UV radiation is the main modifiable risk factor in the development of skin cancer, both melanoma (which is more closely related to intense intermittent sun exposure and sunburns) and nonmelanoma skin cancer (NMSC) (which follows a dose-dependent pattern). However, the question of whether restriction of sun exposure would be justified in patients with skin cancer has been a subject of debate because a growing body of scientific evidence suggests that insufficient exposure to UV radiation is associated with risks to overall health and even life expectancy.1
In a recent study, a Swedish cohort of more than 20 000 women were categorized in 3 groups according to their degree of sun exposure.2 The authors found that, as a result of cardiovascular mortality and other noncancer causes, the mortality rate was twice as high in women who avoided sun exposure as in women with a higher degree sun exposure. They concluded that insufficient sun exposure was a risk factor for death of the same magnitude as smoking. The study controlled for possible confounding factors such as age, smoking, exercise, education level, economic status, and marital status. Cancer mortality increased with greater sun exposure and could be explained by increased longevity in this group. The study had limitations that prevent us from extrapolating the results to the general population. Future studies that include both sexes and a larger geographic area are needed.
UV radiation is involved in vitamin D synthesis. Multiple studies have linked UV radiation deficiency to numerous chronic diseases, mainly cardiovascular diseases, autoimmune diseases, skeletal diseases, diabetes, and colorectal cancer. These studies suggest that maintaining vitamin D levels of at least30ng/mL could reduce overall mortality by half.3
UV radiation has other mechanisms of action that are independent of vitamin D, including an antihypertensive effect caused by direct arteriolar vasodilation and an increase in nitric oxide,4 as well as antidepressant and anxiolytic effects.
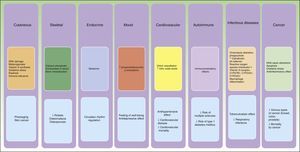
Although dermatologists are responsible for treating and preventing skin cancer, we must do so with a holistic view of the patient. We should recognise the benefit of sun exposure in terms of life expectancy and diseases with high mortality rates—such as hypertension, diabetes mellitus, cardiovascular disease, and osteoporotic hip fracture—even if it means an increased risk of skin cancer (Fig. 1), which, despite its prevalence, has a much lower impact on mortality.5
From a public health perspective, it makes sense to educate people about the harmful effects of both excessive and insufficient sun exposure. In routine practice, dermatologists should recommend to most patients adequate sun exposure as part of a healthy lifestyle, together with a varied diet, and consider supplementation in cases of vitamin D deficiency. Restriction of sun exposure should be reserved for patients with diseases associated with a high risk of skin cancer such as immunodeficient patients, transplant recipients, and patients with DNA repair-deficiency disorders such as xeroderma pigmentosum.
Please cite this article as: Monserrat-García MT, Ortíz-Prieto A, Martín-Carrasco P, Conejo-Mir-Sánchez J. FR- Exposición solar insuficiente y mortalidad global: ¿debemos recomendar o desaconsejar la exposición solar a nuestros pacientes?. Actas Dermosifiliogr. 2017;108:257–258.