Involuntary craniofacial erythema, or blushing, due to autonomic dysfunction can be a cause of psychological distress. Although anecdotal reports have suggested that pharmacologic treatments or cognitive behavioral therapy can be used to treat the condition, no rigorous analyses of their efficacy have been reported.
ObjectivesTo assess the efficacy of video-assisted thoracoscopic sympathectomy and to study phobic anxiety and other personality traits in a series of patients with involuntary facial blushing.
Materials and methodsWe carried out a retrospective observational study of patients treated with bilateral video-assisted thoracoscopic sympathectomy for blushing over a 7-year period (2001-2008). All the patients were treated by a dermatologist, a psychologist, and a thoracic surgeon and were informed of the predicted outcomes.
ResultsA total of 204 patients with a mean age of 34 years (range, 15-67 years) were included; the numbers of males and females were similar. Only 10% had unpredicted outcomes; in such cases, either the procedure was insufficiently effective or postoperative reflex sweating developed (and was considered serious in 2%). There were no deaths and only 1 case of transient Horner syndrome. Video-assisted thoracotomy was required for pleural symphysis in 1 patient; 5 patients developed pneumothorax, but only 1 of them required pleural drainage.
ConclusionsVideo-assisted sympathectomy is a safe, effective and definitive treatment for disabling blushing. Anxiety that is detected before surgery is a reaction to blushing rather than a cause of it.
El blushing es una disautonomía que afecta al área craneofacial y se manifiesta en forma de rubor facial que puede conllevar trastornos psíquicos. La eficacia del tratamiento farmacológico y de la terapia cognitivo conductal es anecdótica y no hay estudios rigurosos que demuestren su validez.
ObjetivoEvaluar la efectividad de la simpaticotomía videotoracoscópica, así como las variables de personalidad y ansiedad fóbica en una serie de pacientes cuyo motivo de consulta fue el enrojecimiento facial incontrolable (blushing).
Material y métodosSe realizó un estudio observacional retrospectivo durante un periodo de 7 años (2001-2008) en los pacientes afectos de blushing a los que se les efectuó simpaticotomía torácica bilateral videotoracoscópica. Todos los pacientes fueron visitados por un dermatólogo, un psicólogo y un cirujano torácico e informados de los efectos secundarios y expectativas de la intervención.
ResultadosDoscientos cuatro pacientes, con una distribución por sexos similar y una edad media de 34 años (rango: 15-67) fueron incluidos en el estudio. Solamente un 10% tuvo un resultado no esperado de la invervención, debido a la poca eficacia o a un excesivo sudor reflejo posquirúrgico que fue considerado grave en un 2% de los casos. No hubo mortalidad y solo un caso de síndrome de Horner transitorio. Se realizó una toracotomía videoasistida por sínfisis pleural y 5 pacientes desarrollaron un neumotórax, de los cuales uno requirió drenaje pleural.
ConclusionesLa simpaticotomía videotoracoscópica es un tratamiento seguro, eficaz y permanente del blushing incapacitante. La ansiedad medida prequirúrgicamente es reactiva al blushing y no al revés.
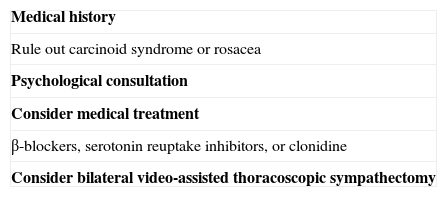
Blushing must be counted as a disorder or disease even though on certain occasions an individual may blush appropriately and even be expected to do so. However, when blushing occurs in response to minor psychological stimuli, gives rise to psychological distress, significantly affects activities at school or work, or interferes with affective or other interpersonal relationships, it must be considered a symptom of a psychiatric disorder and should be treated if a patient seeks help.1 Nonemotional stimuli, such as heat or physical exercise, can also lead to flushing and blushing, as can certain diseases such as hyperthyroidism, carcinoid tumor, or mastocytosis. Additionally, hot flushes are common in postmenopausal women and have been related to diminishing levels of estrogen. Certain skin diseases, such as rosacea, can be preceded by a long-standing tendency to blush and this sign may be present in systemic diseases such as dermatomyositis and lupus erythematosus. Adverse reactions to drugs (hydantoins, penicillin, pyrazolones, salicylates, sulfonamides, and tetracyclines) have also included blushing, which may arise more or less suddenly.2 In none of the aforementioned situations is blushing triggered by an emotional factor, however.
In the English language literature blushing refers to episodes of intense facial flushing that occur often and suddenly in response to emotional stimuli arising indirectly in everyday events (meetings at work or social gatherings, or shopping at a supermarket).1 Blushing may also be unrelated to an emotional trigger, however. Highly characteristic features of this sign are its suddenness and the accompanying feelings of distress, heat, and tingling in the face and, occasionally, confusion. Usually the cheeks and ears become red, but the flush may extend to the neck and upper portion of the chest. Avoidance behaviors may follow and the syndrome may be a symptom of social anxiety disorder, also known as social phobia. This disorder affects 13% of the general population at some point and is found to be frequent in up to half of patients who have a social anxiety disorder.3 Even patients with social anxiety who do not blush, however, display the associated signs and symptoms: distress, restlessness, looking away, inattention to others around them, or even smiling or grimacing.1
It can be useful to assess the severity of blushing by means of malar temperature to guide treatment decisions.4 The prevalence of blushing is unknown but social phobia is a common psychiatric disorder with a prevalence around 10%.5–7
Blushing was described as a debilitating condition by Darwin in 1872.8 The first to report a beneficial effect of thoracic sympathectomy on blushing was Wittmoser in 1985.9
Our minimally-invasive thoracic surgery department has performed over 2000 video-assisted thoracoscopic sympathectomies to treat various conditions.10 Other groups have had experience equivalent to ours.11–13 Our aim was to analyze the indications, safety, and efficacy of this procedure and to describe the clinical features of the patients we treated for blushing, including their personality and anxiety traits.
Materials and MethodsThis prospective observational study included thoracic surgery department patients who underwent bilateral endoscopic interruption of the sympathetic chain for debilitating blushing during the 7-year period from 2001 to 2008.
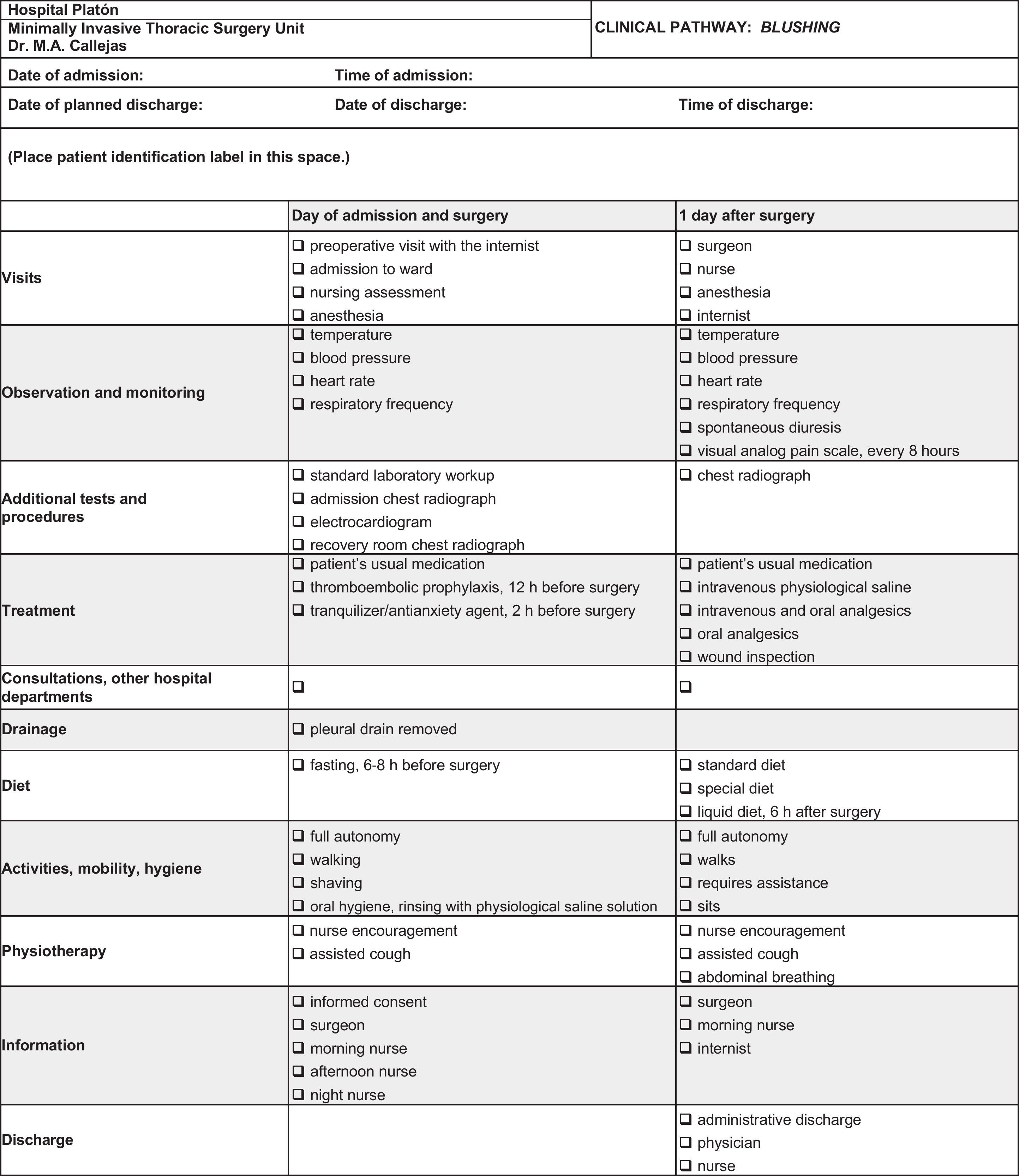
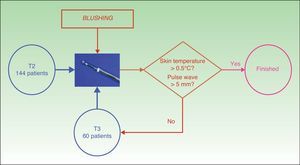
We established a clinical pathway for the patients (Fig. 1) and a protocol to guide treatment decisions (Table 1).
The patients were fully informed regarding the outcomes they could expect, side effects, and risks. All were interviewed by a team of clinical psychologists shortly before scheduling the surgery. Patients with stable facial flushing were examined by a dermatologist to exclude associated skin conditions.
All procedures were performed with the patient under general anesthesia, using oral-tracheal intubation and without carbon dioxide insufflation. Lung collapse was achieved by disconnecting the patient from the ventilator following hyperoxygenation. With the patient in supine decubitus position, arms abducted (aviator position), and the chest elevated to 45°, 25-mm access ports were placed at the third and fourth intercostal spaces in the axilla to provide access to the sympathetic chain.
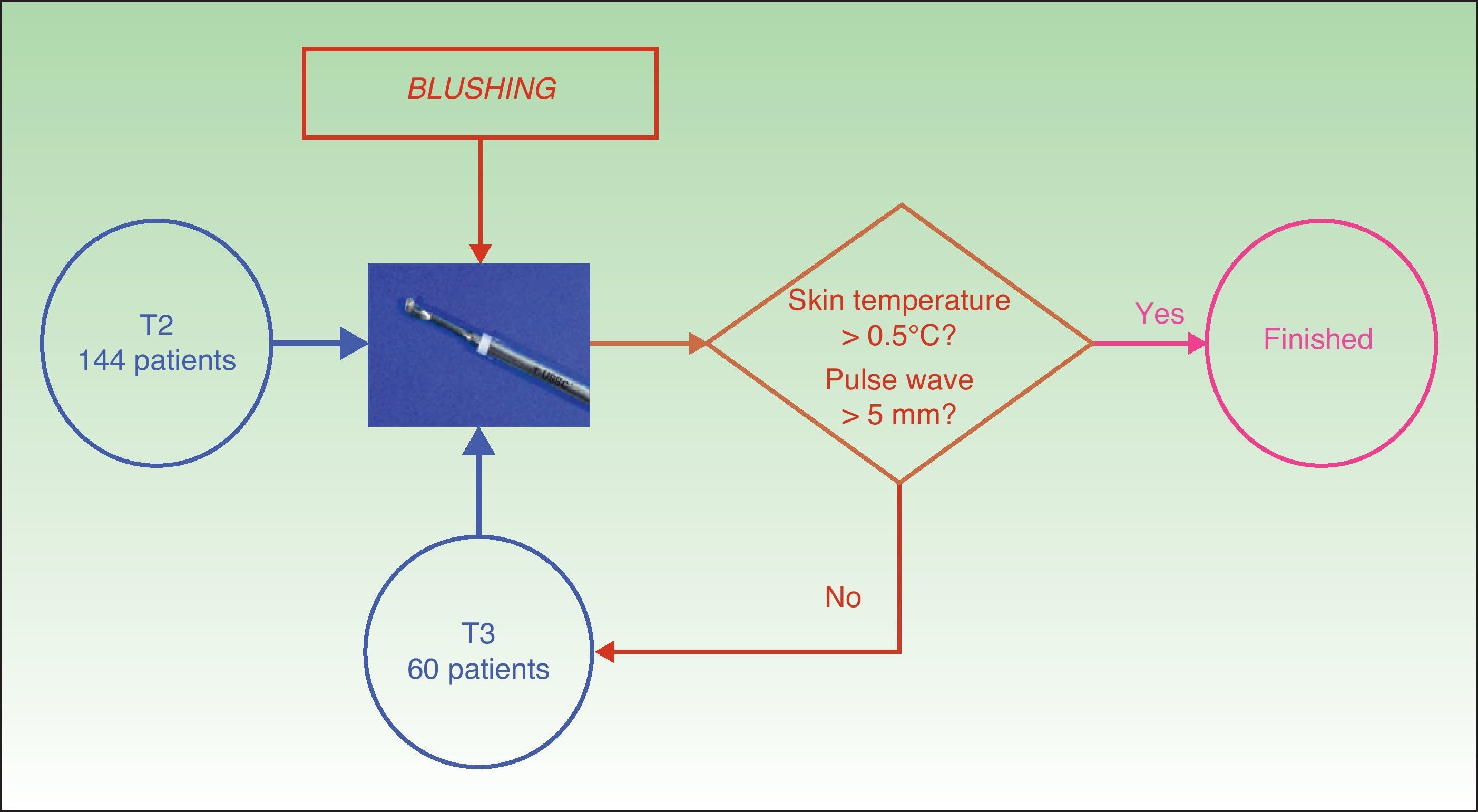
The surgical protocol was systematic bilateral interganglionic resection of the sympathetic chain (sympathicotomy) at T2 by ultrasound scalpel (AutoSonix System, United States Surgical, Division of Tyco Healthcare LP, USA) set to 55000Hz. On the basis of intraoperative response to the pulse wave and the cutaneous temperature corresponding to the sympathetic chain at T3, we also resected at that level or not. If the temperature at the thenar eminence of the upper arm after sympathectomy rose more than half a degree centigrade or if the pulse wave increased more than 5mm, we did not resect at T3 (Fig. 2). Kuntz nerves, if present, were also interrupted to T4.
Before discharge, a chest radiograph was used to rule out pneumothorax and hemothorax. We also checked for Horner syndrome. Postoperative telephone interviews were scheduled at 1 week, between 3 and 6 months, at 1 year, and at 2 years.
Two tests were administered. One was the revised NEO Personality Inventory in its short version, which measures 5 basic factors: neuroticism, extraversion, agreeableness, openness to experience, and conscientiousness. The second was the Liebowitz Social Anxiety Scale, modified for this study. This test measures fear and avoidance. The patients responded to both inventories during the visit with the anesthesiologist. The Leibowitz test was administered a second time 1 month after surgery when the patient returned for a follow-up visit with the thoracic surgeon. The NEO Personality Inventory results were compared to reference values for the general Spanish population. The t test for paired values was used to compare pre- and postoperative values on the Leibowitz Social Anxiety Scale.
ResultsA total of 204 patients with a mean age of 34 years (range, 15-67 years) were treated; the numbers of males and females were similar. A quarter of the patients had symptoms associated with social phobia, 10% had hyperhidrosis, and 5% telangiectasia. Forty-one percent of the patients in our series had a family history of blushing.
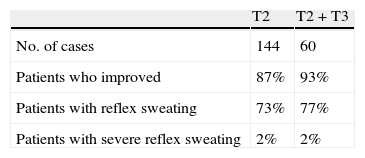
T2 and T2-plus-T3 sympathectomies were performed in similar numbers. On comparing the T2-resection group to the T2-T3 group, we detected no significant differences in efficacy of the procedure or severity of postoperative reflex sweating. (P>.05) (Table 2). Of the patients followed for 2 years (30%), only 1 was reoperated, successfully, for recurrence. No deaths were recorded and there was a single case of transient Horner syndrome, in a patient in whom we had not used the ultrasound scalpel. Video-assisted thoracotomy was required to treat pleural symphysis in 1 case, and of the 5 patients who developed pneumothorax, only 1 required pleural drainage. Patient satisfaction was high: only 10% had unexpected outcomes (low efficacy or excessive postoperative reflex sweating); 75% experienced reflex sweating, but this complication was severe in only 2% (Table 2).
None of the patients with pre- and postoperative social anxiety test results had personality profiles outside 1 SD of the population mean on any of the scales (T=50). The social anxiety scores were significantly lower after surgery, however, in comparison with the baseline scores. The mean score for the fear component of the social anxiety scale was 29.7 before surgery and 18.5 after surgery (t=4.1; sig, 0.000). The avoidance component of the scale fell from a mean preoperative score of 24.7 to a mean of 16.5 a month after the procedure (t=3.5; sig, 0.001).
DiscussionVideo-assisted thoracoscopic sympathectomy was a safe, effective treatment for blushing in this series, as shown by improvement in both physical and psychological symptoms.
The beneficial outcome of this surgical approach is to be expected. Blushing can be defined neurophysiologically as autonomic dysfunction, or a disorder of the autonomic nervous system that has craniofacial manifestations. Blushing is currently considered to occur as a result of postcapillary vasoconstriction due to activation of the cervical sympathetic nervous system pathways to the craniofacial region.14 As autonomic innervation is also implicated in controlling eccrine sweat glands, sweating often accompanies blushing. Repeated blushing eventually leads to rosacea and persistent erythema, telangiectasis, and inflammatory changes. Sympathectomy seems to act on the postcapillary sphincter, preventing the retention of blood in the face.
The acceptance of thoracoscopic sympathectomies as an effective treatment for blushing is based on work done at the Borås Hospital in Sweden.15,16 Two studies published in 1998 analyzed outcomes in 244 patients with blushing, finding that only 2% were dissatisfied with their results, 13% experienced some adverse effect, and 85% were fully satisfied with the procedure. Later studies also supported the use of this treatment,17–19 and it is currently a well established choice for treating uncontrolled, debilitating blushing.20–27 Our results are comparable to those of another recently published series.28
Attempting pharmacologic and cognitive behavioral therapies before resorting to surgery is appropriate. β-blockers, antianxiety drugs, serotonin reuptake inhibitors, and other antidepressants can be used for this disorder. Anecdotal evidence suggests that β-blockers may reduce blushing, but their use in this disorder has not been rigorously tested. Nonetheless, 1 trial of a pharmacologic treatment did find that blushing decreased in 75% of patients.29 Antianxiety drugs and antidepressants can help alleviate associated psychological symptoms, but their efficacy on the intensity of blushing remains undemonstrated. The effect of serotonin reuptake inhibitors on social phobia is well documented, but their effect on blushing is not.30
The use of cognitive behavioral therapy in patients with blushing has been reported,31 but the literature is scant and practical conclusions cannot be drawn. It must also be said that if surgery is ineffective, even in the absence of adverse events, the patient may feel helpless and depressed given the feeling that all options have been tried and there is no hope of a cure. The possibility of such feelings must be anticipated before surgery and the patient should be in touch with a psychiatrist who is able to prescribe antidepressive therapy, which will not only improve the patient's mental state but may also help to attenuate blushing.1
A 2002 study by Drott and coworkers17 is noteworthy in the literature on the surgical treatment of blushing. These authors analyzed the results of 831 thoracoscopic sympathectomies at T2 and found that outcomes were excellent for 94% of patients, who were followed for a mean of 29 months. Postoperative reflex sweating was observed in 67% of patients, although severity was not specified. We analyzed a series of 94 patients with blushing treated by video-assisted T2 sympathectomy in 2003.23 The outcomes were excellent in 90.4% and only 2% reported disappointment with the procedure. Postoperative reflex sweating occurred in 75.5% but was severe in only 3.2%. In 2006, Licht and coworkers19 reported results for 180 patients with blushing. They followed their patients for a mean of 20 months after sympathectomy at T2 in 101 patients and at T2-T3 in 79 patients, finding that 75% were satisfied with the outcome. Postoperative reflex sweating appeared in 88% (83% of the resections at T2 and 95% of the T2-T3 resections) and was severe in 22%.
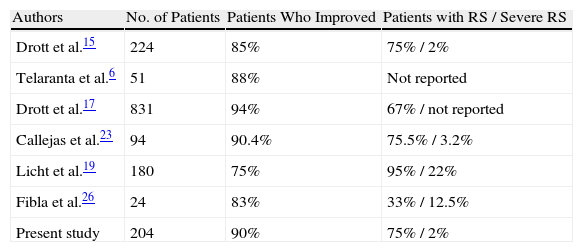
The rate of severe reflex sweating we observed in our series was much lower than the rate reported by Licht and coworkers19 and similar to the one observed by Drott and coworkers15 (Table 3).
Results of Sympathectomy for Blushing As Reported in the Literature: Efficacy and Postoperative Reflex Sweating.
| Authors | No. of Patients | Patients Who Improved | Patients with RS / Severe RS |
| Drott et al.15 | 224 | 85% | 75% / 2% |
| Telaranta et al.6 | 51 | 88% | Not reported |
| Drott et al.17 | 831 | 94% | 67% / not reported |
| Callejas et al.23 | 94 | 90.4% | 75.5% / 3.2% |
| Licht et al.19 | 180 | 75% | 95% / 22% |
| Fibla et al.26 | 24 | 83% | 33% / 12.5% |
| Present study | 204 | 90% | 75% / 2% |
Abbreviation: RS, postoperative reflex sweating.
The satisfactory results we report may be explained by the fact that the same surgeon performed all the procedures and the surgical protocol (Fig. 2) was followed rigorously. We sectioned the sympathetic chain between ganglia in all cases, sparing the ganglion to minimize postoperative reflex sweating. We also believe that our use of the ultrasound scalpel was an important feature of the protocol. This tool sections the sympathetic chain more safely, providing an optimal view of the field, because no smoke rises, and it does not cause peripheral damage to the lung parenchyma or other nearby tissues (intercostal blood vessels and nerves).24 Horner syndrome caused by temperature elevation is avoided and the incidence of other forms of nerve damage is lower. Finally, we note that clips have been used to interrupt the sympathetic chain32 in the interest of making reversal possible in case reflex sweating is debilitating. However, reversibility is not in fact ensured and recurrence is more common. The risk of Horner syndrome is also greater because the chain becomes longer on application of the clip.
The complications and adverse effects of sympathectomy in patients with isolated blushing are generally similar to those observed when this procedure is performed for primary hyperhidrosis.
ConclusionsOur study shows that video-assisted thoracoscopic surgery to treat blushing is safe, effective, and permanent. Adverse effects are few. We emphasize the importance of the beneficial effect of surgery on these patients’ anxiety and social phobia. We can also conclude that the anxiety that is detected before surgery is a reaction to blushing rather than a cause of it as some have suggested.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Callejas MA, Grimalt R, Mejía S, Peri JM. Resultados del tratamiento videotoracoscópico del blushing. Actas Dermosifiliogr.2012;103:525-31.