Primary cutaneous diffuse large B-cell lymphoma, leg type (PCLBCL LT) accounts for approximately 20% of all primary cutaneous B-cell lymphomas and tends to present as infiltrated nodules, tumors, and plaques on the legs in the elderly. Unlike other primary cutaneous large B-cell lymphomas, it has a poor prognosis and tends to require treatment with systemic chemotherapy.
We present the case of an 82-year-old patient with a 1-year history of nodules and plaques on her right leg. Biopsy led to a diagnosis of PCLBCL LT and the lesions resolved without treatment within 1 month of the first visit. This is an atypical course of PCLBCL LT and we believe that it is the first such case to be reported in the literature.
El linfoma cutáneo primario difuso de células grandes-tipo pierna (LCPDCG-TP) representa aproximadamente el 20% de los linfomas cutáneos primarios de células B y suele presentarse como nódulos, tumores y placas infiltradas en las extremidades inferiores en las últimas etapas de la vida. A diferencia de otras entidades de este grupo se caracteriza por un pobre pronóstico, que suele requerir el uso de tratamiento quimioterápico sistémico.
Presentamos el caso de una paciente de 82 años con nódulos y placas en el miembro inferior derecho de un año de evolución, que fueron biopsiadas llegándose al diagnóstico de LCPDCG-TP y presentando, un mes después de la primera visita, resolución espontánea de las lesiones sin tratamiento. Se trata de un caso con un desarrollo atípico, siendo el primero publicado en la literatura con dicha evolución.
Primary cutaneous diffuse large B-cell lymphoma, leg type (PCLBCL LT) accounts for approximately 20% of all primary cutaneous B-cell lymphomas. It is more frequent after the sixth decade of life (mean age at onset, 76 years) and is slightly more common in women (ratio of women to men, 1.6).1 Clinically, it tends to present as nodules, tumors, infiltrated plaques, ulcers,2,3 and has even been reported to take the form of a migratory lesion.4 It mainly affects 1 or both legs (71.7%),1 although it can affect any part of the body. In contrast to other types of primary cutaneous B-cell lymphoma, PCLBCL LT has a poor prognosis, with a 5-year survival of 41%1; therefore, treatment is more aggressive and includes systemic chemotherapy, radiotherapy, and more recently, rituximab. Nevertheless, the advanced age of many patients can limit treatment options. Below, we present a case of PCLBCL LT that resolved spontaneously. We believe this is the first such case to be reported in the literature.
Case DescriptionThe patient was an 82-year-old woman who came to the dermatology department because of asymptomatic lesions on her right leg that had appeared gradually over the previous year. She did not have fever, weight loss, or any other systemic symptoms. Her personal history included hypertension, chronic atrial fibrillation, and 2 cerebrovascular accidents, the second of which had occurred 6 years previously. She had also undergone surgery for varicose veins (both legs) and placement of a prosthesis (right hip). She was receiving regular treatment with omeprazole, digoxin, torsemide, and acetylsalicylic acid. The initial examination revealed tumor lesions on the right leg. These were of rubbery consistency and measured up to 2cm in diameter (Fig. 1). No lesions were visible on the rest of her skin, and no enlarged lymph nodes were detected in the groin, armpits, face, or neck.
Histopathology of a skin biopsy specimen revealed a diffuse dermal infiltrate that was separated from the epidermis by a band of normal collagen (Grenz zone) and extended into the hypodermis. The infiltrate was composed of mainly centroblast-like and immunoblast-like neoplastic cells and a few smaller cells with characteristics of mature lymphocytes (Fig. 2). In the immunohistochemical study, the neoplastic cells stained positive for CD20, CD79a, bcl-2, bcl-6, and MUM-1 (the last 2 with less intensity) and negative for CD10, CD21, and CD30. The Ki-67 proliferation index was approximately 90%. The small cells were positive for CD3 (Fig. 3). The result of in situ hybridization for Epstein–Barr virus (EBV)–encoded small RNA was negative. Polymerase chain reaction (PCR) did not reveal clonal rearrangement of the immunoglobulin (Ig) heavy chain CDR3 region and Ig κ light chain. PCR of the T-cell receptor γ chain gene was not performed, since the T cells present were thought to be associated with the neoplastic B cells.
A, Diffuse dermal infiltrate separated from the epidermis by a normal collagen band (Grenz zone) and marked involvement of the hypodermis (hematoxylin-eosin, original magnification ×4). B, Higher magnification shows that the infiltrate is composed of a proliferation of centroblast-like and immunoblast-like neoplastic cells, together with several smaller cells with the characteristics of mature lymphocytes (hematoxylin-eosin, original magnification ×60).
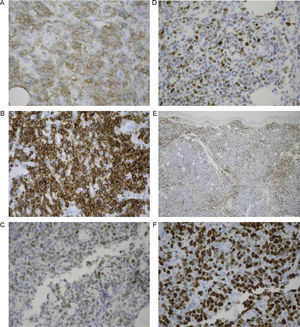
A, Neoplastic cells, which were the main component of the infiltrate, were positive for CD20 (IHC, original magnification ×40). B, Neoplastic cells were intensely positive for bcl-2 (IHC, original magnification ×40). C, Expression of bcl-6 in the neoplastic cells composing the infiltrate (IHC, original magnification ×40). D, Expression of MUM-1 (IHC, original magnification ×40). E, Small accompanying cells were positive for CD3 (IHC, original magnification ×4). F, Marked Ki-67 expression with an estimated proliferation index of 90% (IHC, original magnification ×40). IHC indicates immunohistochemistry.
Suspicion of a lymphoproliferative disorder prompted us to rule out visceral or lymph node involvement. The results of the biochemistry study were unremarkable, even for lactate dehydrogenase, β2-microglobulin, and immunoglobulins; similarly, no alterations were found in the complete blood count, protein electrophoresis, peripheral blood smear, or peripheral blood immunophenotyping. Serology testing for viruses (human immunodeficiency virus, hepatitis B and C virus, and human T-lymphotropic virus 1 and 2) and Borrelia burgdorferi was negative; testing for EBV and cytomegalovirus IgG was positive. Bone marrow biopsy and immunophenotyping were also performed, although neither revealed evidence of malignancy. Whole-body computed tomography revealed the presence of multinodular goiter and an image that was compatible with an enlarged lymph node or peritoneal implant in the right iliac fossa.
PCLBCL LT was diagnosed and the patient was re-evaluated. At 4 weeks from the first visit, the skin lesions had almost completely disappeared, with only what seemed to be residual erythematous-brownish macules remaining (Fig. 4). A second skin biopsy revealed a diffuse infiltrate composed of mature T cells (CD3+) with scant foci of atypical cells expressing CD20 and bcl-2 (Fig. 5), findings that were consistent with almost complete regression of the previous lymphoproliferative disorder. Biopsy of the peritoneal lymph node was ruled out owing to the patient's age, baseline situation, and, essentially, the clinical course of the skin lesions.
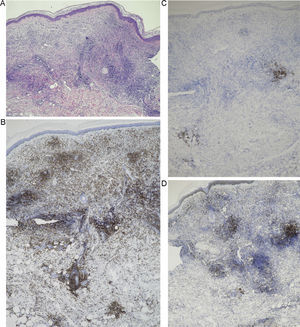
A, Diffuse infiltrate composed of mature T cells with scant foci of atypical cells (hematoxylin-eosin, original magnification ×4). B, Expression of CD3 cells in most of the infiltrate (IHC, original magnification ×4). C, Persistence of foci of CD20+ cells corresponding to atypical cells (IHC, original magnification ×4). D, Persistence of foci of bcl-2+ cells corresponding to atypical cells (IHC, original magnification ×4). IHC indicates immunohistochemistry.
In view of the patient's progress, we opted for close monitoring of the patient, who remained in clinical and laboratory remission until she died of a third cerebrovascular accident 4 months later.
DiscussionSelf-resolving malignant lymphoproliferative disorders are well documented in the medical literature. Probably the most representative group is cutaneous CD30+ lymphoproliferative disorders, which belong to the primary cutaneous T-cell lymphoma group and comprise lymphomatoid papulosis and CD30+ anaplastic large-cell lymphoma (ALCL).
Lymphomatoid papulosis presents as asymptomatic papules, which are frequently ulcerated. They are also self-limiting and recurrent and often heal leaving a superficial scar. However, given that this condition usually resolves spontaneously after months or years, treatment tends to be conservative.5,6 Notwithstanding, long-term follow-up is recommended owing to the risk of a new lymphoma before, after, or concurrently with lymphomatoid papulosis (approximately 19% depending on the series6).
CD30+ ALCL manifests as solitary or localized nodules or tumors, although they can be multifocal in up to 20% of cases. Complete or partial spontaneous remission is observed in up to 42% of cases, although recurrence is common. Standard treatment options include radiotherapy and excision for localized forms and systemic methotrexate for multiple lesions.5 Zayour et al.7 recently proposed the existence of a new subtype of CD30+ cutaneous lymphoproliferative disease characterized by 1 or a few nodules in which the most remarkable histopathology finding is pseudoepitheliomatous hyperplasia and an infiltrate of atypical CD30+ cells similar to those present in CD30+ ALCL. The authors found that the disease tended to resolve spontaneously, more so than in conventional CD30+ ALCL and with a more favorable prognosis.
Spontaneous remission of other conditions is exceptional, however, particularly in the case of aggressive lymphomas. Isobe et al.8 reported the case of a patient with extranodal natural killer (NK)/T-cell lymphoma who had undergone treatment with radiotherapy and CHOP (cyclophosphamide, hydroxydaunorubicin, vincristine, and prednisone). Nine months after treatment he developed nodal recurrence that remitted spontaneously during the following 2 months.
In transplant patients on immunosuppressive treatment, there is a greater incidence of infection and premalignant and malignant disease, including cutaneous T-cell lymphoma, and, more particularly, cutaneous B-cell lymphoma. Treatment for these conditions, which includes chemotherapy, radiotherapy, and surgery, is not well defined; however, remission can sometimes be achieved by simply reducing or switching immunosuppressive treatment.9,10 Patients with human immunodeficiency virus infection are in a similar situation, especially those in more advanced stages, where the risk of non-Hodgkin lymphoma is greater than in the general population. Although the behavior of these lymphomas is usually aggressive, highly active antiretroviral therapy has led to complete remission in some cases.11
The findings for the diseases cited above are neither clinically nor histologically similar to those of the case we report. The differential diagnosis in cases like ours should also include pseudolymphoma, which comprises a series of cutaneous lesions with lymphoid proliferation that are clinically and histologically similar to lymphoma. Although the etiology is uncertain in most cases, there have been reports of cases associated with insect bites and stings, infections, tattoos, vaccines, contact reactions, and medication. In contrast to the case we report, B-cell pseudolymphomas are found mainly on the trunk and upper extremities and usually mimic low-grade cutaneous lymphomas (the present case was high-grade). The presence of a clonal population is not common in pseudolymphomas, although it can point to a proliferation of malignant lymphoid cells. We did not observe monoclonal rearrangement because of the marked accompanying T-cell infiltrate, which was particularly manifest in the second biopsy specimen. Given the clinical and histological course of the disease, we think that the infiltrate could have contributed to the regression of the malignancy, as suggested by Isobe et al.8 in their patient with extranodal lymphoma of NK/T cells.
In conclusion, we have presented the case of a patient with PCLBCL LT that progressed atypically before regressing spontaneously. To our knowledge, this is the first report of spontaneous regression in a cutaneous B-cell lymphoma with poor prognosis.
Ethical DisclosuresProtection of Human and Animal SubjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to Privacy and Informed ConsentThe author obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alcántara-González J, González-García C, Fernández-Guarino M, Jaén-Olasolo P. Linfoma cutáneo primario difuso de células grandes-tipo pierna con regresión espontánea. Actas Dermosifiliogr. 2014;105:78–83.