Follicular lymphoma (FL) constitutes approximately 30% of all non-Hodgkin lymphomas in Western countries. Clinical presentation is typically in the form of lymphadenopathy, hepatomegaly, splenomegaly and bone marrow infiltration.1,2 Extranodal involvement is less frequent than in large B-cell lymphoma2 and does not appear to affect prognosis; this is not the case with B-cell lymphoma.
We report the case of a patient diagnosed with FL who developed skin nodules in the course of her disease. The lymphoma recurred after treatment, but it was exclusively limited to the skin, an unusual observation in this disease.
The patient was a 54-year-old woman who was referred to the hematology department in August 2004 for thrombocytopenia detected during a routine blood analysis (platelet count 70×109/L). Monoclonal B-cell lymphocytosis in the peripheral blood and bone marrow, enlarged subcentimeter abdominal lymph nodes and splenomegaly were observed during the study. The diagnosis was chronic B-cell lymphoproliferative syndrome and the patient was offered splenectomy, which she refused at that time. At follow-up in January 2007, enlarged mediastinal and retroperitoneal lymph nodes (≤5cm in diameter) were observed, prompting the performance of diagnostic and therapeutic splenectomy. Histologic study of the spleen showed a proliferation of small lymphoid cells, with a micronodular growth pattern, predominantly in the germinal centers of the white pulp, with infiltration of the red pulp. The cells had a CD20+, Bcl2+, Bcl6+, IgD− CD23−, cyclin D1− and p53− phenotype and a low proliferative index, findings which were consistent with the diagnosis of FL.
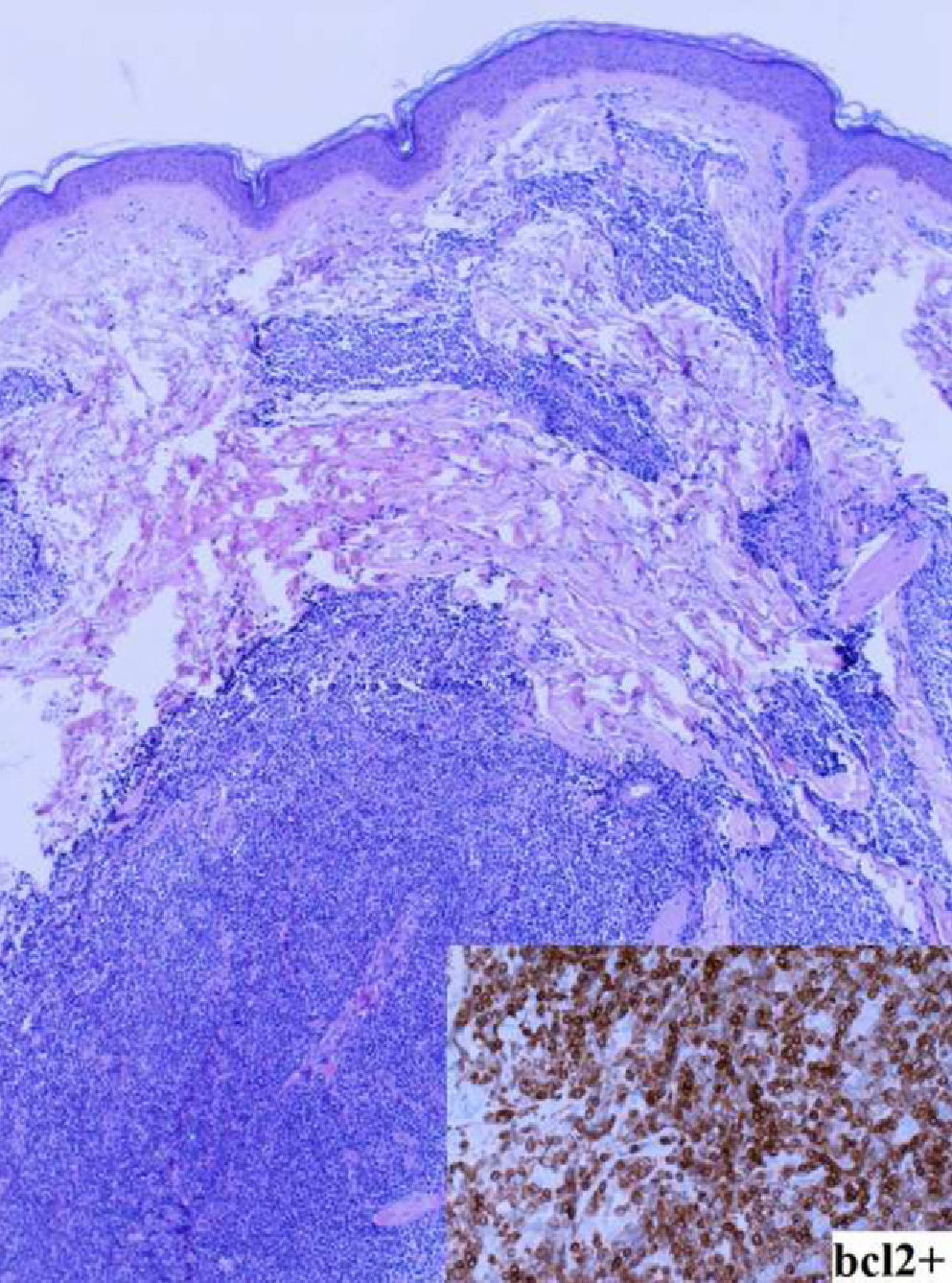
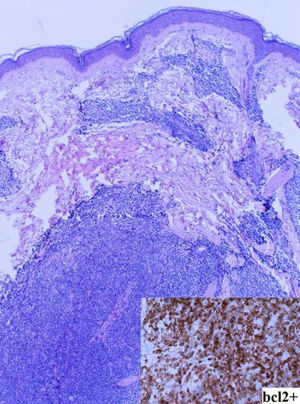
In March 2007, the patient was referred to the dermatology department due to the gradual appearance of asymptomatic subcutaneous nodular lesions on the face, chest and back. The nodules had an erythematous-violacious appearance, were slightly raised, and had diameters ranging between 8mm and 20mm (Fig. 1). Biopsy of the lesions showed a lymphoid infiltrate composed of small monomorphous cells, compatible with FL infiltration (CD20+, Bcl2+, Bcl6+) (Fig. 2). Reassessment of the disease at this time also demonstrated the development of lymphadenopathy, for which chemotherapy was started with a rituximab-CHOP schedule (cyclophosphamide, vincristine, adriamycin and prednisone). Complete remission was achieved after 6 cycles, with clearance of the subcutaneous nodules and the enlarged lymph nodes; subsequently, the patient was placed on maintenance therapy with rituximab administered every 3 months. In December 2009, the patient again presented with cutaneous lesions, predominantly facial, similar to those previously described; biopsy reconfirmed the diagnosis of infiltration by FL. The rituximab maintenance treatment ended in June 2010; the skin lesions were still stable and there was no evidence of disease spread to other areas (peripheral blood immunophenotyping and cervical-thoracic-abdomen CT scan were normal).
FL is characterized by an indolent course and has no standardized treatment; a variety of approaches are used, including simple observation, radiotherapy, immunotherapy, polychemotherapy, maintenance treatment with rituximab,3 and even the application of various hematopoietic stem cell transplantation treatment modalities.1
As in other lymphoid malignancies, patients with FL can have extranodal involvement affecting the skin in up to 3.8% of cases.4 Extranodal involvement in FL does not generally affect overall survival, unlike the case with large diffuse B-cell lymphoma; these 2 diseases constitute the majority of B-cell lymphomas in Spain.2 It is therefore important to rule out transformation of FL to more aggressive forms as these are associated with significantly decreased survival.4 For this reason, lesions should be biopsied whenever a patient experiences relapse or disease progression.
Differential diagnosis is particularly important in primary cutaneous follicular center lymphoma, since it shares histologic features with FL. In addition to systemic involvement, Bcl2 negativity, which is common in cases primarily involving the skin, may be of use in differentiating the 2 diseases.5
FL usually responds well to treatment, although relapses are common and usually affect the lymph nodes, bone marrow or peripheral blood.1,2 What is unusual is recurrence being limited to the skin, as in our patient. At present, and after more than 6 years of follow-up, the patient's disease remains limited to the skin. The persistence of cutaneous disease reflects a lack of complete control of the disease, and it is therefore likely that the patient will develop systemic disease in the future.
Please cite this article as: Palacios Abufón A, et al. Linfoma folicular sistémico con afectación cutánea y recidiva únicamente cutánea. Actas Dermosifiliogr. 2012;103:253–55.