Pain is a common, important symptom negatively affecting the well-being and quality of life of patients with hidradenitis suppurativa (HS). The aim of this study was to examine self-reported pain alleviating methods among outpatients attending a tertiary referral center.
MethodsConsecutive patients with HS were invited to complete a questionnaire regarding their self-reported pain alleviating methods for HS associated pain. Additionally, the patients filled out the Dermatology Life Quality Index questionnaire and a visual analog scale for overall distress related to HS and for boil-associated pain in the past month. Information on disease severity and onset was obtained by interview and clinical examination.
ResultsA total of 134 patients with a mean age of 38.3 years (SD 12.8) participated; 32% (n = 43) had Hurley stage i, 52% (n = 70) had Hurley stage ii, and 16% (n = 21) had Hurley stage iii. Overall, to achieve pain relief, 82% (n = 110) of the patients had previously drained pus from the lesions by manual pressure. Compared to patients who did not alleviate pain, patients who attempted to alleviate pain had a higher mean overall disease related distress score (7.43 [SD 2.81] vs. 5.47 [SD 3.37], p < 0.003), and a higher boil-associated pain score in the past month (6.56 [SD 3.07] vs. 4.39 [SD 3.88], p = 0.007).
ConclusionThis study demonstrates that a large proportion of HS patients attempt to alleviate pain through various alternative and homespun methods. These results may reflect a major role of pain in HS and its potential insufficient management by dermatologists.
El dolor es un síntoma común e importante que afectará negativamente el bienestar y la calidad de vida de los pacientes con hidradenitis supurativa (HS). El objetivo del presente estudio fue valorar los métodos utilizados para aliviar el dolor asociado a la HS, referidos por los pacientes ambulatorios provenientes de un centro de referencia terciario.
MétodosSe seleccionaron de manera consecutiva pacientes con el diagnóstico de HS. Posteriormente se les invitó a que completasen un cuestionario acerca de cuáles eran los métodos que utilizaban para aliviar el dolor asociado a la HS. Así mismo, los pacientes completaron el cuestionario del Índice de Calidad de Vida en Dermatología y la escala visual analógica acerca de las molestias generales que presentaban en relación con la HS, así como el dolor asociado a la aparición de forúnculos en el último mes. La información sobre la gravedad y la forma de presentación de la enfermedad se obtuvo mediante la anamnesis y el examen clínico.
ResultadosSe incluyeron un total de 134 pacientes con una edad media de 38,3 años (DE 12,8). El 32% (n = 43) tenía un estadio i, el 52% (n = 70) un estadio ii y el 16% (n = 21) un estadio iii de Hurley. Para lograr el alivio del dolor el 82% (n = 110) de los pacientes refirieron que habían drenado el pus de las lesiones inflamatorias usando la presión de los dedos. En comparación con los pacientes que no habían usado ningún método para aliviar el dolor, los pacientes que sí lo habían hecho tuvieron en general un mayor grado de angustia en relación con la enfermedad (7,43 [DE 2,81] frente a 5,47 [DE 3,37], p < 0,003), así como un mayor grado de dolor asociado a la presencia de forúnculos durante el último mes (6,56 [DE 3,07] frente a 4,39 [DE 3,88], p = 0,007).
ConclusiónEl presente estudio demuestra que una elevada proporción de los pacientes con HS intentarán aliviar el dolor por sí mismos utilizando diversos métodos caseros y alternativos. Estos resultados reflejan la importancia del dolor en la HS y que posiblemente el manejo de este por los dermatólogos sea insuficiente.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by painful nodules and abscesses affecting the intertriginous areas (e.g. the axilla or groin).1–4
Studies have shown that HS has a profound negative impact on quality of life.5–9 Patients with HS have the lowest quality of life compared to other chronic skin conditions such as psoriasis5–9 and the impairment seems to be associated with disease severity.7–9
Pain is the most commonly reported symptom, and is typically related to the inflammatory lesions.10 The chronicity of pain and the exacerbation of pain during flares makes this symptom the most troublesome aspect of HS. Studies comparing pain in HS with other dermatological conditions have shown that the pain in HS is of higher intensity.5,8,11
Our aim was to explore pain-related behavior in patients with HS to achieve a better and broader understanding of this troublesome aspect in HS patients. As pain in HS is typically related to the inflammatory lesions; i.e. nodules and sinus tracts, we evaluated pain-alleviating methods in relation to these.
MethodsStudy population and patient characteristicsThe study was a non-interventional, cross-sectional, single-center study conducted at the Department of Dermatology, Bispebjerg Hospital, Copenhagen, Denmark, from June 2018 to January 2019. A total of 134 consecutive patients with HS who were attending this department were invited to answer the questionnaire.
Routine clinical examination was performed by a hospital-based dermatologist with high expertise in HS and evaluation of HS severity was based on the overall Hurley staging,12 a score based on physical findings including involvement of specific anatomical sites and the number of nodules, sinus tracts, and scars.1,12 Information of onset of HS (since the patients’ first recollection of symptoms of HS), smoking, and employment status was obtained through interview. Patients also filled out the Dermatology Life Quality Index (DLQI) and a Visual Analog Scale (VAS) from 0 to 10 points to document overall disease related distress with 0 corresponding to “unaffected by” and 10 corresponding to the “worst imaginable distress” caused by HS. Pain caused by possible boils in the past month was also evaluated by VAS.
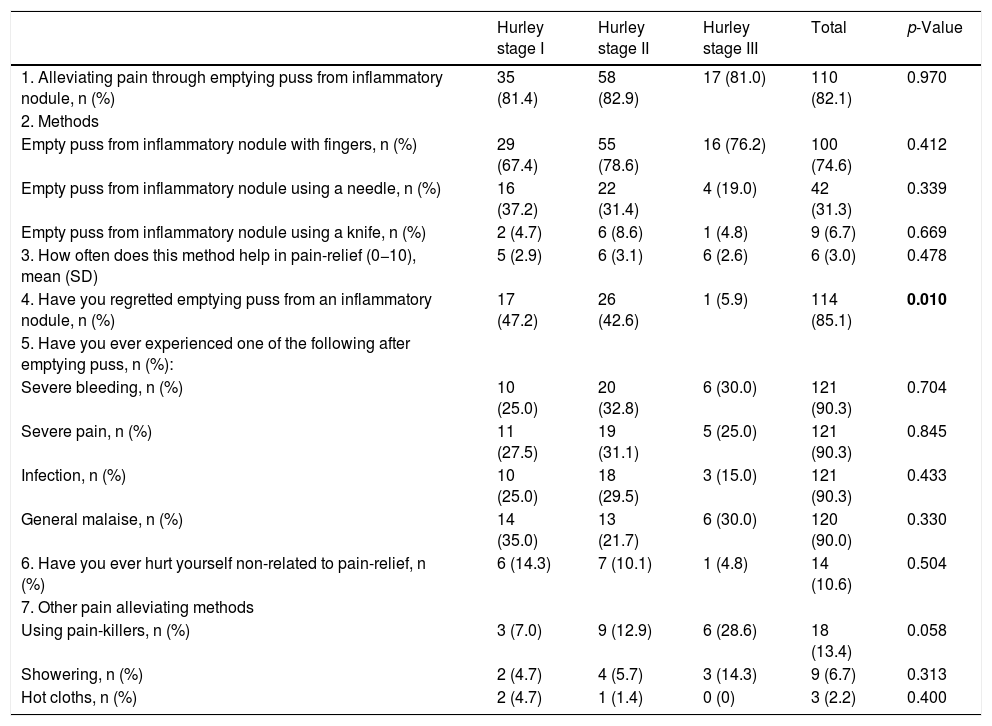
QuestionnaireTo explore the potential level of pain-alleviating methods in patients with HS, the authors constructed a seven-item questionnaire (Table 2). The questionnaire contained multiple-choice questions about whether patients emptied puss from inflammatory lesions and if so how; efficacy of the methods and subsequent symptoms (i.e. excessive bleeding, infection, malaise). Furthermore, patients were asked to describe other pain alleviating methods. Lastly, information on history of self-harm was noted.
Statistical analysisAll descriptive and statistical analyses were performed using SPSS Statistics (version 22.0, IBM, USA). For descriptive purposes, continuous data were presented as means with standard deviations (SD) and ranges, and categorical data as numbers with percentages. Relationships between explanatory variables and pain alleviation were examined with ANOVA and chi-square tests. p-Values of <0.05 were considered statistically significant.
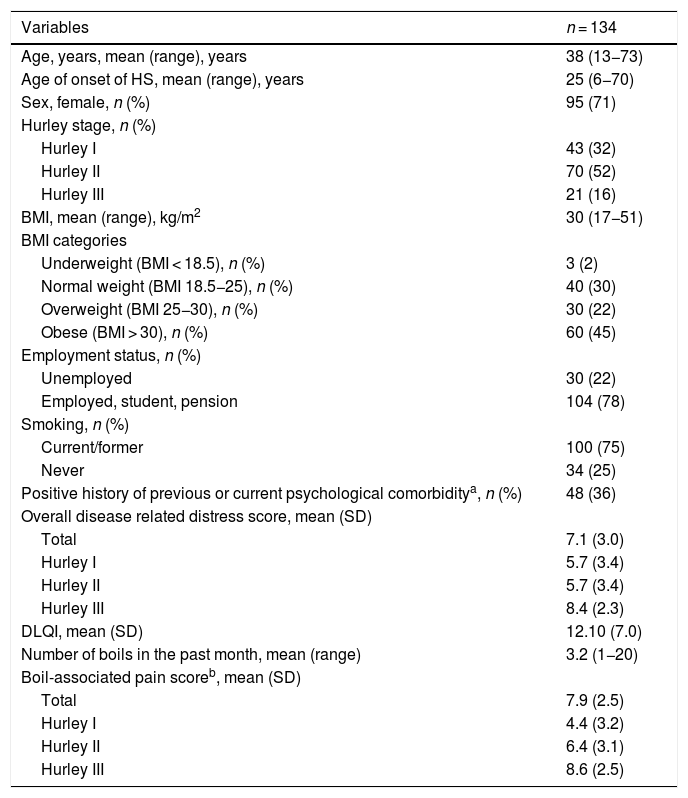
ResultsPatient characteristicsA total of 134 patients (95 women and 39 men) with a mean age of 38.3 years (SD = 12.8) participated; 32% (n = 43) had Hurley stage I, 52% (n = 70) had Hurley stage II, and 16% (n = 21) had Hurley stage III. The mean age of onset of HS was 25 years (range 6–70). A positive family history was noted in 40% (n = 53); 75% (n = 100) were current or former smokers and 67% (n = 90) were either overweight or obese (BMI > 25 kg/m2) (Table 1). The overall mean disease related distress score was 7.1 (SD = 3.0) and mean DLQI was 12.10 (SD = 7.3). Presence of boils in the past month was reported by 71% (n = 95) of the patients with a mean number of boils in the past month of 3.2 (range 1–20), and mean boil-associated pain score in the past month was 7.9 (SD = 2.5) (Table 1).
Patient characteristics.
| Variables | n = 134 |
|---|---|
| Age, years, mean (range), years | 38 (13−73) |
| Age of onset of HS, mean (range), years | 25 (6−70) |
| Sex, female, n (%) | 95 (71) |
| Hurley stage, n (%) | |
| Hurley I | 43 (32) |
| Hurley II | 70 (52) |
| Hurley III | 21 (16) |
| BMI, mean (range), kg/m2 | 30 (17−51) |
| BMI categories | |
| Underweight (BMI < 18.5), n (%) | 3 (2) |
| Normal weight (BMI 18.5−25), n (%) | 40 (30) |
| Overweight (BMI 25−30), n (%) | 30 (22) |
| Obese (BMI > 30), n (%) | 60 (45) |
| Employment status, n (%) | |
| Unemployed | 30 (22) |
| Employed, student, pension | 104 (78) |
| Smoking, n (%) | |
| Current/former | 100 (75) |
| Never | 34 (25) |
| Positive history of previous or current psychological comorbiditya, n (%) | 48 (36) |
| Overall disease related distress score, mean (SD) | |
| Total | 7.1 (3.0) |
| Hurley I | 5.7 (3.4) |
| Hurley II | 5.7 (3.4) |
| Hurley III | 8.4 (2.3) |
| DLQI, mean (SD) | 12.10 (7.0) |
| Number of boils in the past month, mean (range) | 3.2 (1−20) |
| Boil-associated pain scoreb, mean (SD) | |
| Total | 7.9 (2.5) |
| Hurley I | 4.4 (3.2) |
| Hurley II | 6.4 (3.1) |
| Hurley III | 8.6 (2.5) |
Categorical variables are number (percentage), continuous variables are mean (range) and (standard deviation).
Results of the questionnaire and differences in pain alleviating methods between the Hurley stages.
| Hurley stage I | Hurley stage II | Hurley stage III | Total | p-Value | |
|---|---|---|---|---|---|
| 1. Alleviating pain through emptying puss from inflammatory nodule, n (%) | 35 (81.4) | 58 (82.9) | 17 (81.0) | 110 (82.1) | 0.970 |
| 2. Methods | |||||
| Empty puss from inflammatory nodule with fingers, n (%) | 29 (67.4) | 55 (78.6) | 16 (76.2) | 100 (74.6) | 0.412 |
| Empty puss from inflammatory nodule using a needle, n (%) | 16 (37.2) | 22 (31.4) | 4 (19.0) | 42 (31.3) | 0.339 |
| Empty puss from inflammatory nodule using a knife, n (%) | 2 (4.7) | 6 (8.6) | 1 (4.8) | 9 (6.7) | 0.669 |
| 3. How often does this method help in pain-relief (0−10), mean (SD) | 5 (2.9) | 6 (3.1) | 6 (2.6) | 6 (3.0) | 0.478 |
| 4. Have you regretted emptying puss from an inflammatory nodule, n (%) | 17 (47.2) | 26 (42.6) | 1 (5.9) | 114 (85.1) | 0.010 |
| 5. Have you ever experienced one of the following after emptying puss, n (%): | |||||
| Severe bleeding, n (%) | 10 (25.0) | 20 (32.8) | 6 (30.0) | 121 (90.3) | 0.704 |
| Severe pain, n (%) | 11 (27.5) | 19 (31.1) | 5 (25.0) | 121 (90.3) | 0.845 |
| Infection, n (%) | 10 (25.0) | 18 (29.5) | 3 (15.0) | 121 (90.3) | 0.433 |
| General malaise, n (%) | 14 (35.0) | 13 (21.7) | 6 (30.0) | 120 (90.0) | 0.330 |
| 6. Have you ever hurt yourself non-related to pain-relief, n (%) | 6 (14.3) | 7 (10.1) | 1 (4.8) | 14 (10.6) | 0.504 |
| 7. Other pain alleviating methods | |||||
| Using pain-killers, n (%) | 3 (7.0) | 9 (12.9) | 6 (28.6) | 18 (13.4) | 0.058 |
| Showering, n (%) | 2 (4.7) | 4 (5.7) | 3 (14.3) | 9 (6.7) | 0.313 |
| Hot cloths, n (%) | 2 (4.7) | 1 (1.4) | 0 (0) | 3 (2.2) | 0.400 |
Categorical variables are number (percentage), continuous variables are mean (standard deviation).
Of the 134 patients, 82% (n = 110) reported having tried to relieve pain from inflamed lesions on their own through various methods (Table 2). Drainage of puss from inflamed lesions was done using the fingers (74.6%); a needle (31.3%); or to a lesser degree, a knife (6.7%). Other commonly reported pain alleviating methods include usage of pain-killers (13.4%), showering (6.7%) and application of hot cloths to painful lesions (2.2%). Self-harm non-related to pain-relief was reported by 10.6% of the patients. Presence of psychological comorbidity was significantly associated with self-harm non-related to pain-relief (p = 0.004). Self-harm non-related to pain-relief was reported more often in patients with a history of psychological comorbidity than patients without (20.8% (n = 10) vs. 4.8% (n = 4)).
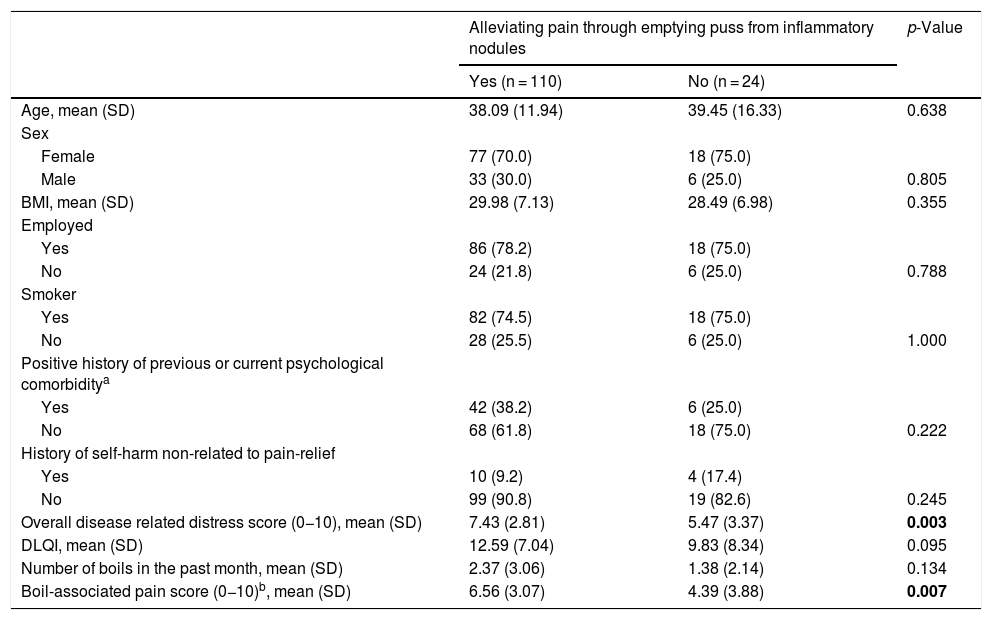
Characteristics of HS patients alleviating painPatients with the tendency to alleviate pain had a significantly greater mean overall disease related distress score than patients who did not (7.43 (SD = 2.81) vs. 5.47 (SD = 3.37), p < 0.003), the same was also seen for boil-associated pain in the past month (6.56 (SD = 3.07) vs. 4.39 (SD = 3.88), p = 0.007) (Table 3).
Factors associated with alleviating pain in patients with HS.
| Alleviating pain through emptying puss from inflammatory nodules | p-Value | ||
|---|---|---|---|
| Yes (n = 110) | No (n = 24) | ||
| Age, mean (SD) | 38.09 (11.94) | 39.45 (16.33) | 0.638 |
| Sex | |||
| Female | 77 (70.0) | 18 (75.0) | |
| Male | 33 (30.0) | 6 (25.0) | 0.805 |
| BMI, mean (SD) | 29.98 (7.13) | 28.49 (6.98) | 0.355 |
| Employed | |||
| Yes | 86 (78.2) | 18 (75.0) | |
| No | 24 (21.8) | 6 (25.0) | 0.788 |
| Smoker | |||
| Yes | 82 (74.5) | 18 (75.0) | |
| No | 28 (25.5) | 6 (25.0) | 1.000 |
| Positive history of previous or current psychological comorbiditya | |||
| Yes | 42 (38.2) | 6 (25.0) | |
| No | 68 (61.8) | 18 (75.0) | 0.222 |
| History of self-harm non-related to pain-relief | |||
| Yes | 10 (9.2) | 4 (17.4) | |
| No | 99 (90.8) | 19 (82.6) | 0.245 |
| Overall disease related distress score (0−10), mean (SD) | 7.43 (2.81) | 5.47 (3.37) | 0.003 |
| DLQI, mean (SD) | 12.59 (7.04) | 9.83 (8.34) | 0.095 |
| Number of boils in the past month, mean (SD) | 2.37 (3.06) | 1.38 (2.14) | 0.134 |
| Boil-associated pain score (0−10)b, mean (SD) | 6.56 (3.07) | 4.39 (3.88) | 0.007 |
Categorical variables are number (percentage), continuous variables are mean (standard deviation).
Patients who alleviate HS-related pain had a higher DLQI (12.59 vs. 9.83), p = 0.095 and had a higher mean number of boils in the preceding month (3.2 vs. 2.4), p = 0.134.
No statistically significant differences were seen between the two groups with regard to age, sex, BMI, employment status, and smoking.
DiscussionThis study assessed pain alleviating methods in 134 HS patients. Only few previous studies have assessed pain alleviation and pain alleviating methods in HS,13 and this is the first study to take into account the relationship with age, sex, Hurley stage, BMI, employment status, smoking, psychiatric comorbidity, overall disease distress, DLQI, boil associated pain score, and number of boils in the preceding month.
We found that the majority of the patients (82%) had either, in their attempt to alleviate pain from the inflammatory lesions, drained pus by squeezing manually with their fingers, injected needles, or to a lesser degree used a knife (Table 2). These findings are consistent throughout the Hurley stages, signifying the high prevalence of pain and desperation in patients with HS independent of disease severity and sex. The mean overall disease related distress score and boil-associated pain score in the past month was higher for those with the tendency to alleviate pain in comparison to those who did not. Although not significantly, patients with a higher total DLQI score and higher number of boils in the preceding month were also more likely to alleviate pain. In general, these findings are to be expected as spontaneous pain alleviating behavior has previously been positively correlated to increasing pain intensity.14 Additionally, the psychological aspect of HS is exemplified by the fact that 36% of the included patients have a positive history of previous or current psychological comorbidity, most commonly depression or anxiety (Table 1).
Self-harm non-related to pain-relief was reported by 10.6% of the patients and was reported more often in patients with a history of psychological comorbidity than patients without (20.8% (n = 10) vs. 4.8% (n = 4)). This behavior may reflect sheer frustration and a pronounced desire to control pain sensation by self-inflicted skin lesions.15
Patients also reported using pain-killers (13.4%), showering and application of hot cloths as pain alleviating methods. These numbers may not completely reflect reality, as the numbers could have been higher if the methods were included as specific multiple-choice options. Nevertheless, only 13.4% stated usage of pain killers. This may reflect the potential low efficacy of standard painkillers (e.g. paracetamol) in HS. Previous studies have indicated that only opioids (e.g. Tramadol) appear to reduce HS associated pain significantly.13,16 Moreover, the studies showed that usage of opioids where associated with Hurley stage III patients and may thus indicate that this group of HS patients experience a much higher burden of pain than Hurley stage II – and I patients.
This study assessed pain-alleviating methods in HS patients. Pain alleviation was found to be highly prevalent among the patients independent of disease severity (above 80% across all Hurley stages). While age, sex, BMI, employment status, and smoking did not influence the behavior of patients with HS, patients with Hurley stage III were considerably less regretful of their actions of draining puss from inflamed lesions in comparison to patients with Hurley stage I and II, which may be explained by the much higher burden of pain in these patients.
In aggregate, this study illustrates an important and frequent challenge in HS that may be overlooked and poorly prioritized by dermatologists. The large variation in various alternative and homespun methods used to alleviate pain may reflect how far patients may go to alleviate pain and the intractable nature of HS-associated pain that may not respond to standard pain medication.16 A better understanding and focus on management of pain in HS is needed. Indeed in Hurley stage III patients, a broad collaboration between dermatologists, general practitioners and pain specialists (anesthesiologists) may optimize the management of the HS associated pain.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Ravn Jørgensen AH, Yao Y, Thomsen SF, Ring HC. Métodos referidos por los pacientes para aliviar el dolor asociado a la hidradenitis supurativa. Actas Dermosifiliogr. 2021;112:153–158.