A 11-year-old girl presented with a 3cm slow-growing lesion on the right iliac region since birth. She reported intermittent episodes of pain, bleeding, and swelling. The patient was otherwise healthy, and no family member exhibited such anomalies.
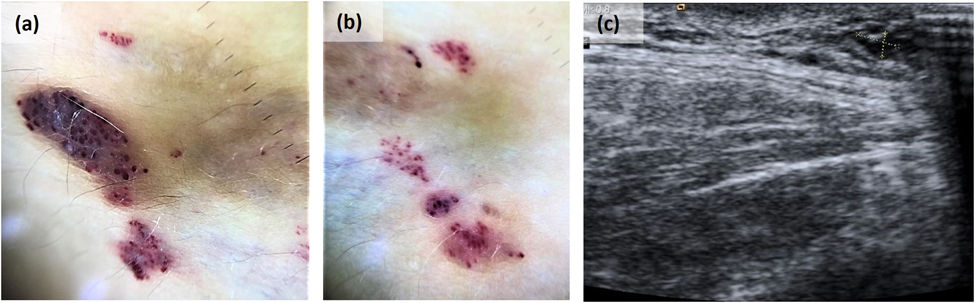
Physical examinationPhysical examination revealed the presence of a localized tumor composed of scattered aggregates of small translucent yellowish, reddish, and dark reddish vesicles and papules that occasionally bled and oozed serosanguinous fluid (Fig. 1).
Additional testsDermoscopy of the dark reddish vesicles showed dark red/bluish lagoons while the dermoscopy of the translucent vesicles revealed light brown lacunas surrounded by paler septa, focal reddish areas, and hypopyon-like features (Fig. 2a and b). Doppler ultrasound revealed a 3mm slight thickening of subcutaneous tissue composed of millimetric cystic structures without a Doppler signal inside, which was consistent with a slow-flow vascular malformation (Fig. 2c).
Dermoscopy and ultrasound images. (a) Dermoscopy of the dark reddish vesicles showed dark red/bluish lagoons. (b) Dermoscopy of the translucent vesicles showed light brown lacunas surrounded by paler septa, focal reddish areas, and hypopyon-like features. (c) Doppler ultrasound revealed a 3mm slight thickening of subcutaneous tissue, composed of millimetric cystic structures without a Doppler signal inside consistent with a slow-flow vascular malformation.
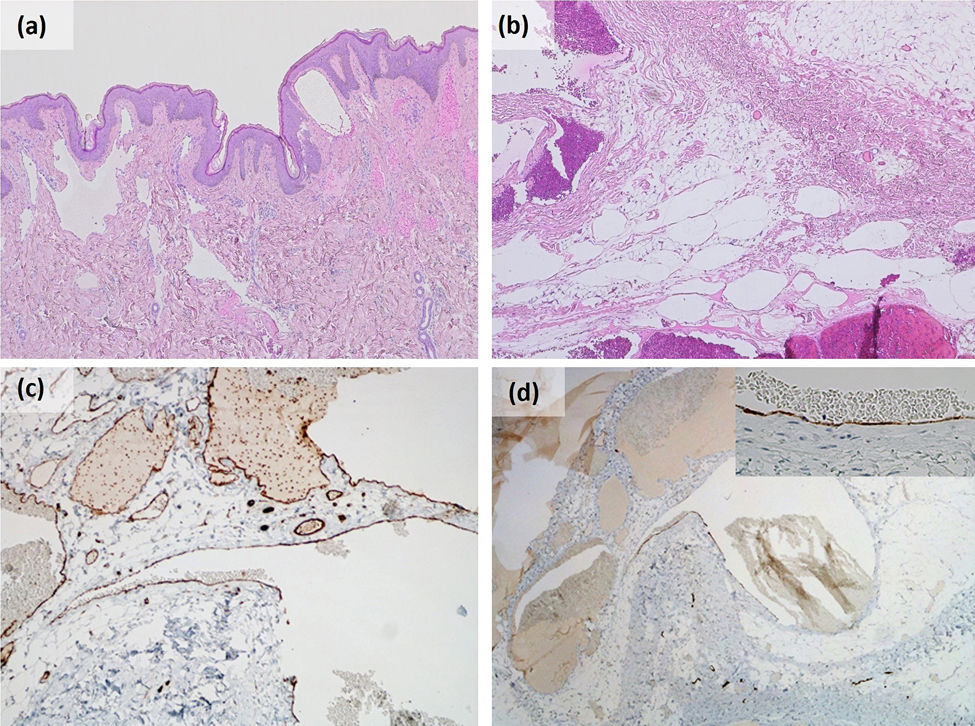
Histopathology showed dilated thin-walled lymphatic vessels of variable size on the superficial dermis and hypodermis, positive for CD31 and CD34, focally positive for podoplanin D2-40, and negative for epithelial markers and WT-1 (Fig. 3).
Histological examination revealed the presence of a benign vascular proliferation composed of irregular dilated vascular channels of variable size in dermis and hypodermis. Vascular structures are mostly thin endothelium-lined channels (c) positive for CD31 and focally positive for (d) podoplanin D2-40 with no supporting stroma. (a and b) Haematoxylin and eosin, original magnification (a) 40×; (b) 100×; (c) CD31 100×; (d) podoplanin D2-40 100×.
What is your diagnosis?
Cutaneous microcystic lymphatic malformation.
Course of the disease and treatmentDue to the presence of intermittent episodes of pain and bleeding, a pulsed dye laser was used on the superficial hemorrhagic components of the lesion with posterior surgical excision of the lesion, which turned out uneventful. No lesion recurrence has been reported at the 18-month follow-up.
CommentCystic lymphatic malformations are rare low-flow congenital vascular malformations resulting from abnormal embryologic development of lymphatic vessels that can affect the viscera, soft tissues, and/or skin.1 According to the International Society for the Study of Vascular Anomalies, they are now categorized based on the size of each cyst as microcystic, macrocystic, and mixed cystic.1,2
Lymphatic malformations (LM) can occur as an isolated finding or as a part of syndromes such as Turner syndrome, Noonan syndrome, Klippel–Trenaunay syndrome, and Down syndrome.1 Recently, somatic activating mutations in the phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) gene have been reported in many patients with LM in the endothelial cells lining the malformed lymphatic vessels.1
Cutaneous microcystic lymphatic malformations occur at birth or during infancy or early childhood. They present as clusters of translucent vesicles to flesh-colored papules that may become purple or black in the presence of bleeding. The surface of the lesions may exhibit warty hyperkeratosis. These lesions are usually found on the buttocks, inguinal region, axillary folds, proximal extremities, and oral cavity. The most common complications are oozing, bleeding, pain, swelling, and secondary infection.3
Dermoscopy shows the presence of a lacunar/saccular pattern. Lesions containing clear fluid dermoscopically show light brown lacunae surrounded by pale septas. The different amounts of blood inside the lagoons cause focal reddish areas, diffuse pink coloration, reddish/violaceous/bluish lacunar structures, and/or hypopyon-like features.4
Histopathology is characterized by acanthosis and papillomatosis of the epidermis with numerous dilated lymphatic channels on the upper dermis, which may often extend to the lower dermis and even to subcutaneous tissue. The lymphatic endothelial marker podoplanin D2-40 highlights the channels. More reliable markers for lymphatic endothelium are prospero-related homeobox-1 (Prox-1), lymphatic vessel hyaluronan receptor-1 (LYVE-1), and vascular endothelial growth factor receptor 3 (VEGFR3), but they are rarely available.5
The treatment of microcystic lymphatic malformations is challenging due to soft tissue infiltration by micro-lymphatic channels that cannot be visualized well with current imaging modalities. Although there are no clinical practice guidelines for the management of these malformations, surgical excision is often considered the first-line therapy and has been reported to cure 75% of cutaneous lymphangiomas. Other therapeutic modalities can be chosen based on location, extension, and symptoms, such as sclerotherapy, radiofrequency ablation, carbon dioxide laser, long-pulsed Nd-YAG laser, pulsed-dye laser, cauterization, and cryotherapy with variable outcomes. Finally, sirolimus – a potent inhibitor of mTOR – is truly promising in the treatment of LM.2,3,6
Informed consentThe patient in this manuscript has given written informed consent to the publication of their case details.
FundingThis research has not received specific aid from agencies of the public sector, commercial sector or non-profit entities.
Conflict of interestThe authors have no conflicts of interest to declare.
AcknowledgmentsWe thank the patient for providing his written consent for using clinical photographs.
We thank Rodrigo Carvalho, MD, from the Dermatology Department of Centro Hospitalar Lisboa Central, for the patient's initial assessment and skin biopsy performance.
We thank André Pinto, MD of the Plastic and Reconstructive Surgery Service of Centro Hopitalar Lisboa Norte, for the surgical excision of the lesion.
We thank Katarína Kieselová, MD, from the Dermatology Department of Centro Hospitalar Garcia de Orta, for providing the dermoscopy images.
Data availabilityData sharing is not applicable to this article as no new data were created or analyzed in this study.