Prurigo nodularis (PN) is a chronic, difficult-to-treat pruriginous disease that can have a significant impact on a patient’s quality of life. It is a neurodermatitis in which the itch-scratch cycle perpetuates the nodular lesions. The cause is unknown, but the condition is associated with other skin diseases (mainly atopic dermatitis), systemic diseases (liver and renal failure and infections), neurologic and psychiatric disorders, and neoplasms.1
Larson et al2 recently published the findings of the largest study to date on the association between PN and neoplasms. They included 695 diagnosed patients (51.6% women) between the ages of 40 and 69 years, comparing them to more than 2 million individuals with similar characteristics. The authors found that 17.8% of the patients with PN had some type of neoplasm and that malignancy was 4-fold more likely among those with PN than in the control individuals (odds ratio [OR], 4.54; 95% CI, 3.74–5.52). Skin tumors were the most common type of neoplasm (in 47%); the majority were basal cell carcinoma, followed in frequency by squamous cell carcinoma and melanoma. Solid organ tumors (in 32% of the patients) were mainly genital (in women), in the lung, or in the digestive tract. Blood neoplasms were found in 21% (mainly non-Hodgkin lymphoma, multiple myeloma, or primary cutaneous lymphoma). The patients with PN had significantly higher risk for skin cancer (OR, 10.94; 95% CI, 8.01–14.96), primary cutaneous lymphoma (OR, 24.82; 95% CI, 7.96–77.46), and female genital neoplasia (OR, 11.00; 95% CI, 4.90–24.68), among other malignant tumors. The pathophysiologic mechanism for the association between neoplasia and PN is unknown, but it may be related to a proinflammatory state.
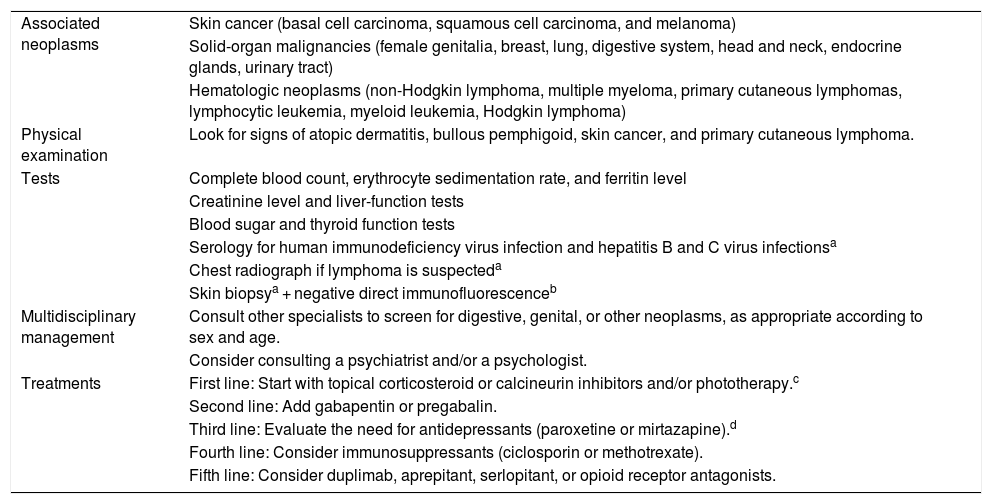
Given the strong association between PN and tumors in patients in the aforementioned study,2 a high index of suspicion is recommended. Also recommended is careful examination of skin and mucosal tissues and additional tests (Table 1) following a multidisciplinary approach; screening for neoplasms according to sex and age should be included.1,2
Management of PN: Associated Neoplasms, Physical Examination, Recommended Additional Tests, and Treatments
| Associated neoplasms | Skin cancer (basal cell carcinoma, squamous cell carcinoma, and melanoma) |
| Solid-organ malignancies (female genitalia, breast, lung, digestive system, head and neck, endocrine glands, urinary tract) | |
| Hematologic neoplasms (non-Hodgkin lymphoma, multiple myeloma, primary cutaneous lymphomas, lymphocytic leukemia, myeloid leukemia, Hodgkin lymphoma) | |
| Physical examination | Look for signs of atopic dermatitis, bullous pemphigoid, skin cancer, and primary cutaneous lymphoma. |
| Tests | Complete blood count, erythrocyte sedimentation rate, and ferritin level |
| Creatinine level and liver-function tests | |
| Blood sugar and thyroid function tests | |
| Serology for human immunodeficiency virus infection and hepatitis B and C virus infectionsa | |
| Chest radiograph if lymphoma is suspecteda | |
| Skin biopsya + negative direct immunofluorescenceb | |
| Multidisciplinary management | Consult other specialists to screen for digestive, genital, or other neoplasms, as appropriate according to sex and age. |
| Consider consulting a psychiatrist and/or a psychologist. | |
| Treatments | First line: Start with topical corticosteroid or calcineurin inhibitors and/or phototherapy.c |
| Second line: Add gabapentin or pregabalin. | |
| Third line: Evaluate the need for antidepressants (paroxetine or mirtazapine).d | |
| Fourth line: Consider immunosuppressants (ciclosporin or methotrexate). | |
| Fifth line: Consider duplimab, aprepitant, serlopitant, or opioid receptor antagonists. |
Abbreviation: PN, prurigo nodularis.
There is limited evidence available on the treatment of PN given that fewer than 10 clinical trials have been published, and most are small.3 Good outcomes have been described after treatment with topical corticosteroids and calcineurin inhibitors, phototherapy, thalidomide (though its safety profile is poor), antiepileptics or anticonvulsives (pregabalin, gabapentin, or amitriptyline), ciclosporin, and methotrexate. A recent retrospective study of 39 patients with refractory PN showed an objectively measured response to methotrexate in 90% at 3 and 12 months, and complete resolution was observed at 12 months in 57%.4 However, 12% of the patients had to stop treatment due to such adverse effects as transaminitis, pneumonitis, or gastrointestinal symptoms, among other events.4 In our patients, we have also observed good responses to treatment with methotrexate and pregabalin.
Emerging therapies include neurokinin 1 receptor antagonists such as aprepitant and serlopitant, the focus of an as-yet unpublished phase-3 trial; interleukin-31 inhibitors such as nemolizumab, currently being studied in a phase-2 trial; and opioid receptor agonists/antagonists such as nalbuphine. There is also the interleukin-4 inhibitor dupilumab.5
PN may be associated with neoplasms. A high index of clinical suspicion is necessary so that appropriate additional screening tests can be ordered. Treatment is complex, and clinical evidence is still limited.
Please cite this article as: Serra-García L, Morgado-Carrasco D. FR-Prurigo nodular: asociación con neoplasias, pruebas complementarias y nuevos tratamientos. Actas Dermosifiliogr. 2021;112:663–664.