Skin cancer prevention and detection campaigns targeting specific groups are necessary and have proven to be more effective than those aimed at the general population. Interventions in outdoor tourist spots have proven successful, although none have specifically targeted golf courses. The aims of this study were to describe the risk profile of golfers and golf course workers and evaluate the impact of a skin cancer prevention and early detection intervention.
Material and methodsThis was a cross-sectional descriptive study conducted at 6 golf courses. The intervention included a skin examination and completion of a questionnaire about demographic details, risk factors, and sun exposure and sun protection habits. Participants were also given advice on sun protection measures, self-examination, and use of sunscreens, and were asked about their satisfaction with the intervention and their intention to change their current behaviors. The effect was measured in terms of the diagnoses made, satisfaction with the intervention, reported intention to change, and potential effect in terms of existing risk factors.
ResultsOf the 351 participants (57% golfers and 43% golf course workers), 70.4% had fair skin, 11.7% had a family history of skin cancer, and 8.5% had a personal history of skin cancer. Skin cancer and actinic keratoses were diagnosed in 10.7% and 40% of the golfers, respectively. The session was rated positively by 99.4% of the participants; 93.9% stated that they intended to improve their sun exposure habits and 93.4% said that they planned to examine their skin more frequently.
ConclusionsOur findings confirm that golf course workers and, in particular, golfers are an important target for skin cancer prevention campaigns. This is the first intervention to specifically target golf courses, and it proved to be both feasible and useful. Its success appears to be attributable to numerous factors: it was conducted at golf courses, had multiple components, and was preceded by a motivational campaign.
El desarrollo de programas de prevención y detección de cáncer cutáneo específicamente dirigidos a grupos diana -de mayor rentabilidad que aquellos desarrollados sobre la población general- es necesario. Intervenciones en enclaves turísticos al aire libre ya demostraron eficacia, aunque no existen campañas específicas en campos de golf. Nuestros objetivos fueron describir el perfil de riesgo de los trabajadores y jugadores de golf y evaluar el impacto de una intervención.
Material y métodosEstudio transversal descriptivo desarrollado en 6 campos de golf, realizándose cuestionarios sobre datos demográficos, factores de riesgo y hábitos de exposición solar y fotoprotección, examen cutáneo. Se impartió consejo sanitario en fotoprotección, autoexamen y cremas fotoprotectoras, y finalmente se completaron encuestas de satisfacción e intención de cambio. Se midió el efecto en términos de: diagnósticos realizados, satisfacción con la intervención e intención expresada de cambio y efecto potencial en términos de factores de riesgo presentes.
ResultadosDe 351 participantes (el 57% golfistas, el resto trabajadores) el 70,4% tenían piel clara, el 11,7% tenían antecedentes familiares y el 8,5% personales de cáncer de piel. Entre los golfistas se diagnosticó cáncer cutáneo en el 10,7% y queratosis actínicas en el 40%. El 99,4% de los participantes valoró las jornadas positivamente, el 93,9% refirió intención de mejorar sus hábitos de fotoexposición y el 93,4% intención de examinarse la piel más frecuentemente.
ConclusionesTrabajadores de campos de golf y especialmente golfistas se confirman como una importante diana para la prevención del cáncer cutáneo. Esta es la primera campaña dirigida a estos grupos, resultando factible y útil el desarrollo de las mismas; su éxito parece relacionado con el desarrollo en el propio escenario, la intervención multicomponente y su estrategia publicitaria motivacional.
Skin cancer is the most common malignancy in white populations and is one of the costliest cancers to treat.1,2 The incidence of skin cancer in white people in Europe, North America, and Australia has steadily increased by 3% to 8% each year since 1960,3–8 and melanoma has the fastest-growing incidence in white populations of any type of cancer.8 These trends are a consequence of various factors, including the aging of the population, ozone depletion, and recreational sun exposure habits.6,8,9 In Spain, the incidence of skin cancer has tripled in recent decades and, despite advances in early diagnosis, the melanoma mortality rate continues to increase at a faster pace than that of any other malignancy.3
Sun exposure is the only major environmental causative factor for skin cancer (and precancer) that is preventable,6–8,10,11 and avoidance of intense intermittent sun exposure–the sort that occurs in golfers–and chronic sun exposure–the sort that occurs in golf course workers–is fundamental to prevention.10,12
Spain's Costa del Sol has a higher concentration of golf courses than any other region of Europe–hence its nickname, “Costa del Golf”–and it is also home to many foreign-born individuals, predominantly from northern and central Europe,13 who are attracted by the region's more than 300 days of sun per year.14 These residents have been identified as a group at risk of developing skin cancer and their high prevalence of cutaneous neoplasms15 is fundamentally associated with recreational sun exposure, often golf-related. Likewise, many tourists–especially those from outside of Spain, in particular northern and central Europeans–are attracted to the region's sun and beaches, but also in many cases to its golf courses. Outdoor workers–such as golf course workers, who receive chronic sun exposure–are another a priori at-risk group. Nevertheless, no interventions specifically designed to target these at-risk groups have been reported. Therefore, although golf is unquestionably beneficial to health,16 it is fundamental that golfers and golf course workers acquire correct sun protection habits in order to avoid developing skin cancer.
We carried out a skin cancer early detection and prevention campaign at golf courses on the Costa del Sol. The aims of this study were to describe the risk profile of golfers and golf course workers and to evaluate the impact of the intervention in terms of the number of diagnoses and the participants’ satisfaction and intention to change their current behaviors.
Patients and MethodsThis was a cross-sectional descriptive study. The campaign consisted of one-day visits, from 9:00 AM to 2:00 PM, at 6 golf courses in the western Costa del Sol between June and August 2011. The visits took place once per week and each golf course was visited only once. The golf courses were selected by convenience sampling from among the courses with the largest size, the largest number of players, and the highest-quality facilities.
The study population consisted of golfers, outdoor golf course workers (employees who usually spend their workday outside), and indoor golf course workers (employees who usually work inside). Although participation was voluntary, many of those present at the golf courses chose to participate.
The intervention model was designed by a group of experts (dermatologists and epidemiologists). We used a multicomponent model that included both primary prevention strategies (promotion of healthy habits) and secondary prevention strategies (early diagnosis of skin cancer). The strategies were very similar to the ones used in major skin cancer prevention campaigns in Europe,4,10 the United States,12,17–19 and Australia6 and in sun protection studies in beachgoers.12,17,18 The ultimate objective of these strategies is to change participants’ behavior in ways that translate into a lower incidence of skin cancer in these population groups.10,19 Our campaign included cognitive factors such as providing and explaining information about sun exposure habits, sun protection measures, proper selection of sunscreens, and other topics. It also included novel emotional and motivational factors such as biometric feedback12,20 and an educational-motivational technique of proven efficacy. This technique consists of identifying possible risk factors and behaviors, identifying suspicious lesions, using Wood light to identify subclinical sun damage, identifying risky behaviors, and providing individualized feedback about the findings–as the slogan says, encouraging participants to “enjoy the sun with precautions”–and about behavioral factors (for example, helping them choose the best sunscreen for their skin type). Another novel component was the inclusion of dermoscopy, a highly sensitive and specific diagnostic instrument in dermatology.21
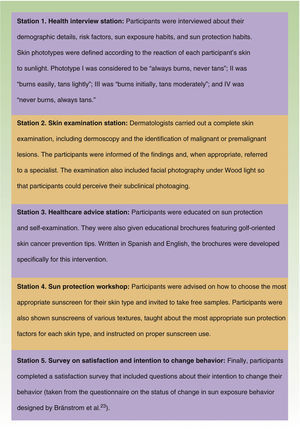
Under the slogan “Enjoy golf without harming your skin,” the intervention was carried out by a team of qualified healthcare professionals from the dermatology department at our hospital–including dermatologists, nurses, and auxiliary nurses–who were assigned to 5 healthcare stations (Fig. 1).20,22,23 We used a previously validated “beach questionnaire”22 about sun protection that was designed to assess sun-related habits, attitudes, and behaviors; with the authors’ permission, we adapted the questionnaire for use on golf courses. The questionnaire provided personalized biometric feedback on the risk of photoaging and photocarcinogenesis derived from the respondents’ risky behaviors and personal risk status. The questionnaire included 3 items on demographic details, 4 items on risk factors, 2 items on general sun exposure habits, 5 items on golf-related sun exposure habits, 6 items on golf-related sun protection practices, 7 items related to the physical examination, and 4 items on participants’ satisfaction and intention to change their behavior.
During the intervention, the questionnaires were administered by interview by the healthcare professionals running each station visited by the participants (Fig. 1).
The golf courses advertised the campaign several weeks in advance.
We carried out a descriptive analysis with measures of central tendency and dispersion for the quantitative variables and frequency distributions for the qualitative variables. We conducted a bivariate analysis comparing participant subgroups (indoor workers, outdoor workers, and golfers) in order to assess differences in the independent study variables using the ¿2 test for the qualitative variables and the Kruskal-Wallis test for the quantitative variables. The significance level was set at P<0.05.
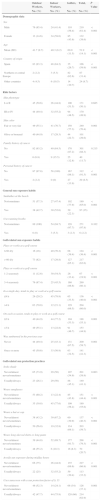
ResultsNine of the 351 individuals surveyed were excluded from the analysis because they were children. Of the 342 participants analyzed, 195 (57%) were golfers, 89 (26%) were outdoor workers, and 58 (16.9%) were indoor workers (Table 1).
Results (I): Demographic Data, Risk Factors, General Sun Exposure Habits, Golf-Related Sun Exposure Habits, and Golf-Related Sun Protection Practices.
| Outdoor Workers, | Indoor Workers, | Golfers, | Total, | P Value | |
|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | ||
| Demographic data | |||||
| Sex | |||||
| Male | 76 (85.4) | 24 (41.4) | 110 (56.4) | 210 (61.4) | <0.001 |
| Female | 13 (14.6) | 34 (58.6) | 85 (43.6) | 132 (38.6) | |
| Age | |||||
| Mean (SD) | 41.7 (9.7) | 40.3 (8.2) | 60.0 (11.5) | 51.9 (14.1) | <0.001 |
| Country of origin | |||||
| Spain | 83 (93.3) | 48 (84.2) | 35 (26.7) | 166 (59.9) | <0.001 |
| Northern or central Europe | 2 (2.2) | 3 (5.3) | 82 (62.6) | 87 (31.4) | |
| Other countries | 4 (4.5) | 6 (10.5) | 14 (10.7) | 24 (8.7) | |
| Risk factors | |||||
| Skin phototype | |||||
| I or II | 45 (50.6) | 26 (44.8) | 100 (51.5) | 171 (50.1) | 0.665 |
| III or IV | 44 (49.4) | 32 (55.2) | 94 (48.5) | 170 (49.9) | |
| Skin color | |||||
| Fair or very fair | 49 (55.1) | 41 (70.7) | 150 (77.3) | 240 (70.4) | 0.001 |
| Olive or bronzed | 40 (44.9) | 17 (29.3) | 44 (22.7) | 101 (29.6) | |
| Family history of cancer | |||||
| No | 82 (93.2) | 49 (84.5) | 170 (87.2) | 301 (88.3) | 0.215 |
| Yes | 6 (6.8) | 9 (15.5) | 25 (12.8) | 40 (11.7) | |
| Personal history of cancer | |||||
| No | 87 (97.8) | 58 (100) | 167 (86.1) | 312 (91.5) | <0.001 |
| Yes | 2 (2.2) | 0 (0) | 27 (13.9) | 29 (8.5) | |
| General sun exposure habits | |||||
| Sunbathes at the beach | |||||
| No/sometimes | 51 (57.3) | 27 (47.4) | 102 (77.9) | 180 (65.0) | <0.001 |
| Yes | 38 (42.7) | 30 (52.6) | 29 (22.1) | 97 (35) | |
| Uses tanning booths | |||||
| No/sometimes | 89 (100) | 54 (94.7) | 128 (97.7) | 271 (97.8) | 0.102 |
| Yes | 0 (0) | 3 (5.3) | 3 (2.3) | 6 (2.2) | |
| Golf-related sun exposure habits | |||||
| Plays or works at a golf course | |||||
| ≤ 60 d/y | 16 (18) | 40 (70.2) | 68 (39.4) | 124 (36.4) | <0.001 |
| > 60 d/y | 73 (82) | 17 (29.8) | 127 (65.1) | 217 (63.6) | |
| Plays or works at a golf course | |||||
| 1-2 seasons/y | 11 (12.6) | 30 (54.5) | 26 (13.4) | 67 (19.9) | <0.001 |
| 3-4 seasons/y | 76 (87.4) | 25 (45.5) | 168 (86.6) | 269 (80.1) | |
| In a single day, tends to play or work at a golf course | |||||
| ≤4 h | 26 (29.2) | 45 (78.9) | 65 (33.5) | 136 (40.0) | <0.001 |
| >4 h | 63 (70.8) | 12 (21.1) | 129 (66.5) | 204 (60.0) | |
| On each occasion, tends to play or work at a golf course | |||||
| ≤3 h | 40 (44.9) | 44 (77.2) | 104 (53.3) | 188 (55.1) | 0.001 |
| >3 h | 49 (55.1) | 13 (22.8) | 91 (46.7) | 153 (44.9) | |
| Was sunburned in the previous year | |||||
| Never | 44 (49.4) | 25 (43.1) | 131 (67.5) | 200 (58.7) | 0.001 |
| Once or more | 45 (50.6) | 33 (56.9) | 63 (32.5) | 141 (41.3) | |
| Golf-related sun protection practices | |||||
| Seeks shade | |||||
| Never/almost never/sometimes | 65 (73.9) | 29 (50) | 107 (54.9) | 201 (58.9) | 0.003 |
| Usually/always | 23 (26.1) | 29 (50) | 88 (45.1) | 140 (41.1) | |
| Wears sunglasses | |||||
| Never/almost never/sometimes | 53 (60.2) | 13 (22.4) | 85 (43.8) | 151 (44.4) | <0.001 |
| Usually/always | 35 (39.8) | 45 (77.6) | 109 (56.2) | 189 (55.6) | |
| Wears a hat or cap | |||||
| Never/almost never/sometimes | 38 (43.2) | 39 (67.2) | 60 (30.9) | 137 (40.3) | <0.001 |
| Usually/always | 50 (56.8) | 19 (32.8) | 134 (69.1) | 203 (59.7) | |
| Wears long-sleeved shirts or long pants | |||||
| Never/almost never/sometimes | 39 (44.8) | 52 (89.7) | 177 (91.7) | 268 (79.3) | <0.001 |
| Usually/always | 48 (55.2) | 6 (10.3) | 16 (8.3) | 70 (20.7) | |
| Avoids sun exposure during midday hours | |||||
| Never/almost never/sometimes | 66 (75) | 26 (44.8) | 135 (69.6) | 227 (66.8) | <0.001 |
| Usually/always | 22 (25) | 32 (55.2) | 59 (30.4) | 113 (33.2) | |
| Uses sunscreen with a sun protection factor of ≥ 15 | |||||
| Never/almost never/sometimes | 46 (52.3) | 14 (24.1) | 66 (34) | 126 (37.1) | 0.001 |
| Usually/always | 42 (47.7) | 44 (75.9) | 128 (66) | 214 (62.9) | |
The mean age of the 342 participants was 51.9 (14.1) years, with statistically significant differences between the three groups: 60 (11.5) years for golfers, 41.7 (9.7) years for outdoor workers, and 40.3 (8.2) years for indoor workers.
Men accounted for 61.4% of the participants, although there were significant differences between groups (56.4% of golfers were men, compared with 85.4% of outdoor workers and 41.4% of indoor workers).
The participants were from 25 different countries of origin, although 59.9% were Spanish and 31.3% were from central or northern Europe, and there were statistically significant differences between groups. Of the golfers, 62.6% were from central or northern Europe and 26.7% were Spanish. In contrast, 93.3% of outdoor workers and 84.2% of indoor workers were Spanish.
Risk FactorsSkin color was fair or very fair in 70.4% of participants, although there were significant differences among groups: 77.3% of golfers, 55.1% of outdoor workers, and 70.7% of indoor workers had fair or very fair skin. Skin phototype was I or II in 50.1% of participants, and there were no significant differences between groups.
Participants had a family history of cancer in 11.7% of cases, and there were no statistically significant differences between groups. A personal history of skin cancer (of any type) was reported by 8.5% of participants, with significant differences between groups (13.9% of golfers, 2.2% of outdoor workers, and zero indoor workers).
Sun Exposure HabitsRegular sunbathing on the beach in summer was reported by 35% of participants, and there were statistically significant differences between groups (22.1% of golfers, 42.7% of outdoor workers, and 52.6% of indoor workers).
Fully 97.5% of participants said they never used tanning booths, and there were no significant differences between groups.
There were statistically significant differences between the groups’ golf-related sun exposure habits. Golf-related sun exposure occurred more than 60 days per year in 63.6% of participants (65.1% of golfers, 29.8% of indoor workers, and 82% of outdoor workers). Golf-related sun exposure took place for 3 or 4 seasons of the year in 80.1% of participants (86.6% of golfers, 45.5% of indoor workers, and 87.4% of outdoor workers). Sixty percent of participants (66.5% of golfers, 21.1% of indoor workers, and 70.8% of outdoor workers) said they had more than 4hours of golf-related sun exposure each day, and 44.9% (46.7% of golfers, 22.8% of indoor workers, and 55.1% of outdoor workers) said they had more than 3hours of sun exposure between the hours of 11:00 AM and 5:00 PM. In addition, 41.3% of participants (32.5% of golfers, 56.9% of indoor workers, and 50.6% of outdoor workers) said they had had a golf-related sunburn in the previous year.
Golf-Related Sun Protection PracticesSignificant differences in golf-related sun protection practices were found between groups. First, 41.4% of participants (45.1% of golfers, 50% of indoor workers, and 26.1% of outdoor workers) said they always or usually sought shade. Second, 55.6% of participants (56.2% of golfers, 77.6% of indoor workers, and 39.8% of outdoor workers) said they always or usually wore sunglasses. Third, 59.7% of participants (69.2% of golfers, 32.8% of indoor workers, and 56.8% of outdoor workers) said they always or usually wore a hat or cap. Fourth, 20.7% of participants (8.3% of golfers, 10.3% of indoor workers and 55.2% of outdoor workers) said they always or usually wore a long-sleeved shirt or long pants. Fifth, 33.2% of participants (30.4% of golfers, 55.2% of indoor workers, and 25% of outdoor workers) said they avoided sun exposure during midday hours. Finally, 62.9% of participants (66% of golfers, 75.9% of indoor workers, and 47.7% of outdoor workers) said they always or usually wore sunscreen with a sun protection factor of at least 15.
Physical ExaminationLesions highly suggestive of skin cancer were diagnosed in 23 (6.7%) participants (10.3% of golfers, 3% of outdoor workers, and zero indoor workers) (Table 2). In addition, actinic keratoses were diagnosed in 25.7% of participants, and the differences between groups were significant (40% of golfers, 10.1% of outdoor workers, and 1.7% of indoor workers) (Table 2).
Results (II): Physical Examination, Satisfaction, and Intention to Change Behavior.
| Indoor Workers, No. (%) | Outdoor Workers, No. (%) | Golfers, No. (%) | Total, No. (%) | P Value | |
|---|---|---|---|---|---|
| 58 (16.9%) | 89 (26%) | 195 (57%) | 342 (100%) | ||
| Physical examination | |||||
| Actinic keratoses | |||||
| No | 57 (98.3) | 80 (89.9) | 117 (60) | 254 (74.3) | <0.001 |
| Yes | 1 (1.7) | 9 (10.1) | 78 (40) | 88 (25.7) | |
| No. of melanocytic nevi | |||||
| <50 | 46 (79.3) | 77 (86.5) | 173 (88.7) | 296 (86.5) | 0.183 |
| ≥50 | 12 (20.7) | 12 (13.5) | 22 (11.3) | 46 (13.5) | |
| Atypical nevi | |||||
| No | 48 (82.8) | 78 (87.6) | 180 (92.3) | 306 (89.5) | 0.093 |
| Yes | 10 (17.2) | 11 (12.4) | 15 (7.7) | 36 (10.5) | |
| Clinical suspicion of melanoma | |||||
| No | 58 (100) | 87 (97.8) | 192 (98.5) | 337 (98.5) | 0.535 |
| Yes | 0 (0) | 2 (2.2) | 3 (1.5) | 5 (1.5) | |
| Clinical suspicion of SCC | |||||
| No | 58 (100) | 89 (100) | 191 (97.9) | 338 (98.8) | 0.218 |
| Yes | 0 (0) | 0 (0) | 4 (2.1) | 4 (1.2) | |
| Clinical suspicion of BCC | |||||
| No | 58 (100) | 87 (97.8) | 180 (92.3) | 325 (95) | 0.024 |
| Yes | 0 (0) | 2 (2.2) | 15 (7.7) | 17 (5) | |
| Clinical suspicion of skin cancer | |||||
| No | 58 (100) | 86 (96.6) | 175 (89.7) | 319 (93.3) | 0.008 |
| Yes | 0 (0) | 3 (3.4) | 20 (10.3) | 23 (6.7) | |
| Satisfaction and intention to change behavior | |||||
| Opinion of the campaign | |||||
| Negative/neutral | 0 (0) | 0 (0) | 2 (1.1) | 2 (0.6) | 0.45 |
| Positive/very positive | 58 (100) | 89 (100) | 183 (98.9) | 330 (99.4) | |
| Most interesting part of the campaign | |||||
| Information received about sun exposure and skin cancer prevention | 2 (3.4) | 1 (1.1) | 20 (11.4) | 23 (7.1) | 0.005 |
| Skin examination by dermatologist | 9 (15.5) | 22 (24.7) | 55 (31.4) | 86 (26.7) | |
| Advice on sunscreens | 0 (0) | 0 (0) | 2 (1.1) | 2 (0.6) | |
| Educational brochures | 1 (1.7) | 1 (1.1) | 1 (0.6) | 3 (0.9) | |
| It was all interesting | 46 (79.3) | 65 (73) | 97 (55.4) | 208 (64.6) | |
| Intention to improve sun exposure habits | |||||
| Not at all/slightly | 3 (5.2) | 6 (6.7) | 11 (6) | 20 (6.1) | 0.927 |
| Somewhat/a lot | 55 (94.8) | 83 (93.3) | 171 (94) | 309 (93.9) | |
| Intention to examine his/her skin more frequently | |||||
| Not at all/slightly | 3 (5.2) | 3 (3.4) | 13 (7.1) | 19 (5.8) | 0.453 |
| Somewhat/a lot | 55 (54.8) | 86 (96.6) | 170 (92.9) | 311 (94.2) | |
In the satisfaction surveys, 99.4% of participants described the campaign as positive or very positive, 93.9% said that they intended to adopt better sun exposure habits, and 93.4% said they planned to examine their skin more frequently. There were no statistically significant differences between groups.
DiscussionThe skin cancer prevention campaign described in this study is the first such campaign described in the literature to specifically target golfers and golf course workers. In this campaign, these groups were confirmed to be at risk and, therefore, appropriate targets for both primary prevention strategies (because of their intrinsic risk factors and sun exposure habits) and secondary prevention strategies (because of the high prevalence of clinical diagnoses of malignant or premalignant lesions). In addition, the participants expressed a high degree of satisfaction as well as the intention to change their sun exposure habits.
The first public skin cancer prevention and detection programs were launched in the United States in the 1980s.19 Programs of this sort appear to have brought about a marked reduction in sun exposure2 and, more importantly, a decrease in skin cancer mortality rates.6 Nevertheless, it appears increasingly evident that actions targeting specific groups–which are more cost-effective than those targeting the general population–should be developed.2,4–7,11,19,20 In addition, educational interventions in outdoor tourist enclaves have been shown to be effective at improving sun protection habits.11
One key aspect of this campaign was the fact that it was carried out at the very site of risky activity. The on-site design allowed the intervention to directly “inoculate” the target population. It also facilitated the participation of golfers and golf course workers, who were able to gain access to health professionals without having to overcome the usual administrative hurdles. Because the campaign was covered by several regional media organizations and featured the participation of former professional golfers and retired elite athletes who enjoy the sport, we were able to spread information to the general population beyond the golf courses.
The relationship between knowledge and changes in behavior is often inconsistent.7,10,17–19 In order to maximize the likelihood of behavior changes, it is therefore important to correctly design actions based on the transtheoretical model of behavior change,24 which suggests that individuals facing health problems go through certain stages in the process of changing their behavior. We therefore used a multicomponent intervention model similar to those which have already been used successfully in Australia2 and the United States.18,24 The biometric feedback techniques associated with healthcare information and education have proved to be more effective than education alone at improving attitudes and behaviors related to sun exposure in at-risk groups.12 Moreover, studies have shown that taking photographs under Wood light, showing patients their light-induced skin damage, and explaining the significance of the damage is an effective way to improve sun protection behaviors, even in the long term.25,26
The results confirmed that golfers (in particular) and golf course workers (especially those who work outdoors) were groups at risk of developing skin cancer because of their intrinsic risk factors, the fact that they have fair or very fair skin (especially the golfers, many of whom were from central or northern Europe),15 and their considerable history of skin cancer–both family history and, more importantly, personal history (especially in golfers). Golfers and golf course workers also faced risks associated with their sun exposure habits. Golf is a risky activity independent of sun exposure at the beach (a location visited more often by the golf course workers) or use of tanning booths (used by hardly any participants). The sun exposure habits of golfers and outdoor workers, in particular, consisted of many days of sun exposure per year, throughout almost the entire year, with daily exposure times of several hours, many of these occurring during the midday hours. In addition, nearly half of the participants reported having had at least one golf-related sunburn in the previous year. The golf-related sunburn rate was especially high in indoor workers, probably because of their more acute and intermittent sun exposure habits. We also identified risks related to sun protection measures. Participants used sun protection measures insufficiently and irregularly, with significant differences in application between groups. In agreement with most studies,7 sunscreen was the most frequently used sun protection method overall, although it was used by fewer than two thirds of the participants and the rate of sunscreen use was especially low among outdoor workers, possibly because of the cost. Sun protection recommendations tell us that sunscreen use should be accompanied by other methods.7 Moreover, although sunscreen has proved effective in the prevention of actinic keratoses and sunburns,6 some studies have suggested that there may be an elevated number of malignant or premalignant skin lesions in sunscreen users, probably because they compensate for their sunscreen use by staying in the sun for longer periods.6,7
Hats and caps were the most common sun protection method among golfers and outdoor workers, possibly due to the influence of role models (professional golfers) who also tend to favor this method. Less common was the use of long-sleeved shirts, which are rarely worn by professional golfers. However, long-sleeved shirts were worn more frequently by outdoor workers, in many cases probably because of work uniform requirements.
Finally, the physical examinations revealed a high prevalence of clinical diagnoses of malignant and premalignant skin lesions among the participants. Because of the unique design of our study, it is difficult to compare the skin lesion prevalence in our study with those found in other studies; nevertheless, the figures in our study were generally higher than those found in the Euromelanoma campaigns4,27 and in other screening campaigns conducted in Spain and elsewhere in Europe.5 Additionally, examination under Wood light revealed intense subclinical light-induced damage in most participants. The high prevalence of actinic keratoses diagnosed, especially among golfers, was especially remarkable. Independent of golf, the high rate of diagnoses of skin cancer may be influenced by the high rate of participation of adults over 50 years of age and, especially among golfers, of foreign-born individuals with light skin phototypes. Similarly, the relatively low prevalence of diagnoses of malignant or premalignant lesions in golf course workers in comparison to golfers could be related to the fact that the workers tend to be younger (in other words, they have not yet had time to develop these lesions).
The campaign was received very well by the participants, who showed great interest in all aspects of the intervention and identified the skin examination by the dermatologist as the most interesting specific aspect. Although some studies12 have postulated that campaigns of this type could not, by themselves, bring about improvements in sun protection behavior, most participants in our study said that they intended to change their sun exposure habits and to examine their skin more frequently.
One limitation of this study is the possible existence of a selection bias owing to the fact that participation was voluntary. However, in order to encourage participation, we offered complete physical examinations by dermatologists free of charge as well as free samples of sunscreens, and the golf course managers agreed to facilitate the participation of their workers.
Another limitation is the fact that the clinical diagnoses were not confirmed histologically, due to the fact that some of the participants lived outside of our healthcare area. Nevertheless, the diagnoses were made by specialists with experience in skin cancer and dermoscopy, a technique not used in many previous studies.4
Another limitation is the fact that the variables used to evaluate sun protection behaviors were indirect measures (questionnaires). However, questionnaires are the most common instrument for studying behaviors related to sun exposure, and the survey used in our study was a modified version of a previously validated survey.22 Finally, the participants may be influenced by a memory bias, which could explain why the golfers reported relatively low rates of sunburn in previous years.
The final limitation is the difficulty of conducting a complete evaluation of the campaign. The evaluations were administered once, without any subsequent follow-up of the participants.12,19 In the future, it would be advisable to develop actions with a greater degree of continuity in these target groups.2
Further studies are needed in order to determine the real impact of these interventions on the health of the population as well as their long-term benefits. It would also be advisable to carry out interventions that are sustained over time in other at-risk populations.
In conclusion, golfers and golf course workers are a key target population in the prevention of skin cancer. It is feasible and pertinent to launch awareness-raising campaigns that specifically target these groups. One key factor in the success of the campaign was the fact that it was carried out at the site of risky behavior. Another factor was the development of a multi-component intervention model that included innovative techniques and a motivational strategy.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that no private patient data appear in this article.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to the Association of Golf Courses of Marbella for collaborating on the campaign.
We are grateful to La Roche-Posay for providing sunscreen samples and for developing the educational brochures.
Please cite this article as: del Boz J, Fernández-Morano T, Padilla-España L, Aguilar-Bernier M, Rivas-Ruiz F, de Troya-Martín M. Campaña de prevención y detección de cáncer cutáneo en campos de golf de la Costa del Sol. Actas Dermosifiliogr. 2015;106:51–60.