Syphilitic alopecia occurs in only 4% of patients with syphilis. We present 5 cases of this uncommon manifestation and review the corresponding literature. All of the patients in our series were men aged between 31 and 46 years. The lesions, which were located mainly in the parieto-occipital area of the scalp, manifested as multiple, irregular, nonscarring patches of alopecia that adopted a characteristic patchy moth-eaten pattern. One patient initially presented diffuse alopecia with multiple erythematous scaling lesions. Immunohistochemical staining revealed the presence of numerous spirochetes in the hair follicles in the 2 patients in whom skin biopsy was performed. The lesions improved with treatment in all the patients who attended follow-up. Dermatologists should maintain a high level of clinical suspicion for this uncommon manifestation of syphilis, particularly when it is the only symptom.
La alopecia sifilítica es una manifestación infrecuente de la sífilis, que solo aparece en un 4% de los pacientes. Presentamos 5 casos de alopecia sifilítica y realizamos una revisión de la literatura. Todos los pacientes eran varones, con edades comprendidas entre los 31 y los 46 años. Las lesiones consistían en múltiples placas alopécicas de predominio en la región parietooccipital, irregulares, no cicatriciales, que adoptaban el característico patrón apolillado o en trasquilones. Un paciente comenzó con una alopecia difusa asociada a múltiples lesiones eritematosas y descamativas en el cuero cabelludo. En los 2 casos en que se realizó biopsia cutánea se detectó, mediante tinciones inmunohistoquímicas, la presencia de numerosas espiroquetas en el folículo piloso. Todos los pacientes en seguimiento clínico mejoraron sus lesiones tras el tratamiento. Los dermatólogos deben estar alerta ante esta manifestación infrecuente de la enfermedad, que todavía adquiere mayor relevancia clínica cuando aparece de forma aislada.
Syphilis, also known as the great imitator, has not been eradicated and physicians should maintain a high level of diagnostic suspicion.1 In addition to the usual forms of presentation, very rare cutaneous manifestations can appear and sometimes make diagnosis difficult.2
Syphilitic alopecia (SA) is an unusual manifestation of syphilis infection we should be familiar with, given the progressive rise in the number of cases of syphilis in Spain in recent years. This increase in the incidence of syphilis means we are more likely to see patients with atypical manifestations or with neurological complications in our routine clinical practice.1,2 We present 5 cases of SA and review the literature.
Case DescriptionsFor this study, we gathered all cases of SA diagnosed in the dermatology department of Hospital General Universitario de Valencia, Spain, between May 2007 and May 2011. Of a total of 81 patients diagnosed with syphilis, 57 had secondary syphilis. Alopecia was observed in 6.17% of all 81 cases of syphilis. The most relevant characteristics of the patients with SA are summarized in Table 1. All were men aged between 31 and 46 years and, on questioning, all reported high-risk sexual behavior. Serology was positive for reagin and antitreponemal antibodies in all patients, and 2 of them were also found to be positive for human immunodeficiency virus (HIV) infection, a new finding for case 1.
Characteristics in the 5 Cases of Syphilitic Alopecia.
| Case | Age, y/Sex | Sexual Behavior | Serology | Duration of the Alopecia | Associated Lesions | Type of Syphilitic Alopecia | Biopsy | Treatment | Follow-up at 3 Months |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 41/male | Homosexual | RPR 1/32TPHA (+)HIV (+) | 2 months | Papular-necrotic lesions on the trunkPalmoplantar lesions | Symptomatic SA | Spirochetesin the hair follicle | Three doses of penicillin G benzathine 2.4×106 IU | Clinical resolutionRPR 1/4 |
| 2 | 46/male | Homosexual | RPR 1/32TPHA (+)HIV (+) | 2 weeks | Fever and myalgiaUlcer on glans penisPalmoplantar lesionsRash on the trunk | Essential SAMoth-eaten pattern | Spirochetes in the hair follicle | Three doses of penicillin G benzathine 2.4×106 IU | Clinical resolutionRPR 1/2 |
| 3 | 40/male | Unknown | RPR 1/32TPHA (+)HIV (-) | 1 month | Oral ulcerPalmoplantar lesions | Essential SAMixed pattern | Not performed | Single dose of penicillin G benzathine 2.4×106 IU | Clinical resolutionRPR negative |
| 4 | 34/male | Heterosexual contactwith prostitutes | RPR 1/16TPHA (+)HIV (-) | Unknown | No | Essential SAMoth-eaten pattern | Not performed | Three doses of penicillin G benzathine 2.4×106 IU | Clinical resolutionRPR 1/4 |
| 5 | 31/male | Heterosexual | RPR 1/32TPHA (+)HIV (-) | 1 month | Ulcer on glans penisPalmoplantar lesionsRash on the trunk | Essential SAMoth-eaten pattern | Not performed | Single dose of penicillin G benzathine 2.4×106 IU | Unknown |
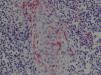
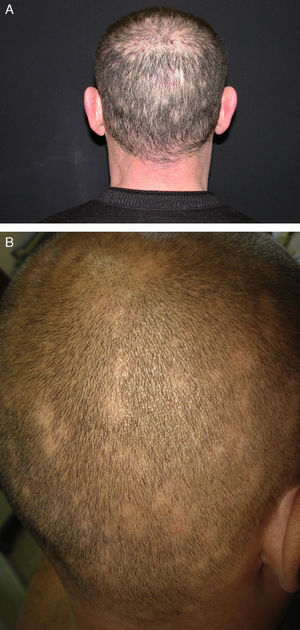
Physical examination revealed multiple plaques of nonscarring alopecia, predominantly affecting the parieto-occipital region. The plaques varied in size, did not present signs of inflammation or desquamation, and were not completely devoid of hair—they had the characteristic moth-eaten or patchy appearance (Fig. 1, A and B). One patient initially presented with diffuse alopecia associated with numerous desquamating erythematous lesions on the scalp (Fig. 2); after the first dose of antibiotic he developed a Jarisch-Herxheimer reaction with high fever, malaise, generalized joint and muscle pain, and marked worsening of the alopecia. On detailed questioning, the majority of patients reported other associated manifestations that could have suggested syphilis. Patient 4 had been completely unaware of the hair loss, and the diagnosis was made by chance; he presented no other symptoms of syphilis.
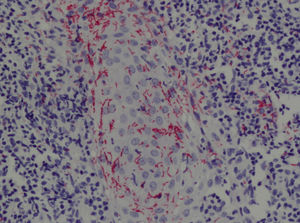
The skin biopsy in case 1 showed marked hyperkeratosis with areas of follicular keratosis and a diffuse granulomatous dermatitis with the presence of numerous plasma cells.
Histology in case 2 revealed irregular epidermal hyperplasia and a dense lymphohistiocytic inflammatory infiltrate with a lichenoid distribution that was prominent at the dermoepidermal junction. Immune staining showed the presence of numerous spirochetes with evident tropism for blood vessels and the perifollicular epithelium (Fig. 3).
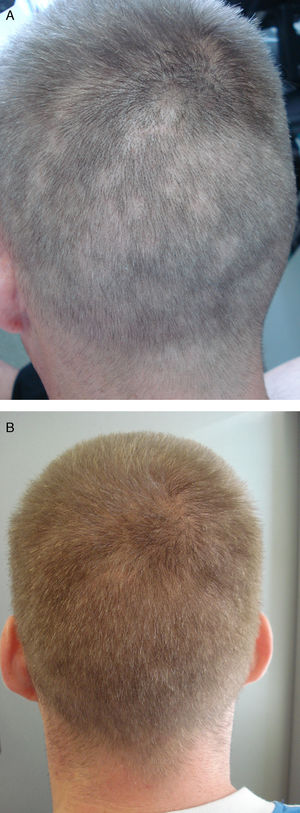
The patients who attended follow-up (cases 1 through 4) presented clinical improvement after the intramuscular administration of penicillin G benzathine, 2.4 million units (Fig. 4, A and B). It was decided to treat case 4 as syphilis of unknown duration and administer a weekly dose for 3 weeks. The serological response was adequate in all of the patients.
DiscussionSA is an unusual manifestation that only occurs in 4% of cases of syphilis.3 In 1940, McCarthy4 described 2 types of secondary SA, and that classification continues to be used, practically unchanged, to this day. Symptomatic SA is an extremely rare manifestation in which there are associated skin lesions on the scalp, usually in the form of papulosquamous lesions. The second type, essential SA, is characterized by hair loss with no other visible syphilitic lesions on the scalp. Essential SA has 3 distinct clinical patterns3,5,6:
Moth-eaten or patchy: This pattern is the most common and is characterized by the presence of small scattered plaques of nonscarring alopecia that are not completely hairless and show no signs of inflammation or desquamation. The plaques are irregular in size and have poorly defined borders. They occur mainly in the parieto-occipital region, possibly due to a greater load of treponemes because of the rich local blood supply to this area, but they can also arise in other areas of hairy skin, such as the beard, eyelashes, axillas, pubis, trunk, and even on the legs.
Diffuse: In this pattern, alopecia is diffuse, caused by widespread telogen effluvium-type hair loss, and there are no obvious plaques.
Mixed: Small, irregular plaques of alopecia develop on a background of diffuse alopecia.
The moth-eaten pattern is the most common form of presentation on the scalp and is considered one of the most characteristic signs of secondary syphilis.5,7 Other clinical entities (e.g., alopecia areata, trichotillomania, or tinea capitis) can also produce localized, nonscarring alopecia that clinically can mimic moth-eaten alopecia.3 In addition, syphilis must be included in the differential diagnosis when patients have rapid diffuse hair loss of unknown etiology.7 The diffuse pattern of SA can be considered a reactive phenomenon of the telogen effluvium type rather than a direct effect of the treponeme on the follicle. In primary syphilis, however, hair loss is very rare, and is only seen when the primary chancre occurs on the scalp. Scarring alopecia has been described in patients with tertiary syphilis.8
The different clinical forms of SA can be associated with systemic manifestations such as general malaise, low-grade fever, lymphadenopathies, asthenia, anorexia, and various mucosal and cutaneous manifestations, some of which are highly characteristics, such as a generalized nonpruritic papulosquamous rash predominantly affecting the trunk, palmoplantar lesions with Biett collarettes, ulceration of the oral mucosa, and condylomata lata. Less commonly, annular figurate plaques with central hyperpigmentation, granulomatous nodules and plaques, and the so-called corona veneris (numerous papules along the frontal hairline) may be observed.9
SA should be suspected when the typical lesions are present, possibly accompanied by other cutaneous or systemic manifestations; the diagnosis is confirmed by laboratory studies such as serology (reagin and antitreponemal antibodies), which is always positive in secondary syphilis.2,5 The histology of SA lesions usually shows preservation of the epidermis with areas of follicular hyperkeratosis. Psoriasiform epidermal hyperplasia with a lichenoid infiltrate has occasionally been reported.9 Other characteristic features are a marked reduction in the number of terminal hairs in anagen, associated with an increase in the number of hair follicles in telogen and catagen.10,11
According to Ackerman,12 SA should be classified as a nonscarring inflammatory alopecia with the presence of a perivascular and perifollicular lymphohistiocytic dermal infiltrate with plasma cells.9 A similar pattern can be observed in alopecia areata, but there is a series of findings that are highly suggestive of alopecia areata, such as the presence of miniaturized hair follicles, peribulbar eosinophils, and a honeycomb-pattern lymphocytic infiltrate.7,9,11 Recent molecular studies have identified Treponema pallidum in affected follicles, supporting the theory of a specific immunological reaction to the treponemal antigens.7 Immunohistochemistry can show the presence of spirochetes in the hair follicles, usually in the perifollicular and peribulbar regions, indicating that the treponeme has a direct pathogenic role in alopecia.13
The therapeutic approach to SA is identical to that for other patients with secondary syphilis.6 The treatment of choice in immunocompetent individuals is an intramuscular dose of 2.4 million units of penicillin G benzathine.3 In HIV-infected patients, weekly doses must be administered for 3 weeks.14,15 Greater hair loss, and even the possibility of telogen effluvium, have been reported secondary to a Jarisch-Herxheimer reaction after starting treatment (case 1).9 However, the hair loss is reversible and typically resolves completely within 8 to 12 weeks after treatment.3 It is important to initiate early treatment to avoid possible late complications, as the association between alopecia and cerebrospinal neurosyphilis has traditionally been assumed.4,5
SA may sometimes be the only manifestation of secondary syphilis,5,6 as in our case 4, and it is therefore important to maintain a high level of diagnostic suspicion in order to avoid a late or incorrect diagnosis. In patients with other skin manifestations, systematic examination of the scalp and other areas of hairy skin could reveal that SA is more common than is described in the literature and that it is underdiagnosed at the present time.
The dermatologist can play a very important role in the diagnosis of SA. Serological screening for syphilis, in addition to studies of thyroid hormones and antinuclear antibodies, must be performed in all cases of patchy or diffuse alopecia.5,7 We consider it important for dermatologists to be aware of this condition in order to correctly identify this type of alopecia and the other cutaneous manifestations as part of a single systemic disease, given that early treatment will lead to complete recovery and will prevent potentially serious complications.14,16,17
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Drs Javier López, Juan Vilata, Antonio Martínez, and Juan Ignacio Marí for their collaboration in some of the cases.
We would also like to thank Dr. Arantxa Torrijos for her critical reading of the article and her valuable corrections.
Please cite this article as: Hernández-Bel P, et al. Alopecia sifilítica: presentación de 5 casos y revisión de la literatura. Actas Dermosifiliogr. 2013;104:512–7.