Pilomatricoma is the second most common skin tumor in childhood and youth and it has a broad differential diagnosis. The main objective of the present study was to determine the incidence of pilomatricomas in our hospital and to analyze the following variables: patient age and sex, tumor site, symptoms, previous trauma, clinical diagnosis, associated diseases, number of cases of multiple tumors, ultrasound findings, anesthetic and surgical techniques, and postoperative complications.
Material and methodThis was a retrospective study of the pilomatricomas surgically excised between January 2004 and December 2012 and registered in the database of the pathology department of our hospital.
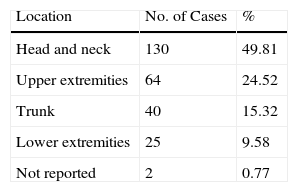
ResultsWe found 261 pilomatricomas in 239 patients (120 female and 119 male) between 1 and 83 years of age (mean age, 26.4 years). The most common presentation was as a firm subcutaneous nodule, which was asymptomatic in 82% of cases. Tumors most commonly affected the head and neck (49.81%). Preoperative diagnosis was correct in 54.4% of cases, concomitant diseases were present in 59 cases, and 7 patients reported a history of trauma in the area of the tumor. There were 17 cases of multiple tumors, 1 case in a patient with familial disease and 2 in patients with Steinert disease. Soft-tissue ultrasound was performed on 57 lesions; images were compatible with pilomatricoma in 48 cases. Tumor excision was performed under local anesthesia in 185 cases and under local and general anesthesia in 76. The postoperative complications were hypertrophic scarring and wound dehiscence (1 case each).
ConclusionsThis was a retrospective study with the largest series recorded in Spain and with one of the highest incidences. In addition, we report on variables not described in other studies.
El pilomatricoma es la segunda neoformación cutánea más frecuente en la infancia y la juventud, con un amplio diagnóstico diferencial. El objetivo principal del estudio fue determinar la incidencia de pilomatricomas en nuestro hospital y sus características en relación con: edad, sexo, localización, síntomas, traumatismo previo, diagnóstico clínico, enfermedades asociadas, casos múltiples, características ecográficas, tratamiento quirúrgico y técnica anestésica y complicaciones posteriores.
Material y métodoSe recogieron de forma retrospectiva los pilomatricomas extirpados quirúrgicamente en nuestro hospital de enero de 2004 a diciembre de 2012 a partir de la base de datos de anatomía patológica.
ResultadosSe estudiaron 261 pilomatricomas en 239 pacientes, 120 eran mujeres y 119 varones de edades comprendidas entre 1 y 83 años, con una media de 26,4 años. La forma de presentación más frecuente fue como un nódulo firme, subcutáneo, asintomático en el 82% de los casos. La localización más frecuente fue la cabeza y el cuello (49,81%). El diagnóstico clínico preoperatorio fue acertado en el 54,4%. Cincuenta y nueve pacientes tenían otras enfermedades y 7 recordaban traumatismo previo en la zona. Se registraron 17 casos múltiples, uno familiar, y 2 en pacientes con enfermedad de Steinert. En 57 lesiones se realizó ecografía de partes blandas, con imágenes compatibles con pilomatricoma en 48. Ciento ochenta y cinco pilomatricomas se extirparon con anestesia local y 76 con anestesia local y general. Como complicaciones posquirúrgicas hubo un caso de cicatriz hipertrófica y otro de dehiscencia.
ConclusionesEl nuestro es el estudio retrospectivo que recoge el mayor número de casos en nuestro país y uno de los que comunica mayor incidencia de casos. Además, se estudian variables no recogidas en otras series.
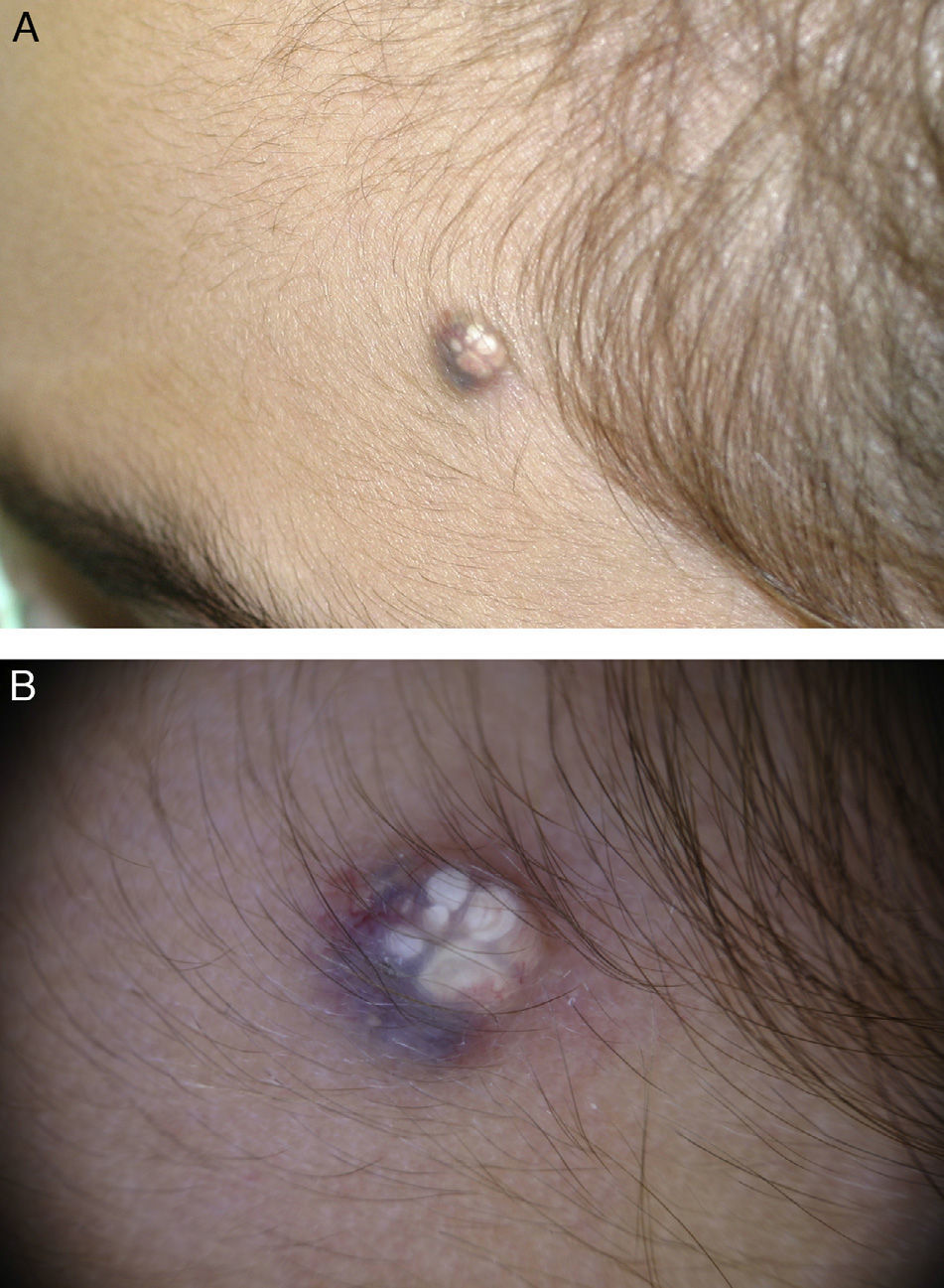
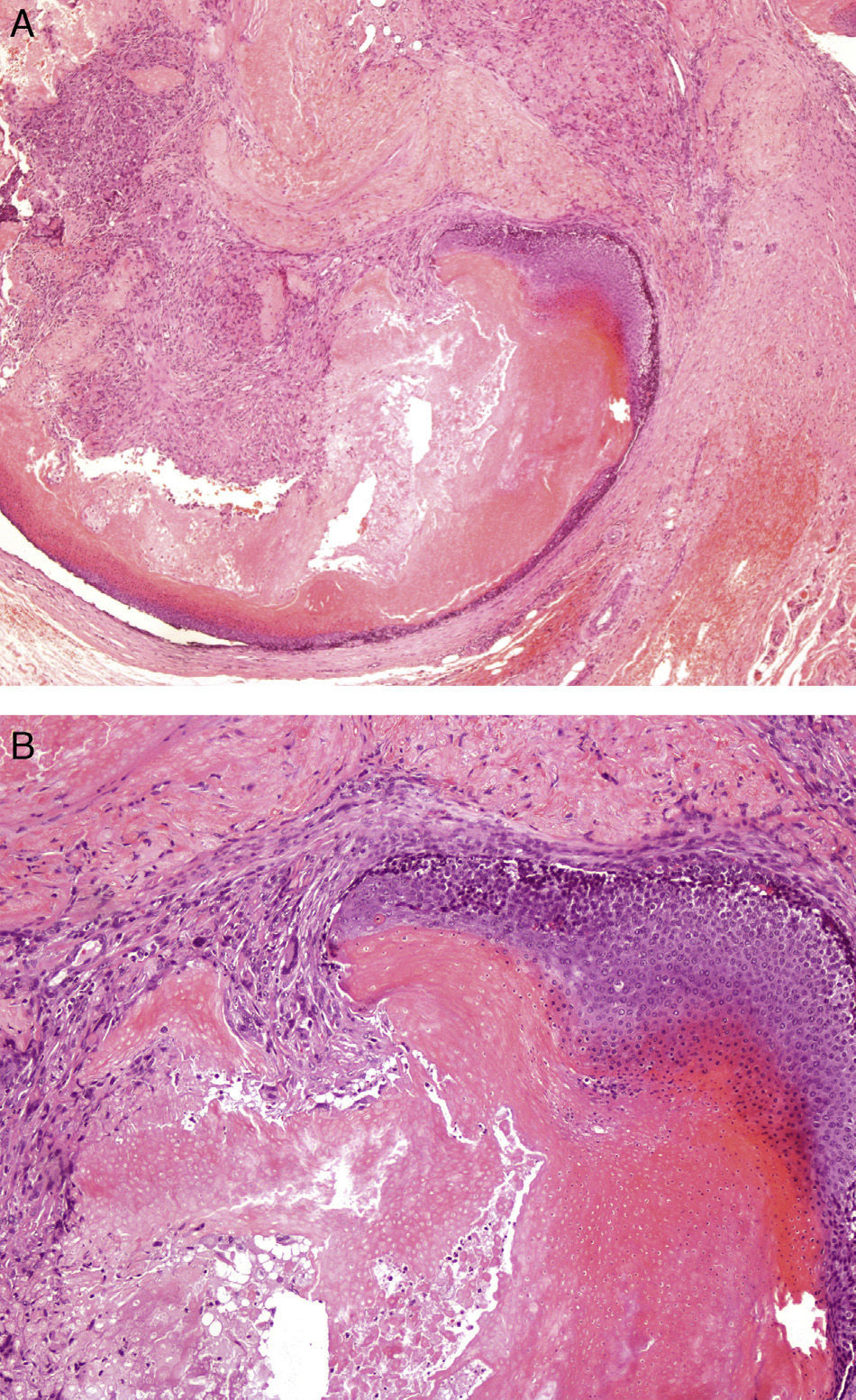
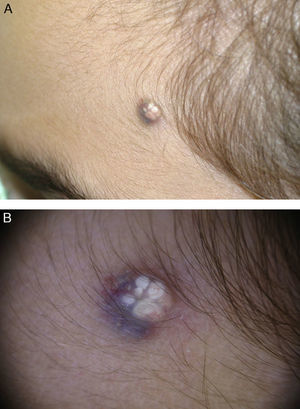
Pilomatricoma, also known as pilomatrixoma and trichomatricoma, is a benign tumor that differentiates towards the hair matrix, cortex, and epithelial sheath. It is the second most common benign skin tumor in the first 2 decades of life after epidermal cyst, but despite its frequency it has a broad clinical differential diagnosis.1 It has been described more frequently in females and is most commonly located on the head and neck, followed by the trunk and the extremities. The most common clinical presentation is a firm, movable subcutaneous lesion with a lobulated surface; the overlying skin may acquire a red or bluish hue.2 The tent sign is a characteristic feature of pilomatricoma and refers to the firm, angulated shape formed when the overlying skin is stretched between the fingers.3 Another recently described sign, the skin crease sign, refers to the skin crease or fold that is formed when the edges of the tumor are gently pressed between the thumbs perpendicularly to the tension lines of the skin.4 Pilomatricoma typically presents as a solitary lesion, and while no inheritance patterns have been described, there have been reports of familial cases.5,6 Multiple lesions (≥2) have been reported in between 2% and 3.5% of patients, depending on the series. Multiple pilomatricomas appear to be more common in patients with systemic disease and diverse syndromes, and may be indirect markers of underlying disease. Despite its frequency, pilomatricoma is clinically underdiagnosed and the differential diagnosis includes numerous benign skin lesions (epidermoid and dermoid cysts, swollen lymph nodes, foreign body granuloma, molluscum contagiosum, xanthogranuloma, and adnexal subcutaneous tumors) and malignant lesions (basal cell carcinoma and melanoma).7 Highman and Ogden8 provided the first histologic description of pilomatricoma in 1944, and referred to the characteristic anucleate cells in pilomatricoma known as ghost or shadow cells. Histologically, pilomatricoma appears as a well-circumscribed tumor with a mixed population of basaloid epithelial cells and shadow cells in the center of the lesion and a fibroblastic mesenchymal component.9 Foci of calcification are common and ossification may be seen, but much less frequently.10 Diagnosis is confirmed by histology, but clinical suspicion can be supported preoperatively by imaging studies and soft-tissue ultrasound in particular. Ultrasound scans show a hyperechoic and isoechoic nodule with a peripheral halo and a posterior shadow.11 Computed tomography and magnetic resonance imaging have also been used in some cases. The role of fine-needle aspiration is unclear due to the high likelihood of false positives, and most authors believe that its effectiveness depends on the experience of the person performing the procedure.12
Pilomatricoma is, by definition, a benign tumor, but there have been reports of malignant transformation and even metastasis, although it is believed that these cases were primarily malignant (i.e., pilomatricoma carcinoma).13 Treatment is surgical, but there is no consensus on optimal excision margins, surgical technique, or age for surgery in young patients. Spontaneous remission has not been reported, and up to 3% to 4% of cases recur after surgery, although recurrence in such cases is probably due to incomplete excision.
The main aim of the present study was to determine the frequency of solitary and multiple pilomatricoma in our hospital after noticing what appeared to be a high rate of cases. A second aim was to describe the clinical and ultrasound features of these lesions.
Material and MethodsThis was a descriptive retrospective study of all pilomatricomas surgically removed at Hospital Universitario de Fuenlabrada in Madrid, Spain, which serves a population of 250 000 inhabitants. We studied all cases registered in the database of the pathology database in our hospital between January 2004 and December 2012.
The variables analyzed were patient sex, age at diagnosis, tumor location, associated symptoms, a clear history of trauma, preoperative clinical diagnosis, concomitant diseases, multiple and familial cases and possible associations, ultrasound and histologic features, surgical and anesthetic technique, and subsequent complications.
ResultsWe identified 261 surgically excised pilomatricomas in 239 patients. Most of the patients (83.68%) were from the dermatology department. The rest had been evaluated and operated on in other departments, namely the general surgery department (34 patients, 14.23%), the ear, nose, and throat department (4 patients, 1.67%), and the ophthalmology department (1 patient, 0.42%).
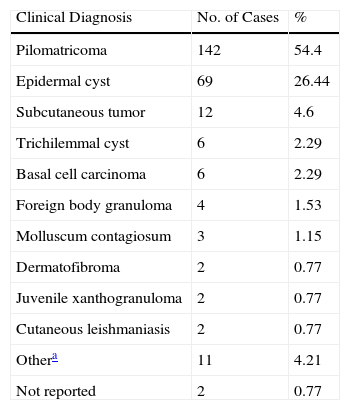
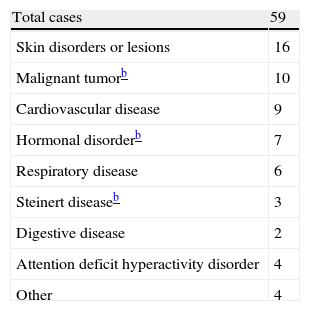
Of the 239 patients, 120 (50.21%) were female and 119 (49.79%) were male. Age at diagnosis ranged from 1 to 83 years, with a mean age of 26.4 years; 46.03% of the patients were aged 16 years or younger. The most common tumor location was the head and neck (49.81% of cases), followed by the upper extremities (24.52%), the trunk (15.32%), and the lower extremities (9.58%) (Table 1). The most common clinical presentation was a firm subcutaneous nodule that was asymptomatic in 82% of cases (Fig. 1). The preoperative clinical diagnosis was pilomatricoma in 54.4% of cases; the second most common clinical diagnosis was epidermal cyst (26.44%). Many clinical entities, both benign and malignant, were initially suspected; these are shown together with the corresponding number of cases in Table 2. Fifty-nine of the 239 patients had a concomitant disease: 16 patients had another skin condition (multiple melanocytic nevi and pigmented lesions under follow-up in 5 cases, acne in 2, basal cell carcinoma in 2, and psoriasis, acanthosis nigricans, lichen planus, genital lichen sclerosus, multiple lipomatosis, ptosis, sebaceous nevus, and multiple common warts); 10 patients had a malignant tumor (breast cancer in 2 cases and melanoma, pheochromocytoma, and cancer of the colon, endometrium, cervix, prostate, pancreas, and liver); 9 patients had cardiovascular disease (ischemic heart disease, chronic venous insufficiency, aortic stenosis, temporal arteritis, hypertension, and diabetes); 7 patients had a hormonal disorder (hypothyroidism, low height, morbid obesity, polycystic ovary syndrome, premature pubarche, overgrowth syndrome, and hyperandrogenism); 6 patients had respiratory disease (asthma, obstructive sleep apnea syndrome, and chronic obstructive lung disease); 3 patients had Steinert disease; 2 patients had a digestive disease (hepatopathy and celiac disease); 2 patients had attention deficit hyperactivity disorder; and there were isolated cases of vasovagal syncope, migraine, arthrosis, and renal cysts (Table 3). Seven patients reported prior trauma at the site of the tumor (2 recalled injury with a pencil tip, 1 recalled an insect bite/sting, and 1 recalled vaccination). There were 20 cases of multiple pilomatricoma (8.39%); 1 patient had 4 lesions, 4 patients had 3 lesions, and 15 patients had 2 lesions. The patient with 4 tumors was being evaluated for overgrowth syndrome and had a sister with a confirmed case of pilomatricoma that had been surgically removed. Two of the other patients with multiple pilomatricoma had confirmed Steinert disease (Fig. 2) and 1 had endometrial carcinoma. Three of the 239 patients had a history of pilomatricoma at another site that had been excised at a different hospital; the corresponding pathology reports were included in the database. Fifty-seven (21.84%) of the 261 lesions were examined by soft-tissue ultrasound, which revealed images consistent with pilomatricoma in 48 cases (Fig. 3). The other 9 tumors exhibited nonspecific or incompatible features. Histologically, most of the tumors had typical features of pilomatricoma (Fig. 4). Additionally, there were 5 hybrid cysts (epidermal cyst and pilomatricoma in the same specimen), 1 anetodermic pilomatricoma, which was diagnosed preoperatively, 1 case of ossification, 1 pilomatricoma with acanthotic seborrheic keratosis, and 1 follicular cyst with trichilemmal-epidermal-like areas and pilomatricoma. There were no cases of pilomatrical carcinoma or signs of malignant transformation in any of the lesions.
Preoperative Clinical Diagnosis for 261 Surgically Excised Pilomatricomas.
| Clinical Diagnosis | No. of Cases | % |
| Pilomatricoma | 142 | 54.4 |
| Epidermal cyst | 69 | 26.44 |
| Subcutaneous tumor | 12 | 4.6 |
| Trichilemmal cyst | 6 | 2.29 |
| Basal cell carcinoma | 6 | 2.29 |
| Foreign body granuloma | 4 | 1.53 |
| Molluscum contagiosum | 3 | 1.15 |
| Dermatofibroma | 2 | 0.77 |
| Juvenile xanthogranuloma | 2 | 0.77 |
| Cutaneous leishmaniasis | 2 | 0.77 |
| Othera | 11 | 4.21 |
| Not reported | 2 | 0.77 |
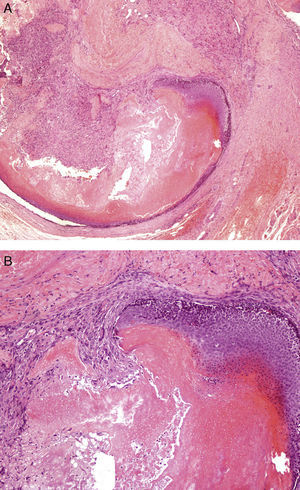
Well-circumscribed tumor with a mixed epithelial component composed of basaloid and shadow cells in the center of the lesion, and a peripheral mesenchymal component formed by fibroblastic cells. A, Hematoxylin-eosin, original magnification ×40. B, Hematoxylin-eosin, original magnification ×100.
In total, 185 tumors (70.88%) were excised using local anesthesia and 76 (29.12%) using a combination of local and general anesthesia or sedation; 1 patient died from anesthesia-related complications. Postsurgical complications included hypertrophic scarring (1 case) and dehiscence of the surgical wound that required no further action (1 case). There have been no reports of recurrence to date; just 1 patient needed additional surgery on a lesion on the wing of the nose that had been incompletely excised by curettage following a clinical suspicion of molluscum contagiosum. The lesion was completely excised in the second operation.
DiscussionIn 1880, Malherbe and Chanantais14 described a group of tumors they believed were derived from the sebaceous gland and that they called calcifying epitheliomas of sebaceous glands. In 1961, Forbis and Helwig15 studied 228 cases of the same tumor and proposed the name pilomatricoma because they concluded that the tumor was derived from the matrix of the hair.
Pilomatricoma is a very common skin tumor, so much so that the high rates of undiagnosed cases reported in the literature are very surprising.7 Most of the reports in the literature describe a similar presentation: a firm subcutaneous nodule, located preferentially on the head and neck in female patients that appears in first 2 decades of life.
In 1943, Cordiviola and Quevedo16 described a special anetodermic clinical form consisting of a firm subcutaneous tumor covered by thin, folded skin.
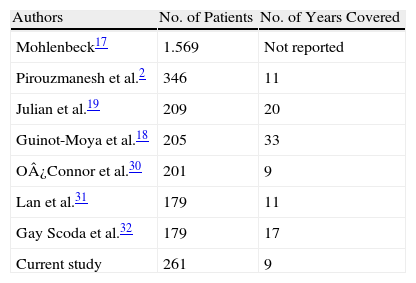
Table 4 lists the studies that have analyzed series of over 100 pilomatricomas. The largest series published to date is that of Moehlenbeck17 from 1973, which described 1569 pilomatricomas, including 170 cases seen at the author's hospital. The most common tumor location in our series, coinciding with previous reports, was the head and neck. Unlike other studies, however, we found no significant differences for sex. Although pilomatricoma shows a predilection for the female sex, Guinot-Moya et al.18 found that these tumors were slightly more common in male patients. A prior history of recognizable trauma (e.g., insect bite/sting, vaccine) at the site of the tumor has been reported in up to 9% of patients,2,18 although the association could be coincidental given the high frequency of pilomatricoma.
As already mentioned, even though pilomatricoma is very common, the tumor is only diagnosed preoperatively in 6% to 29% of cases.2,19 This low diagnostic rate could possibly be explained by the fact that most series have been published in journals outside the field of dermatology. In our series, 54.4% of pilomatricomas were correctly diagnosed prior to surgery; this rate is high compared with reports in the literature and can probably be explained by the fact that most patients were initially evaluated by the dermatology department.
The diagnostic role of soft-tissue ultrasound in pilomatricoma is growing. In a series of 124 pilomatricomas reported by Solivetti et al.,11 25.8% of the tumors were evaluated by ultrasound. The tumor is viewed as a hyperechoic or isoechoic nodule with a peripheral halo and a posterior shadow. Solivetti et al. described 5 characteristic ultrasound patterns of pilomatricoma, and recognized the importance of ultrasound as a preoperative diagnostic tool in this setting. In our series 57 tumors (21.84%) were examined by soft-tissue ultrasound, and the images were consistent with pilomatricoma in 48 cases (84.21%) and inconsistent or nonspecific in 9 cases; these results are possibly related to varying levels of experience and the use of different criteria, as not all the examinations were performed and reported by the same radiologist.
Histology showed that most of the lesions in our series were well-circumscribed subepidermal tumors composed of a mix of basaloid and shadow cells, fibroblastic cells without atypia, and a variable amount of calcified material. Although hybrid cysts are rare in pilomatricoma, there have been some reports of cysts containing one or more components of the pilosebaceous unit.20 In such cases, there is a mixed variable component with evident transition between the 2 areas; this is a different concept from coexisting or collision tumors. Our findings support reports to date that ossification, anetodermic pilomatricomas, and hybrid cysts are rare.5,10,20
The highest reported rate of multiple pilomatricomas in large series (<100 cases, Table 4) is 3.5%.17 In our series, 8.39% of patients had multiple pilomatricomas; 1 of the patients had 4 lesions and also had a first-degree relative with a confirmed diagnosis of pilomatricoma. Multiple pilomatricoma has been described in Steinert disease (myotonic dystrophy), Gardner syndrome, Turner syndrome, Sotos syndrome,21 Rubinstein-Taybi syndrome, medullary thyroid carcinoma, and sarcoidosis.22 More recently, it has also been described in isolated cases of trisomy syndromes, cerebral glioblastoma,23 celiac disease,24 21-hydroxylase deficiency,25 and Kabuki syndrome.26 Concerning the etiology and pathogenesis of pilomatricoma, several studies have demonstrated the presence of mutations in the β-catenin pathway, a signaling protein involved in the development of the hair follicle; these studies have shown that the mutations favor the development of pilomatricoma and other adnexal tumors, and may also affect other cancer-related genes, possibly explaining why malignant tumors are more common in patients with multiple pilomatricomas.27–29
Two patients with multiple pilomatricoma in our series had Steiner syndrome. The presence of multiple lesions in a patient with overgrowth syndrome and another with endometrial carcinoma has not been previously reported.
The association between solitary pilomatricoma and other diseases has not been previously studied. The most common concomitant diseases in our series were other skin disorders, malignant tumors, and cardiovascular disease. However, given the high incidence of both pilomatricomas and these diseases, it is easy to assume that the association is purely coincidental.
Pilomatricoma is treated by surgical excision, but there is no consensus on the optimal age at which surgery should be performed in children, or on the most appropriate technique and margins. Our patients underwent simple excision without wide margins. The choice of anesthetic technique was governed by clinical criteria, including medical history, concomitant medication, age, and tumor characteristics (e.g., location and size). One of the girls in our series died as a result of anesthetic complications in the postoperative period. She had a progressively growing tumor and the results of the ultrasound evaluation had been inconclusive. This is the first report of postsurgical complications in a patient with pilomatricoma.
The main limitations of our study are related to its retrospective design, particularly in terms of the lack of uniformity in the collection of clinical data, probably due to the large number of physicians involved. In many cases, for example, there was no information on prior trauma at the tumor site, possibly because the physician did not ask this question or note down the answer. Furthermore, the true frequency of pilomatricomas in our hospital is higher than that reported as our study design excluded patients with a clinical diagnosis of pilomatricoma who had not undergone surgery.
In conclusion, this retrospective study of pilomatricomas is the largest to date in Spain and considering the number of years studied and the size of the population served by our hospital (250 000), we have reported one of the highest incidence rates of pilomatricoma. We would also like to stress the high proportion of lesions evaluated by ultrasound and the considerable number of patients with multiple pilomatricoma. To our knowledge, this is the first study to describe concomitant diseases, surgical treatment, anesthetic techniques, and postoperative complications in patients with pilomatricoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Hernández-Núñez A, Nájera Botello L, Romero Maté A, Martínez-Sánchez C, Utrera Busquets M, Calderón Komáromy A, et al. Estudio retrospectivo de pilomatricomas: 261 tumores en 239 pacientes. Actas Dermosifiliogr. 2014;105:699–705.