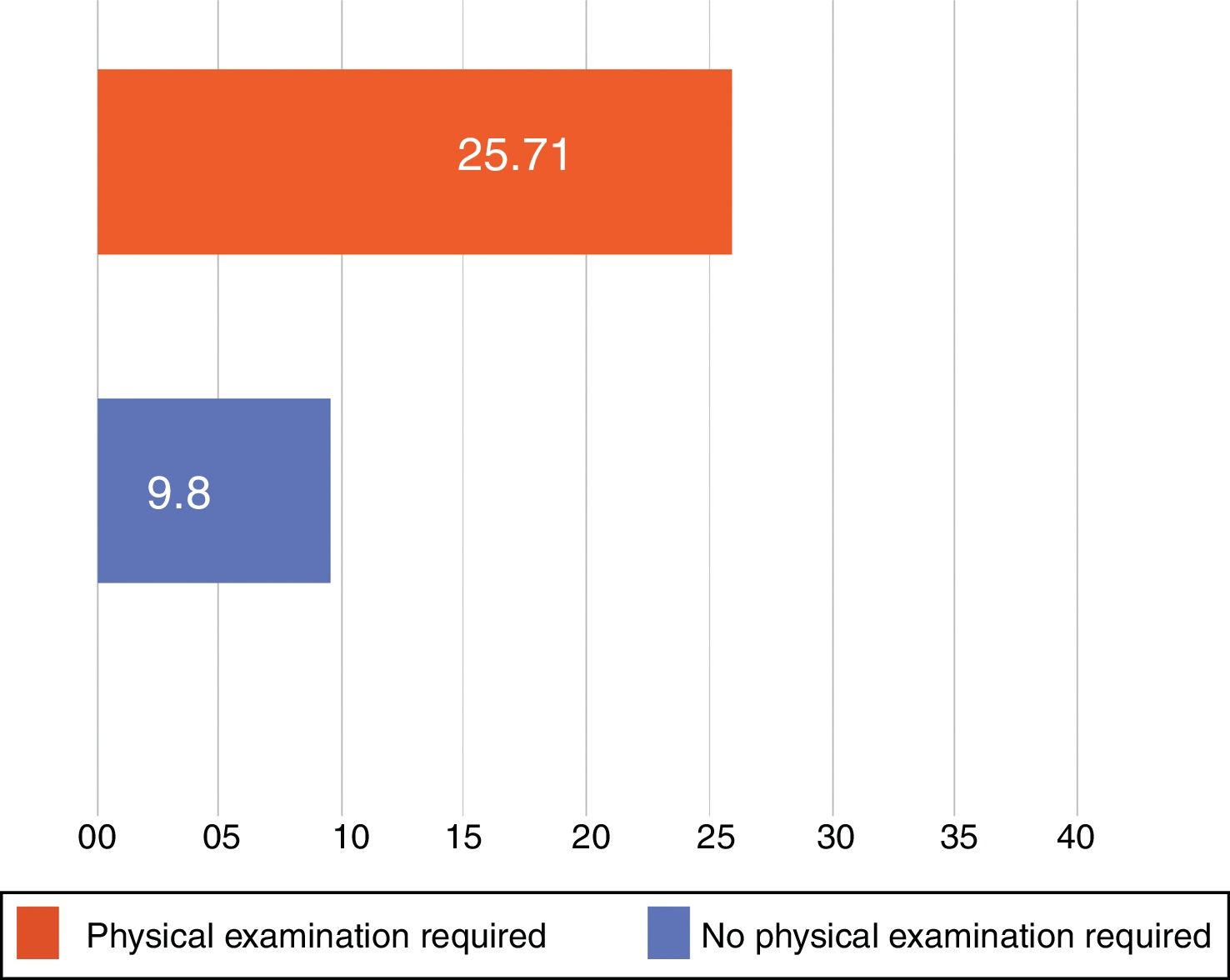
The mean (SD) response time (until the dermatologist's diagnosis at Hospital de Puerto Montt) was 12.6(22.8) days overall. The average response time decreased to 6.41(5.2) days once the specialist was permanently available on staff, down from 15.68(27.2) days in the period before the contract was in effect, a difference that was statistically significant (P=.0005) (Fig. 4). For patients who did not require direct physical evaluation at Hospital de Puerto Montt, the dermatologist's mean overall response time was 9.2 (12.7) days. In contrast, 25.71(41.2) days elapsed if the patient had to travel to the hospital for examination and diagnosis, a difference that was also significant (P<.0001) (Fig. 5). Only 20.6% of the patients registered in the teledermatology system required physical examination by a dermatologist.
A systematic review of the literature on store-and-forward teledermatology systems found that the number of cases in each study ranged from 12 to 882.12 Most studies included fewer than 200, which is to say, fewer than our present analysis. The average age of patients in these studies was 53 years, which is older than the average ages of patients in 2 other Chilean studies5,13 and our study. The reviewers also found that more of the patients studied in the literature were men (57%), whereas our study had more women.
The clinic that registered the fewest teledermatology consultations in our study was the CECOSF in the peninsular sector of Ayacara, which is isolated by land and has a population of only 949 individuals.14 The largest community studied, Chaitén with a population of 5071 inhabitants,15 did not generate the largest number of consultations; instead, it was the Hospital de Palena, with 1711 inhabitants in its catchment area15 that did so. This observation may be attributable to the limited internet connection after the volcanic eruption of 2008 and the fact that the proximity of the Hospital de Palena to the city of Puerto Montt could have encouraged direct consultation of public or private dermatologists.
Inflammatory skin diseases (dermatitis and similar conditions) generated the largest number of teledermatology consultations registered by both primary care clinics and the dermatologist at Hospital de Puerto Montt. These findings are similar to those reported by some other authors in Chile5,13 and abroad,16 even though different classifications were used. However, our observations are not consistent with reports of higher proportions of consultations for infectious diseases registered by other primary care clinics in similar areas of Chile.17,18 The discrepancies may be attributable to the degree of diagnostic doubt associated with inflammatory skin conditions, which have signs and symptoms that resemble those of other diseases. This argument supports the use of teledermatology to support general practitioners.
Agreement between general practitioners’ and dermatologists’ diagnoses has been assessed in at least 4 studies in Chile,13,19–21 which reported higher levels of agreement (between 0.65 and 0.83) than we observed. However, a study carried out in India16 reported a similar level of agreement to ours. These findings identify a critical gap in some general practitioners’ training and a need to improve their ability to identify dermatologic diseases.
Finally, the average response time (diagnostic delay) varied greatly according to whether a physical examination was required and whether or not a dermatologist at Hospital de Puerto Montt responded to consultations occasionally or was on staff at that reference hospital. These significant differences reflect the public health system's problems in managing the delivery of care in remote regions, showing that a contracted specialist can drastically decrease waiting times. Furthermore, the fact that longer waiting times are associated with the need for direct physical examination of the patient shows that there is considerable delay in assigning follow-up visits, possibly attributable to either the scarce availability of dermatologists or administrative delays in scheduling. Fortunately, only a little over a fifth of the teledermatology consultations required physical examination for diagnosis, showing that the primary care system has great potential to resolve most cases if supported by this innovative approach.
ConclusionsThis in-depth analysis of the actual clinical use of a teledermatology system supports its use for the delivery of public health care. The approach is potentially very important for patients in remote areas who otherwise would have no access to specialists. General practitioners need further training to hone their diagnostic skills. Strategies to arrange transport for patients who urgently need to be examined physically should be developed. Further studies of this approach in other districts with isolated communities are needed to provide additional examples of how far this technology can be extended.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González Coloma F. Teledermatología aplicada en zonas extremas: expieriencia de 4 centros asistenciales chilenos en ámbito rural y aislamiento extremo. Actas Dermosifiliogr. 2019;110:653–658.