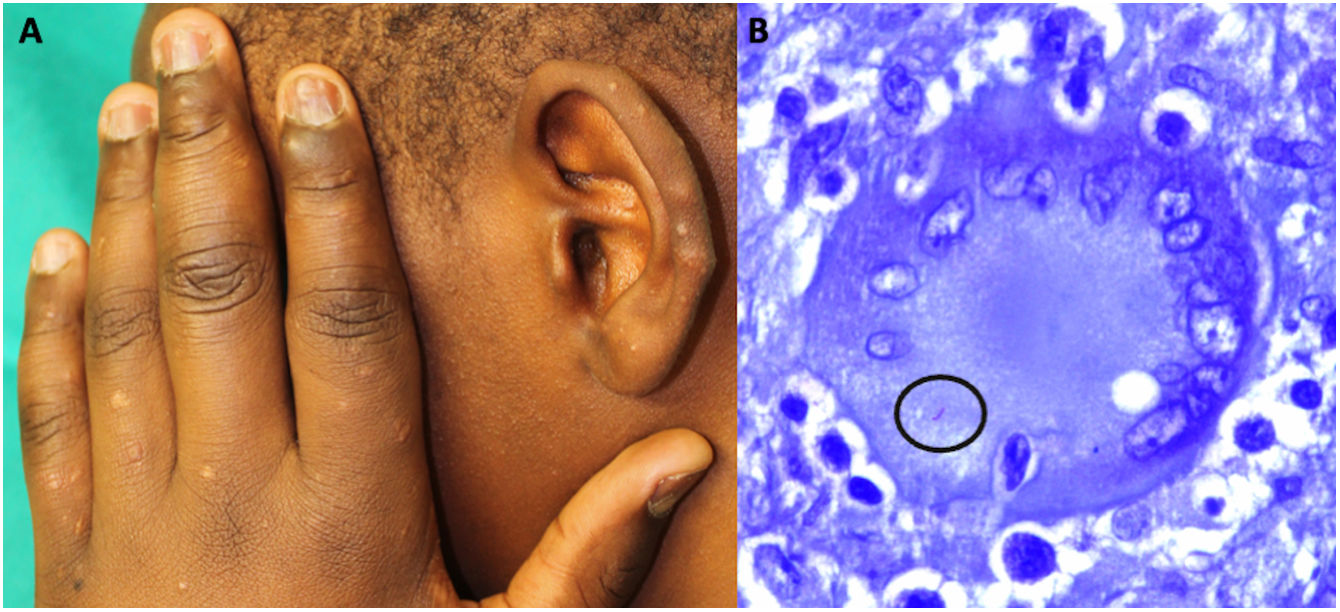
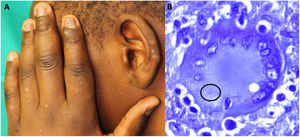
This is the case of a 15-year-old teenager from Senegal. The patient presented with asymptomatic lesions on his ears and back of his hands that had been spontaneously appearing and recurring over the past year. Upon physical examination, small yellowish skin-colored millimeter-sized papules were seen symmetrically distributed across these regions (Fig. 1A). The patient showed no further symptoms. A biopsy of one of the ear lesions revealed the presence of necrotizing granulomas. After several serial Ziehl–Neelsen stains, a bacillus was finally seen (Fig. 1B). According to the thoracic and abdominal CT scan performed no other organs were involved. Sputum bacilloscopy tested negative, unlike the Quantiferon test, which tested positive. Based on these findings, the patient was diagnosed with papulonecrotic tuberculid (PNT). After a 1-month oral course with isoniazid, rifampicin, pyrazinamide, and ethambutol, the skin lesions were almost completely gone.
Cutaneous PNT is a rare form of extrapulmonary PNT that has been reported in 1–2% of the cases. The clinical presentation can vary. It often affects teenagers between the ages of 10 and 14 but can occur at any age. It is mainly due to the presence of Mycobacterium tuberculosis and less commonly to Mycobacterium bovis. It often has a long course. PNT often presents with recurrent symmetrical outbreaks of papules, pustules, crusts, and even ulcers symmetrically distributed on the face, ears, extensor surfaces of the limbs, trunk, and buttocks. PNT can be preceded by systemic symptoms and often resolves spontaneously within a matter of weeks or months, potentially leaving varioliform scars. The differential diagnosis for PNT includes lichen scrofulosorum, a form of tuberculid. Papulonecrotic forms were originally considered tuberculids. However, DNA from mycobacteria has been detected in them through the polymerase chain reaction (PCR) test. Therefore, it is now suggested that these forms represent true tuberculosis rather than hypersensitivity reactions. In our case, the finding of a bacillus in the skin biopsy and the absence of pulmonary involvement support the latter option.