Infantile hemangiomas (IH) are the most common benign tumors of childhood and have a characteristic presentation and distribution. Recently, interest has arisen in a group of IH with minimal or arrested growth of segmental distribution that, when situated in the lower body, are associated with LUMBAR syndrome. We describe a new case of ulcerated segmental IH-MAG associated with LUMBAR syndrome.
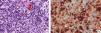
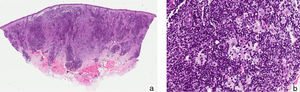
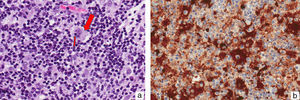
A newborn girl with a diagnosis of lumbar lipomyelomeningocele was evaluated at 20 days of age for a birthmark on the left lower limb and diaper dermatitis. Physical examination revealed a violaceous patch of livedoid appearance affecting the whole lower limb, accentuation of the venous markings on the dorsum of the foot, and lower limb dysmetria (Figure 1, A andB). An ulcer with punched out edges was observed in the perianal region (Figure 1C). On suspicion of cutis marmorata telangiectatica congenita, treatment was only prescribed for the erosive diaper dermatitis. At age 45 days, new skin lesions characterized by shiny red papules were observed in the left inguinal fold, and the perianal ulcer had deteriorated (Figure 2, A andB). Histopathology revealed a vascular proliferation with a prominent endothelium surrounded by fibroblastic tissue with positive immunohistochemistry for CD-31 and GLUT-1, consistent with IH (Figure 2, C-E). Ultrasound examination of the abdomen and pelvis detected hip dysplasia and left pyelectasis, with no other associated hemangiomas. In addition, a left talipes equinovarus deformity was observed. In view of the lumbar lipomyelomeningocele, bone abnormalities, renal manifestations, and the clinical and histopathological evidence of IH, a diagnosis of segmental IH-MAG in the setting of LUMBAR syndrome was made. Treatment was started with oral propranolol at a dose of 2mg/kg/d, with dose escalation to 3mg/kg/d, and local wound care, achieving a favorable clinical response and complete reepithelialization of the perianal ulcer 40 days after starting treatment (Figure 3, A andB). Treatment with propranolol was continued for 6 months and was well tolerated, with no complications.
IH is the most common benign tumor of childhood.1 A definitive diagnosis can be made based on its characteristic clinical appearance and behavior, without the need for additional tests.1,2 However, a minority of IH present unusual behavior, leading to a delay in clinical diagnosis.3 IH-MAG, also known as abortive or reticular hemangioma, is present at birth and is characterized clinically by a network of violaceous telangiectatic appearance or a livedoid pattern that can mimic the precursor macule of IH or even vascular malformations.3,4 However, these lesions do not present the proliferative phase typical of classic IH.3 IH-MAGs do not develop the proliferative component or they do so peripherally, in less than 25% of the surface area of the hemangioma.3–6 Segmental IHs cover a specific skin territory; the most well known are facial IHs, closely associated with PHACES syndrome (posterior fossa, arterial, cardiovascular, ocular and midline raphe malformations).7,8 Likewise, segmental IHs in the lower body are associated with LUMBAR syndrome, which consists of urogenital abnormalities, ulceration, myelopathy, bone deformities, anorectal, arterial, and renal anomalies, and is considered to be analogous with PHACES syndrome.8 Recently, 2 cases of segmental IH-MAG have been described in the setting of PHACES syndrome.8
Histopathologically, a proliferation of vessels with a prominent endothelium and dilated lumen are observed in the superficial dermis. These vessels are positive for CD-31 (an endothelial cell marker) and GLUT-1 (erythrocyte-type glucose transporter protein), a specific marker of IH.5
The most common complication of IH is ulceration, occurring in 15% to 25%.1,2 However, in IH-MAG in the perianal region the risk of ulceration can be as high as 80% due to constant friction, the presence of microbial flora, and exposure to irritant substances in the urine and feces.3,6,7 This ulceration can mask IH, simulating other diseases in the diaper region,7 as occurred in our patient. This form of ulceration was also observed in the 2 cases of segmental IH-MAG described in PHACES syndrome.8
Ulcer care is a fundamental part of treatment, preventing superinfection and controlling pain. Oral therapy with the β-blocker propranolol is controversial in segmental IH and in PHACES syndrome because of the association with arterial anomalies. However, the possibility of severe vasoconstriction leading to acute hypoperfusion has been shown to be avoided by a stepped initiation of propanolol treatment, and this has been extrapolated to its use in LUMBAR syndrome.6,9
We have described a new case of LUMBAR syndrome associated with ulcerated segmental IH-MAG that was successfully treated with propranolol. We have drawn attention to the clinical features and to the need for early diagnosis due to its possible syndromic associations.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Sandro Casavilca-Zambrano of the Pathology Department of Instituto Nacional de Enfermedades Neoplásicas in Lima, Peru, for his support in the histopathology study.
Please cite this article as: Calderón-Castrat X, Peceros-Escalante J, Velásquez F, Lipa-Chancolla RM, Ballona R. Hemangioma infantil de crecimiento mínimo o detenido segmentario en un síndrome LUMBAR. Actas Dermosifiliogr. 2017;108:474–476.