A 42-year-old woman with a past history of subclinical hypothyroidism of autoimmune origin, consulted for skin lesions that had developed progressively over 3 years in the axillas and groin. She complained about the past occasional pruritus with sweating. The patient was not aware of any similar lesions among her relatives.
Physical ExaminationGrayish-brown macules measuring a few millimeters in diameter were observed in both axillas (Fig. 1). The lesions were not infiltrated and in some areas they were grouped in a reticulate pattern a reticulate. Similar lesions were observed in the groin (Fig. 2). The rest of the physical examination, including the skin adnexa and mucosas, revealed no relevant findings.
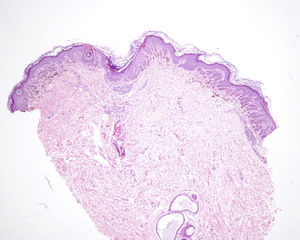
HistopathologyA biopsy of one of the lesions showed mild hyperkeratosis of the epidermis, with elongation and hyperpigmentation of the rete ridges, occasional small corneal cysts, and the presence of melanophages in the superficial dermis (Fig. 3).
What Is Your Diagnosis?
DiagnosisDowling-Degos disease (DDD).
Clinical Course and TreatmentThe patient was discharged with no treatment.
CommentDDD or reticular pigmented anomaly of the flexures is a rare genodermatosis of autosomal dominant inheritance with variable penetrance. Manifestations arise between 30 and 40 years of age. It was described by Behçet as a variant of acanthosis nigricans, from which it was differentiated by Dowling and Freudenthal in 1938; it was called dermatose pigmentaire réticulée des plis by Degos and Ossipowski, and finally named Dowling-Degos disease in 1978 by Jones and Grice.
Genetic alterations described in DDD include mutation and loss of function of the keratin 5 gene,1 changes at chromosome 17p13.3, and mutations of POFUT12 and POGLUT1,3 which encode the proteins O-fucosyltransferase1 and O-glucosyltransferase1, implicated in the NOTCH pathway.
The disease presents as hyperpigmented macules with a reticulate pattern in the axillas and groin. The macules can spread to other skin folds and may be associated with comedo-like lesions on the back and neck, pitted pinpoint perioral scars, epidermal cysts, hidradenitis suppurativa, squamous cell carcinomas, and multiple keratoacanthomas.4 Histopathology shows orthokeratosis or hyperkeratosis, thinning of the suprapapillary epithelium, elongation of the rete ridges, hyperpigmentation of the basal layer, and follicular cysts. A perivascular lymphohistiocytic infiltrate can be observed in the papillary dermis.4 The differential diagnosis should include acanthosis nigricans and granular parakeratosis, as well as various entities considered by some authors to be part of the spectrum of a single disease: Galli-Galli disease (GGD), reticulate acropigmentation of Kitamura (RAK), Haber syndrome (HS), reticulate acropigmentation of Dohi (ARD) or dyschromatosis symmetrica hereditaria (DSH), and dyschromatosis universalis hereditaria (DUH).4 In addition to the findings described for DDD, we also find atrophic acral hyperpigmented macules and palmar pitting or fissures in RAK, rosacea-like facial erythema and hyperkeratotic pigmented papules on the trunk in HS, and hyperpigmented and hypopigmented macules on the dorsum of the hands and feet in DSH or ARD and widespread in DUH. DDD and GGD are indistinguishable based on clinical findings and are differentiated by the presence of acantholysis on histopathology.5 The later onset and the absence of other clinical findings will differentiate DDD from other diseases that cause early-onset reticulate hyperpigmentation: Naegeli-Franceschetti-Jadassohn syndrome, congenital dyskeratosis, and dermopathia pigmentosa reticularis.
From a histologic point of view, DDD must be differentiated from acanthosis nigricans and seborrheic keratosis with an adenoid pattern. Involvement of the infundibulum of the hair follicle is a characteristic finding in DDD but is not seen in the other 2 conditions.6 DDD has been treated with hydroquinone, adapalene, tretinoin, and topical corticosteroids, with variable results. Another option is the Er: YAG laser treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank Dr Alberto Romero Maté.
Please cite this article as: González-Olivares M, Nájera L, García-Donoso C. Hiperpigmentación reticulada en pliegues. Actas Dermosifiliogr. 2016;107:853–854.