Dermatologists working primarily with children are familiar with the problems faced by patients who have rare genetic skin diseases. Diagnosis may be more or less straightforward, but patients and their families will always face serious difficulties in everyday life, due in part to the disease itself but also to the lack of knowledge and understanding of their condition within the health care system. Epidermolysis bullosa (EB) and ichthyosis are examples of such rare genodermatoses. EB, and particularly its generalized dystrophic forms, is undoubtedly one of the most severe genetic skin diseases dermatologists encounter in their practice. Over the course of their lives, patients with severe forms of dystrophic EB (DEB) experience a series of severe extracutaneous manifestations that have an extraordinarily negative impact on their quality of life, leading to early death in many cases.1,2 While most ichthyoses, fortunately, are not life-threatening, these diseases do adversely affect quality of life and require multidisciplinary care.3 It is fortunate that both EB and the most severe forms of ichthyoses are rare; that is, their prevalence is less than 1 case per 2000 individuals. Two recent studies that estimated the prevalence in Spain of DEB and autosomal recessive congenital ichthyosis (ARCI), respectively, reported an approximate prevalence of 6.0 cases per million inhabitants4 for DEB and 7.2 cases per million inhabitants for ARCI.5 The same studies also showed that the majority of patients in Spain who have these diseases lack a genetic diagnosis and are not treated in a specialized setting; that is, they do not have access to a hospital staffed by experts and equipped with the material and human resources their treatment requires. The evidence plainly shows that the care of these patients could be improved. As there are no officially recognized centers of reference in Spain for these rare diseases, it is impossible to refer affected patients to the hospital that can offer them the best medical attention for their condition.
According to recent estimates, there are 276 patients in Spain with DEB.4 Considering the population of each Spanish autonomous community, we would expect the number of cases per community to range from a high of 46 in Andalusia to a low of 2 in La Rioja; the autonomous cities of Ceuta and Melilla are excluded from this calculation because their very small population would give an estimated prevalence of close to 0 (Table 1). The prevalence of ARCI in Spain is estimated at 288 cases, and the resulting distribution would range from about 60 in Andalusia to 1 in the autonomous cities of Ceuta and Melilla (Table 2). Clearly, this theoretical distribution of affected patients based on the population density of each autonomous community is of fundamental importance in any decision concerning the allocation of health care resources in general and the location of future centers of reference in particular.
Expected Number of Cases of Dystrophic Epidermolysis Bullosa (DEB) by Spanish Autonomous Community.
| Autonomous Community | Population (× 106 inhabitants) | Expected No. of Cases of DEB (95% CI) |
| Andalusia | 8.3 | 50 (35-98) |
| Aragon | 1.3 | 8 (6-16) |
| Asturias | 1.1 | 6 (4-12) |
| Balearic Islands | 1.1 | 7 (5-13) |
| Canary Islands | 2.1 | 13 (9-25) |
| Cantabria | 0.6 | 3 (2-7) |
| Castile- Leon | 2.5 | 15 (10-29) |
| Castile-La Mancha | 2.0 | 12 (9-24) |
| Catalonia | 7.3 | 44 (31-86) |
| Valencia | 5.0 | 30 (21-59) |
| Extremadura | 1.1 | 6 (5-13) |
| Galicia | 2.7 | 16 (11-32) |
| Madrid | 6.4 | 38 (27-75) |
| Murcia | 1.5 | 9 (6-17) |
| Navarre | 0.6 | 4 (3-7) |
| Basque Country | 2.1 | 13 (9-25) |
| La Rioja | 0.3 | 2 (1-4) |
| Ceuta | 0.08 | 0 (0-1) |
| Melilla | 0.08 | 0 (0-1) |
Expected Number of Cases of Autosomal Recessive Congenital Ichthyosis (ARCI) by Spanish Autonomous Community.
| Autonomous Community | Population (× 106 Inhabitants) | Expected No. of Cases of ARCI (95% CI) |
| Andalusia | 8.3 | 60 (47-80) |
| Aragon | 1.3 | 9 (7-13) |
| Asturias | 1.1 | 8 (6-10) |
| Balearic Islands | 1.1 | 8 (6-11) |
| Canary Islands | 2.1 | 15 (12-20) |
| Cantabria | 0.6 | 4 (3-6) |
| Castile-Leon | 2.5 | 18 (14-24) |
| Castile-La Mancha | 2.0 | 15(12-20) |
| Catalonia | 7.3 | 53 (42-71) |
| Valencia | 5.0 | 36 (29-49) |
| Extremadura | 1.1 | 8 (6-11) |
| Galicia | 2.7 | 20 (16-27) |
| Madrid | 6.4 | 46 (36-62) |
| Murcia | 1.5 | 11 (8-15) |
| Navarre | 0.6 | 4 (4-6) |
| Basque Country | 2.1 | 15 (12-21) |
| La Rioja | 0.3 | 2 (2-3) |
| Ceuta | 0.08 | 1 (0-1) |
| Melilla | 0.08 | 1 (0-1) |
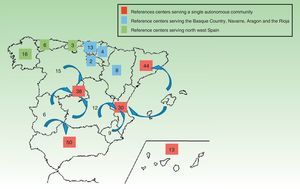
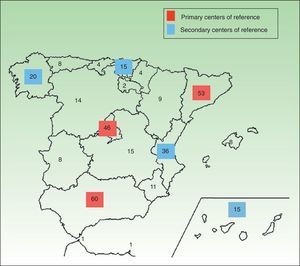
In diseases as rare as DEB or ARCI it is essential to establish centers of reference where experts can confirm the patients’ diagnosis, assess their prognosis, provide genetic counseling and, in general, manage the complications associated with the condition in the context of a multidisciplinary team. Conversely, such centers of reference need to treat enough patients to allow experience with the disease to accumulate. It would, therefore, be of little use to create a large number of such centers if in practice each one only provided care for very few affected patients. Moreover, these units must be accessible and located at a reasonable distance from the homes of affected patients. The aim is to ensure that visits to the health care center do not become a financial burden or excessively disrupt the personal or working life of patients or their families. We estimate that it would be reasonable to have national reference centers for DEB and ARCI in the autonomous communities with larger populations, such as Andalusia, Madrid and Catalonia, and that these centers could also serve patients who live in smaller autonomous communities nearby, where there are too few patients to warrant a local center. In some areas, such as the northeast of Spain where the autonomous communities of Galicia, Cantabria, and Asturias have a combined estimated prevalence similar to that of the more populous communities, a shared center of reference could be established to serve the whole region. In Figs. 1 and 2, we propose several examples of possible networks of reference centers for DEB and ARCI in Spain. Despite the decentralized structure of the Spanish health care system, in the case of these rare disease the authorities should set aside political interests and understand the need to work together for the benefit of the patient.
Possible distribution of dystrophic epidermolysis bullosa (DEB) reference centers in Spain. A reference center for each one of the larger autonomous communities (those in red) may be possible. The smaller autonomous communities (in blue and green) could be grouped together and a reference center created to serve each group. In some cases, patients may choose to attend a reference center in an adjacent autonomous community because it is easy for them to access or has historically served their area.
Possible distribution of autosomal recessive congenital ichthyosis (ARCI) reference centers based on the estimated prevalence by autonomous community. The primary or most important reference centers, working on a national level, would be located in the more populous autonomous communities (red squares), and the secondary reference centers (blue squares), serving a considerable number of patients, would be located in the less populous autonomous communities. The patients in the other Spanish autonomous communities could choose the most appropriate primary or secondary centers depending on geographical distance or personal considerations.
Besides taking into consideration the issue of estimated prevalence (the expected caseload in each autonomous community), we also need to ensure that centers of reference have the material and human resources they need to resolve complications as they arise. For example, although almost any organ may be affected by DEB and consequently specialists in almost all fields are needed, the absolutely essential core team must include a dentist, gastroenterologist, ophthalmologist, nutritionist, and hand surgeon. In the case of ARCI, the dermatologist in charge must be an expert in ichthyoses and related skin problems and also be prepared to efficiently coordinate the medical care of other commonly affected organs, such as the eyes and ears. Specialists involved in the treatment of DEB and ARCI must acquire the best training available in the disease they are treating because these conditions are unlike other disorders. Over time, clinicians’ knowledge of a disease clearly improves with experience, but given the scant number of patients with these rare diseases, an alternative pathway to expertise would be to spend a period working in centers acknowledged to have experience or to attend relevant seminars. The opportunity to simply consult physicians who are expert in the disease to discuss treatment options available would be another pathway to training. DEBRA Spain organizes and finances training (in Spain and abroad) for interested professionals, and the Spanish Ichthyosis Association (ASIC) has also made training one of the objectives of its recently established research fund. Patients affected by these diseases expect a high level of knowledge from their physicians because they are very often better informed about their condition than their specialist.
Another crucial aspect of reference centers is communication between professionals on a multidisciplinary care team as this approach is particularly important for patients who require coordinated, consistent care that follows a shared protocol. Working with centers that have diagnostic laboratories is also particularly important. In Spain, we have at least 2 such centers for EB: one in Madrid (CIEMAT) and one in Barcelona (Hospital Clínic). There are also at least 2 facilities offering molecular diagnostic services for the different types of ARCI: the Molecular Biology Department at the University of Salamanca (which also provides genetic diagnosis of other types of ichthyosis), and the genomic medical foundation (Fundación de Medicina Xenómica) at the University of Santiago de Compostela. These services are essential for managing EB because it is impossible to determine the type of EB affecting a newborn baby on the basis of clinical appearance alone; good communication between the dermatologist and the laboratory would make it possible to define the type within a week of birth, thereby providing parents an early diagnosis and an accurate assessment of the prognosis. The point is not to label the disease, but rather to inform the family promptly about what to expect and the potential complications their child may develop.
The centers of reference should also be responsible for managing the patient's transition from pediatric to adult care. This transition may be easier in general hospitals because it seems that communication between caregivers in the two phases of life should be more fluid, but a smooth transition is not impossible for patients treated in pediatric hospitals, and indeed in some diseases, such as cystic fibrosis, the continuity of care is extremely well organized. An effort should also be made to ensure easy patient access to the center of reference and fluid communication between the specialized center and other hospitals. It would even be desirable for experts in DEB or ARCI to give basic training to professionals who only sporadically encounter patients with these diseases in their practice. In this way, more specialists would become familiar with the relevant protocols and would apply them.
We should never lose sight of the ultimate goal of centers of reference: to provide affected patients with the best care from birth. The model proposed is neither an attempt to label a certain type of disease or a way to invoke professional prestige; the intention is, rather, to inform parents about their child's prognosis, to anticipate and treat complications, and eventually to facilitate access to genetic counseling and support patients and their families throughout their lives. In short, to achieve these objectives, centers of reference for EB and ichthyosis are urgently needed in Spain.
We would like to thank Dr. Ignacio García Doval for his assistance in estimating the prevalence of DEB and ARCI by autonomous community.
Please cite this article as: Hernández-Martin A, et al. Unidades de referencia para epidermólisis ampollosas e ictiosis: una necesidad urgente en Espa¿na. Actas Dermosifiliogr. 2013;104:363-6.