Melanocytic neoplasms with spitzoid morphology (Spitz nevi, atypical Spitz tumors, and spitzoid melanomas) may be benign or malignant. Because the malignant potential of atypical Spitz tumors is uncertain, the proper therapeutic approach has been much debated over the years. Promising new techniques for molecular analysis have enabled better predictions of the biological behavior of these tumors. We review their cytogenetic features and prognosis and also provide an update of the most recent recommendations for management.
Las neoplasias melanocíticas con morfología spitzoide (nevus Spitz, tumor de Spitz atípico y melanoma spitzoide) abarcan un espectro desde lesiones benignas a malignas. Debido al potencial maligno incierto de los tumores de Spitz atípicos el abordaje terapéutico ha generado durante años controversia. El desarrollo de nuevas técnicas moleculares parece prometedor y ha contribuido a una mejor predicción del comportamiento biológico de los tumores de Spitz. Nuestro objetivo es revisar las características citogenéticas de los tumores de Spitz, el pronóstico y actualizar las últimas recomendaciones de manejo.
Over the last few decades, the molecular features of Spitz nevi have been studied closely with the aim of determining patterns that may help distinguish these lesions from melanoma and of characterizing the malignant potential of atypical Spitz tumors.
Comparative genomic hybridization revealed initially that some mutations present in melanoma (copy number gains on chromosomes 1q, 6p, 7p, 8q, 17q, 20q and losses on chromosomes 6q, 8p, 9p, and 10q) were not present in benign melanocytic nevi.1 With fluorescence in situ hybridization (FISH), it has been demonstrated that between 12% and 20% of Spitz nevi have amplifications on chromosome 11p.2
The copy number gains of the HRAS gene, located on chromosome 11p, gives rise to spitzoid tumors with similar characteristics to melanoma (larger size, mainly dermal localization, desmoplasia, and infiltrating growth). In absence of additional genetic mutations, these tumors show benign behavior with limited proliferative activity.3–8 Unlike melanomas, Spitz nevi do not harbor BRAF and NRAS mutations, but they may carry HRAS mutations (15–30%). These mutations may also be present with lower frequency in atypical Spitz tumors (10%).3,9–11
Subsequently, a set of sporadic atypical Spitz tumors were discovered known as Wiesner nevi or BAPomas, associated with somatic mutations in BAP1 (tumor suppressor gene located on chromosome 3p21), often in combination with the p.V600E mutation in BRAF.12–14 Mutations in BAP1, when they affect the germline, lead to a predisposition to multiple Spitzoid melanocytic tumors within the BAP1 tumor syndrome15; this syndrome links malignant tumors with cutaneous melanoma, uveal melanoma, mesothelioma, clear cell renal carcinoma, meningioma, and lung adencarcinoma.16
Clinically, BAPomas are usually, well defined and occasionally pedunculated dome-shaped tumors with a smooth surface, and a color varying from that of normal skin color to a brown or reddish hue. They are usually manifest as multiple lesions located on the trunk, with a mean size of 5 mm. Given their appearance, they may be confused with Miescher nevi. Pathology study reveals a principally dermal tumor consisting of epithelioid melanocytes with abundant cytoplasm, enlarged nuclei with vesicular chromatin, and conspicuous nucleoli, with or without associated lymphocyte infiltrate. They are generally not pigmented. They show similar cytological features to Spitz nevi; however, certain features are lacking such as epidermal hyperplasia, hypergranulosis, Kamino bodies, spindle-shaped melanocytes, and clefting around junctional melanocytes.12–14BAP1 mutation correlates with loss of nuclear expression of BAP1, identified through immunohistochemistry.12 The importance of recognizing these lesions lies in their possible genetic implications within the syndrome of predisposition to tumors associated with BAP1 mutations.15,16
Mutations have been detected in the promoter of telomerase reverse transcriptase (p-TERT) in most melanomas in children, including spitzoid melanoma, and in 22–71% in adults. It has been suggested that tumors without this mutation have a more favorable prognosis than carriers of the p-TERT mutation, which have a more aggressive behavior.17
ROS1, NTRK1, ALK, BRAF, and RET fusion kinases are present in 55% of Spitz nevi, 56% of atypical Spitz tumors, and 39% of spitzoid melanomas.18 The presence of these translocations does not appear to be associated with a higher incidence of aggressive disease.17,19 Spitz tumors with ALK translocations usually present as isolated, dome-shaped lesions, generally located on the limbs. They are usually amelanotic and, less frequently, pigmented. Pathology study shows plexiform fascicles of spindle-shaped melanocytes in the dermis, and these express ALK in histochemical study.18,19
Gerami et al.5 proposed using FISH to detect the copy number of the genes RREB1 (6p25), MYB (6q23), and CCND1 (11q13) and of centromere 6 (Cep 6). The absence of these abnormalities is suggestive of Spitz nevi, whereas the presence of chromosomal abnormalities points to diagnosis of melanoma and some atypical Spitz tumors with an aggressive behavior,20 with a sensitivity of 86.7% and a specificity of 95.4%.5 An analysis by age groups revealed a larger number of false positives in children.21 Subsequently, it was proposed to use CDKN2A (9p21), RREB1 (6p25), CCND1 (11q13), and MYC (8q24), given their greater specificity for detecting spitzoid lesions.22
In a case-control study that analyzed the aggressive behavior of atypical spitzoid tumors, on stratifying risk by FISH results, it was found that cases with isolated 6q23 deletion were low risk, whereas the presence of chromosomal abnormalities such as copy number gains on 6p25 or 11q13 had an intermediate risk; in contrast, loss of homozygosity in 9p21 was associated with an aggressive behavior.23 Lee et al.19 also evaluated the FISH results and the frequency of aggressive tumor behavior in a cohort of atypical spitzoid neoplasms in the pediatric population. The authors estimated that at least 25% of children with atypical spitzoid neoplasms with homozygous deletions on 9p21 had recurrence after complete excision and fewer than 12.5% had distant metastasis.
Mass spectrometry imaging, a new method recently used for differential diagnosis of spitzoid lesions, identifies a molecular signature that enables specific diagnosis through a distinctive combination of between 5 and 20 proteins. Lazova et al.24 showed, through identification of a combination of 5 peptides, that there are proteomic differences between Spitz nevi and spitzoid melanoma; the authors suggest that use of this combination could provide useful information for evaluating the risk of atypical Spitz tumors.
In a study in which the exome of 77 melanocytic lesions was sequenced (Spitz nevus, spitzoid melanomas, and benign melanocytic nevi), it was observed that MEN1, PRKAR1A, and DNMT3A mutations in spitzoid melanomas may indicate participation of the protein kinase A pathway or a role for DNA methylation.25 The authors highlight that the somatic mutation load is lower in conventional nevi and in Spitz nevi compared with conventional melanoma and spitzoid melanoma.
Molecular techniques are promising complementary tools for histologic evaluation of tumors with an unknown malignant potential. Currently, although they appear to contribute to a more accurate prediction of biological behavior, there may be times when the genetic profiles overlap, and so their predictive value is still unknown. The cost and limited availability—these techniques are for the most part restricted to research centers—have hindered their use in everyday clinical practice.26
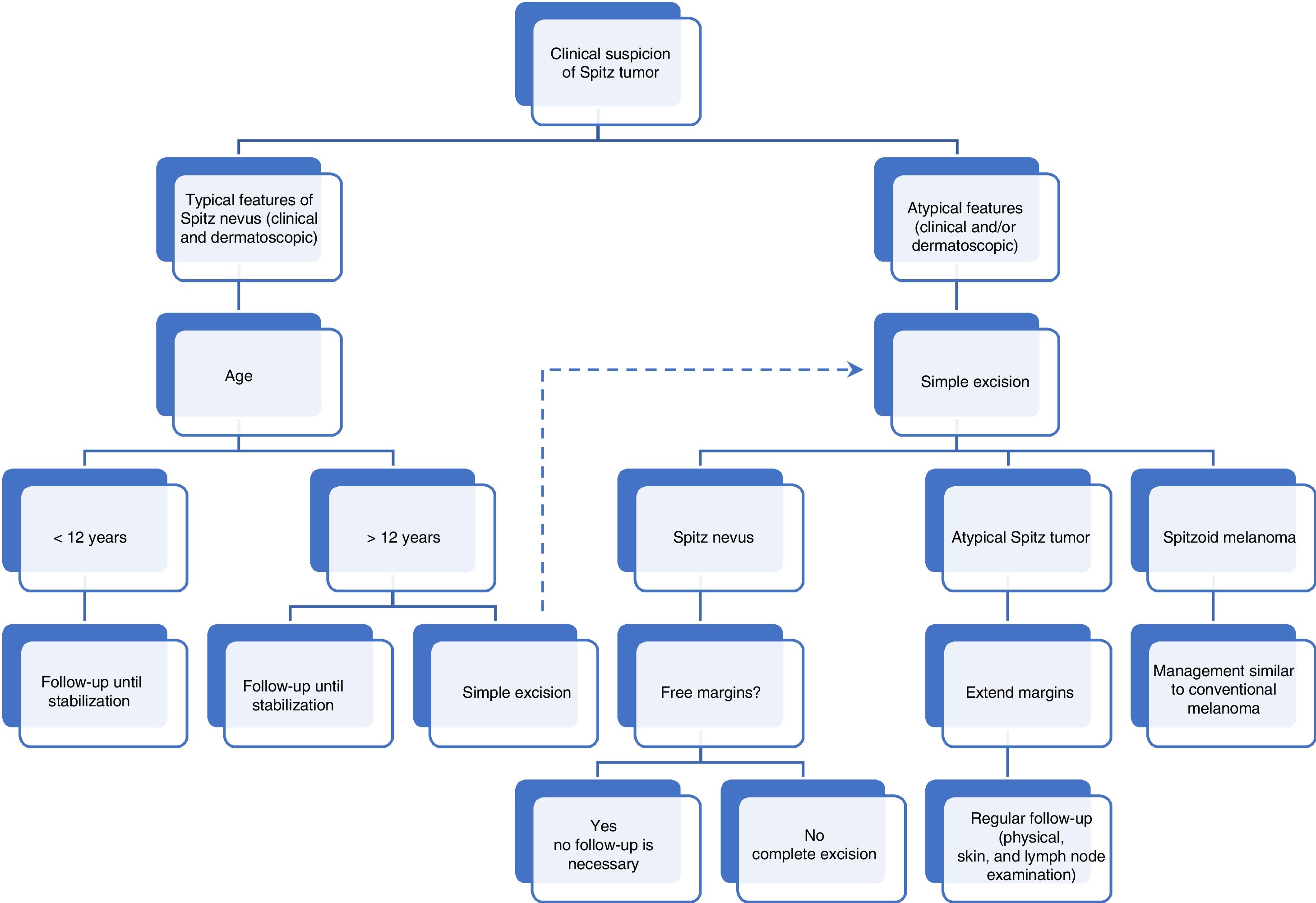
Prognosis and managementSpitz nevusThere is no established consensus for management of spitzoid tumors. Some authors suggest excising all such lesions, including classic Spitz nevi, given their occasional resemblance to melanoma.27 However, conventional Spitz nevi are completely benign and recently, it has been reported that up to 80% of lesions undergo spontaneous involution or conversion to another more common type of melanocytic nevus.28 Cases of Spitz nevi with metastasis have been considered as diagnostic errors and have retrospectively been diagnosed as melanomas.29 However, melanoma is very uncommon in children.30 In a study conducted by Lallas et al.,31 based on a cohort of 384 patients aged 12 years or more with lesions showing spitzoid features, the authors reported a risk of melanoma of 13.3%. This risk increased significantly with the age of the patient, with an equal probability of the lesion being a nevus or melanoma from 50 years onwards. The authors also suggested that a spitzoid pattern in dermatoscopy is predictive of melanoma in patients aged 70 years. For this reason, when faced with conventional Spitz nevus in a child, in particular those under 12 years, with no atypical clinical or dermatoscopic features, the recommendation is for regular clinical follow-up only.32 Nino et al.33 proposed follow-up every 6 months for the first 2–3 years and then once a year. Furthermore, in this age group, the lesions were often located in visible areas and, therefore, a more conservative approach may avoid possible sequelae, such as ugly scars after excision of a benign lesion. Given that the incidence of melanoma increases with age, it is understandable that excision is performed more frequently in adults.
In a recent update to management of spitzoid lesions, the recommendation is for complete surgical excision after 12 years for lesions without any atypical features (Tables 1 and 2, Part 1) or, alternatively, digital monitoring until stabilization.32 Excision should be considered in all spitzoid tumors with atypical clinical or dermatoscopic features, regardless of the age of the patient.32,33 In view of the finding in a previous study that showed that nodular lesions are more likely to be melanomas than flat superficial lesions (32% vs 12%, respectively),32 the following is recommended:
- a)
In those clinically typical lesions with a nodular appearance, excision should be performed or, alternatively, clinical and dermatoscopic monitoring indicated. This monitoring initially should be performed after 15 days and then, if no changes are detected, at 4 and 8 weeks, until 6 months without any growth or—if the lesions is involving—until disappearance, when follow-up can be stopped. If growth is detected between visits, excision is recommended.32
- b)
For clinically typical flat lesions, follow-up is recommended every 2–3 months; lesions with a starburst or globular pattern in dermatoscopy, punctiform vessels, or natural changes resulting from the sequential progression usually seen in Spitz nevi are not considered cause for alarm, until the lesion acquires the appearance of a conventional nevus or until its involution. As for lesions with a nodular appearance, monitoring should continue until 6 months have passed without any growth.32 Recently, the authors of the aforementioned clinical guideline have proposed a modification: after arguing that no cases of melanoma or atypical Spitz tumors have been detected after an initial symmetric starburst pattern, they now suggest that further actions are not required, or just follow-up, even if subsequent asymmetric changes occur.34
There are still doubts about the malignant potential of atypical Spitz tumors. It is thought that these lesions constitute a heterogenous group with different biological behavior, for the most part benign with only a small percentage constituting melanomas.35 In these cases, faced with the uncertainty of whether or not to follow the protocol for treatment of conventional melanoma, Kelley and Cockerell36 proposed assessing sentinel lymph node status as a diagnostic method in case of doubt for lesions with a thickness of 1.0 mm or more. As for conventional melanoma, these authors considered the presence of melanocytes with cytological atypia in the parenchyma or subcapsular space of the lymph node as indicative of metastatic disease. Subsequently, it has been observed that lymph nodes are more frequently involved in atypical Spitz tumors than in conventional melanoma in adults (38–39% vs 10–16%, respectively).35,37 Ludgate et al.38 observed a positive sentinel lymph node rate of 47% in a cohort of 67 patients with atypical Spitz tumors. Despite this high incidence, no patients with a positive finding in selective lymph node biopsy (SLNB) showed recurrence and all were disease-free after a mean follow-up of 3.6 years. Furthermore, the authors found that younger age was significantly associated with a higher rate of lymph node positivity but with a better prognosis, as also reported to date for melanoma.39 These results show that perhaps a positive sentinel lymph node might not be as significant in determining the malignant potential of atypical Spitz tumors as previously thought.26 However, the authors proposed that a consensus should be sought with the patient after explaining the risks and benefits of SLNB for atypical Spitz tumors.38
With the aim of avoiding unnecessary aggressive diagnostic and therapeutic procedures, in a systematic review that included 541 patients with atypical Spitz tumors, Lallas et al.35 assessed the role of SLNB as a prognostic method in the treatment of these patients. The review included 303 patients who underwent SLNB; of these 119 (39%) were positive. It was observed that the majority of patients with atypical Spitz tumors had favorable clinical outcomes: 99% of those with positive SLNB did not present with spread beyond the lymph node after 5 years, whereas 32%–37% of patients with conventional melanoma and positive SLNB had disease progression at 3 years.40 Of the group of 541 patients with atypical Spitz tumors, only 5 (<1%) had local recurrence during follow-up: 2 of among 238 who had undergone wide local excision without SLNB, 2 of 184 patients with a negative finding in SLNB, and 1 of 119 patients with positive SLNB.35
The presence of melanocyte aggregates in the lymph nodes does not have the same significance as in melanoma41; thus some benign melanocytic proliferations such as blue nevi,42 congenital and acquired nevi,43 and by analogy some Spitz nevi, may show deposits in the lymph nodes due to a process of migration of benign melanocytes from the nevus.
A series of 24 children with atypical Spitz tumors who underwent complete excision of their lesions without SLNB found all patients to be disease free after a mean follow-up of 3 years.44 Therefore, there does not seem to be any evidence to support SLNB in patients with atypical Spitz tumors, as the procedure is associated with a certain degree of morbidity and there is no improvement in prognosis.35,38,44
Although there have been no studies of optimal margins, using the Melanoma Pathology Assessment and Treatment Hierarchy (MPATH-Dx) evaluation tool, based on a reporting scheme for melanocytic melanomas, Spitz nevi were included as category 2, implying that excision should be with a margin of <5 mm. Atypical Spitz tumors are considered as category 3, that is, there should be a margin of 5–9 mm. Melanomas are included in category 3 or 5, and require wide excision with a margin ≥1 cm.45 However, the recommendation of many authors for atypical Spitz tumors it to perform a wide excision, and the margins most widely used are those of 1 cm.26,35,38 Likewise, there is consensus about monitoring for excised atypical Spitz tumors; the most recent recommendations include regular clinical follow-up at least once a year for 3 years, with lymph node ultrasound in case of swollen lymph nodes.32,35Fig. 1 summarizes the algorithm for management of spitzoid tumors.
In conclusion, spitzoid lesions are a challenge both in terms of diagnosis and clinical management. Integration of the form of clinical presentation, pathology findings, immunohistochemical expression patterns, dermatoscopy, and new molecular genetics techniques can help us to clarify the malignant potential of atypical Spitz tumors. We should not forget that melanoma is uncommon in childhood, and so the age of the patient is one of the most important factors to account for.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sainz-Gaspar L, Sánchez-Bernal J, Noguera-Morel L, Hernández-Martín A, Colmenero I, Torrelo A. Nevo de Spitz y otros tumores spitzoides en la infancia. Parte 2: características citogenéticas y moleculares. Pronóstico y tratamiento. Actas Dermosifiliogr. 2020;111:20–25.