Shellac is the purified form of a resin produced by the female lac bug, Kerria lacca. It is widely used in the wood, cosmetics, food, and pharmaceutical industries.1–3 It is precisely the ubiquitous nature of shellac that makes it difficult to interpret positive results in patch tests.2
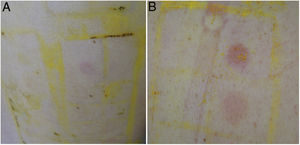
In order to determine the relevance of positive results to shellac and their clinical correlation, we retrospectively reviewed positive results to this allergen over a 5-year period (2016–2020) in our contact dermatitis unit. All patients were assessed using the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea [GEIDAC]) and a cosmetics series (Chemotechnique). Furthermore, depending on the clinical setting, we used specific series and the patient's own products. We recorded patient-related variables (age, sex, association with profession, and diagnosis of atopic dermatitis), as well as the allergens evaluated, the patch test results (positive allergens and their relevance), and the distribution of lesions in the individual patient. During the study period, we assessed 1093 patients, of whom 176 were tested with shellac-containing cosmetics series, yielding 21 positive results. One-third (33%) of the shellac-positive patients were involved in household chores and 23.8% in health care. Table 1 shows the MOAHLFA index of the 21 shellac-positive patients and of the whole sample. The reaction was weak (+) in 16 of the 21 patients (76%) (Fig. 1A) and more intense (++) in the remaining 5 (24%) (Fig. 1B). Doubtful responses (+?) were not recorded owing to their high frequency. Shellac generated the sole positive result in only 2 patients. Other commonly detected allergens in these patients were nickel (8 patients), gold (4 patients), and Kathon CG, methylisothiazolinone, and linalool (3 patients). The clinical manifestations of shellac-positive patients were facial dermatitis in 11 cases, desquamative cheilitis in 4, exclusively palpebral dermatitis in 2, and disseminated eczematous lesions on the face, hands, and axillae in 1 case. The patch test results were considered relevant (present relevance) in only 1 of the 21 shellac-positive patients (4.7%). This relevance was established after revising the components of the patient's own products and verifying the progress of eczema in the clinical history once the patient had avoided the allergy.
MOAHLFA Index for Patients With Positive Reactions to Shellac and for all Patients Assessed During the Same Study Period (2016–2020).
| Patients with positive results to shellacN=21 | % | Total no. of patients assessedN=1093 | % | |
|---|---|---|---|---|
| M | 1 | 4.76 | 349 | 31.93 |
| O | 1 | 4.76 | 37 | 3.39 |
| A | 3 | 1.43 | 170 | 15.55 |
| H | 3 | 1.43 | 398 | 36.41 |
| L | 0 | 0 | 101 | 9.24 |
| F | 21 | 100 | 262 | 23.97 |
| A | 18 | 85.71 | 834 | 76.30 |
Abbreviation: MOAHLFA, male, occupational dermatitis, atopic dermatitis, hand dermatitis, leg dermatitis, face dermatitis age (>40 y).
Traditionally, shellac has had several applications. In the food industry (food additive E-904), its uses include food packaging, food-safe resin, biodegradable films, emulsifiers, and foaming agents.3 In health care, it can be found in dental molds and drug packaging. In the cosmetic industry, its properties as a film-forming agent, emollient, and adhesive have enabled it to be used as lipstick, mascara, eyeliner, spray, lacquer, and hair dye. Specifically, most cases of allergic contact dermatitis caused by shellac have been associated with lipstick, mascara, and eyeliner.1 The symptoms reported in these cases typically manifest as facial dermatitis or erosive cheilitis.4–7
The shellac-positive patients in our study also consulted mainly for cheilitis and palpebral or facial eczema. However, in our experience, it proved problematic in most cases to confirm the definitive relevance of this positive result owing to various factors. First, a high percentage of the responses were weak (76%). Second, this allergen was ubiquitous. Third, it was considerably difficult to obtain the exact composition of the patients’ own products, since very often they only brought lipstick or eyeshadow, with no data on the ingredients. Lastly, almost all the patients (19/21) were concomitantly sensitized to other allergens that could potentially cause similar symptoms. Therefore, given the high proportion of weak or doubtful responses, shellac should be considered a problematic allergen (ratio of positive results [quotient of mild allergic responses divided by total allergic responses×100]≥55%).8
We require prospective studies that systematically include this allergen in order to clarify both the effectiveness of its use in patch tests and its present relevance, as well as its true role in patients with symptoms of facial and palpebral dermatitis or cheilitis.7,9 In fact, shellac has been included among the components of the extended standard GEIDAC series.10 We expect that the analysis of data from the Spanish Contact Dermatitis Registry (REIDAC) will go some way to clarifying these issues.
Conflict of InterestsThe authors declare that they have no conflict of interest.