A broad range of skin flaps can be used to repair facial surgical defects after the excision of a tumor. The aim of our study was to develop a practical guideline covering the most useful skin grafts for each of the distinct facial cosmetic units.
Material and methodsThis was a multicenter study in which 10 dermatologists with extensive experience in reconstructive surgery chose their preferred technique for each cosmetic unit. The choice of flaps was based on personal experience, taking into account factors such as suitability of the reconstruction technique for the specific defect, the final cosmetic result, surgical difficulty, and risk of complications. Each dermatologist proposed 2 flaps in order of preference for each cosmetic subunit. A score of 10 was given to the first flap and a score of 5 to the second.
ResultsThe total score obtained for each of the options proposed by the participating dermatologists was used to draw up a list of the 3 best grafts for each site. There was notable unanimity of criteria among most of the dermatologists for reconstructive techniques such as the glabellar flap for defects of the medial canthus of the eye, the bilateral advancement flag flap or H flap for the forehead, the rotary door flap for the auricle of the ear, the Mustarde flap for the infraorbital cheek, the O-Z rotation flap for the scalp, the Tenzel flap for the lower eyelid, and the island flap for the upper lip.
ConclusionsThe results of this study will be useful as a practical guide to choosing the best reconstruction technique for each of the facial cosmetic units.
Existe una enorme variedad de colgajos cutáneos empleados para la reparación de defectos quirúrgicos faciales tras la extirpación de tumores. El objetivo del estudio fue consensuar una guía práctica de los colgajos más útiles para cada una de las distintas unidades estéticas faciales.
Material y métodosEstudio multicéntrico donde 10 dermatólogos de larga experiencia quirúrgica reconstructiva eligieron sus técnicas preferidas para cada unidad estética. La elección de estos colgajos se fundamentó en la experiencia personal de cada dermatólogo basándose en factores como la idoneidad de la técnica reconstructiva para ese defecto, el resultado estético final, la facilidad de ejecución y la baja probabilidad de complicaciones, entre otros. Eligieron 2 colgajos por orden de preferencia para cada subunidad estética y se le asignaron 10 puntos al primer colgajo y 5 al segundo.
ResultadosCon la suma obtenida de todas las opciones aportadas por los dermatólogos encuestados se obtuvo una relación de los 3 mejores colgajos para cada localización. Destacar la unanimidad de criterio por parte de la mayoría de los dermatólogos para técnicas reconstructivas como el colgajo glabelar para defectos de canto interno del ojo, el colgajo de avance bilateral en bandera o H para frente, el colgajo en puerta giratoria para concha auricular, el colgajo pangeniano para mejilla infraorbitaria, el colgajo de rotación O-Z para cuero cabelludo, el colgajo de Tenzel para párpado inferior y el colgajo en isla para labio superior.
ConclusionesLos resultados de este estudio son de utilidad para ofrecer una guía práctica para la elección de las mejores técnicas reconstructivas en cada una de las distintas subunidades estéticas faciales.
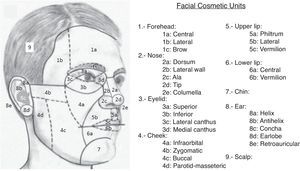
The reconstruction of large surgical defects after the surgical excision of skin tumors usually requires the use of skin flaps. For optimal results, it is important to take into account the concept of facial cosmetic units.1 These units consist of areas limited by natural folds and borders, such as the nasolabial fold, mental crease, vermilion, brow, and hairline, and have a relatively uniform skin color, texture, and thickness, quantity of subcutaneous fat, mobility, and hair distribution, among other common characteristics. The main cosmetic units are in turn subdivided into various subunits because of the anatomic complexity of some regions, such as the nose and the auricles of the ear (Fig. 1). Certain fundamental norms based on these cosmetic units exist to help us achieve minimally visible scars. A flap must be designed within the limits of the cosmetic unit in which the primary defect is located, and the incisions should preferably be placed along the borders of the units, without crossing them. It should also be noted that best results are obtained with the reconstruction of complete cosmetic units, even if the defect affects less than the whole unit, and that the reconstruction of defects that affect various cosmetic units should be undertaken considering each individual unit, compartmentalizing the repair. However, there is considerable variability in the choice of the best flap for each site. Although general recommendations exist according to the topographic site,2–5 no consensus guidelines have been published to specify which flap should be used in each cosmetic unit. In order to draw up a practical guideline on the most useful flaps for each one the distinct facial cosmetic units, we undertook a study with the participation of 10 dermatologists with extensive experience in reconstructive surgery, who stated their preferred flaps for each site. We have found no evidence that any study of these characteristics has yet been performed in Spain.
Materials and MethodsTen dermatologists were selected from different surgical schools across the Iberian Peninsula (9 Spanish and 1 Portuguese). All had between 10 and 30 years’ experience in dermatologic surgery and performed at least 300 complex operations per year. They were sent a questionnaire with a diagram of all the facial cosmetic subunits and they were asked to choose 2 flaps, in order of preference, for each subunit.
The choice of flaps was based on each dermatologist's personal experience. The suitability of a flap depended on factors such as the objective adaptation of flap design to the site of the defect, final cosmetic result, surgical complexity, and risk of complications.
To unify flap classification criteria, we decided to use the concept of the main movement performed during movement of the flap—rotation, transposition, or advancement—and the participating dermatologists were sent a detailed classification so that the same terminology was used in all cases. Among the rotation flaps we included classic variants such as the Mustardé, O-Z, and Rieger flaps. Transposition flaps were subdivided into rhomboidal (Limberg, Dufourmentel), bilobar, and interpolation (nasolabial, paramedian forehead) flaps.
Advancement flaps were subdivided into unilateral, bilateral (flag), A-T, V-Y, crescentic, and island.
The first flap chosen was assigned 10 points and the second 5. The 3 best flaps for each site were thus determined according to the sum of the scores obtained from each participating dermatologist.
ResultsAll the reconstruction techniques chosen by each dermatologist for each facial cosmetic subunit are listed in order of preference in the Additional Material, together with the final score obtained for each reconstruction technique in each cosmetic subunit.
DiscussionDermatologic surgical practice varies considerably in Spain depending on the surgical school in which a surgeon has trained. This data compilation has enabled us to draw certain conclusions that represent an interesting common viewpoint on the choice of reconstructive technique.
First, the flap with the highest score was the glabellar flap for defects of the medial canthus of the eye. This flap achieved the maximum score of 100 points, reflecting unanimity of all the participating dermatologists for this cosmetic unit. The flaps with the following highest scores were the bilateral advancement flag flap or H flap for the forehead (95 points), the revolving-door flap for the auricle of the ear (85 points), the Mustardé flap for the infraorbital cheek (85 points), the O-Z rotation flap for the scalp (80 points), the Tenzel flap for the lower eyelid (75 points), and the island flap for the upper lip (75 points). The agreement on the use of these flaps as best option in these cosmetic units, supported by the extensive surgical experience of the participating dermatologists, allows us to confirm them as the flaps of first choice for each of these sites.
In the analysis of the cosmetic units that generated fewest different repair options, the parotid-masseteric subunit of the cheek stood out for having only 2 flaps nominated: the rhomboid transposition (Limberg) flap and the lateral rotation flap. This finding also confirmed unanimity of criteria in this cosmetic subunit.
In contrast, the sites for which the largest number of different flaps were proposed were the antihelix of the auricle of the ear and 3 subunits of the external nose: the lateral wall, the tip, and the dorsum of the nose. This diversity of flaps suggests a lack of unanimity of criteria between participants; this can be explained by the surgical complexity of these areas. Another possible cause is the use of different flaps depending on the size of the defect within a single cosmetic subunit.
With respect to the most frequently chosen flaps according to the main movement to be made, advancement flaps came at the top of the list, followed by transposition flaps and, finally, rotation flaps. However, the individual flap most widely used in the overall group of facial cosmetic units was the Limberg flap. This flap can therefore be considered the most versatile flap for use in almost all the cosmetic subunits. But perhaps the most important outcome of the analysis of these data is the elaboration of a practical guideline to choose the ideal flap in each cosmetic subunit (Table 1).
- –
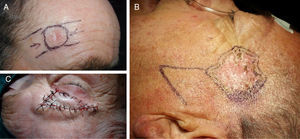
In the central subunit of the forehead, the flap of choice was the bilateral advancement flag flap or H flap (Fig. 2A),6 followed by the A-T advancement flap and the O-Z rotation flap.
- –
In the lateral subunit of the forehead, the flap of choice was the Limberg flap (Fig. 2B), followed by the rotation flap from an inferior position and, in third place, the A-T flap.
- –
In the brow, the preferred flap was the island flap (Fig. 2C), followed by the flag flap and, finally, the O-Z rotation flap.
- –
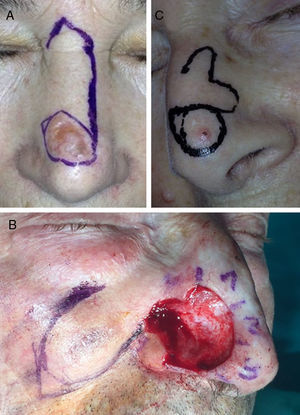
For the dorsum of the nose, the flap of choice was the Rieger flap (Fig. 3A),7 followed by the Limberg flap and the A-T flap.
- –
On the lateral wall of the nose, the first choice of flap was the Limberg flap,8 followed by the lateral advancement flap and, in third place, the lateral advancement flap with a double Burow or Webster triangle.
- –
The majority of participants in the survey most commonly used a nasolabial transposition flap to reconstruct the nasal ala (Fig. 3B),9 with the Limberg flap in second place and spiral rotation flap in third.
- –
There was considerable variability in the choice of flap for the repair of defects on the tip of the nose, but the bilobar flap (Fig. 3C) was preferred, followed by the horizontal advancement flap after the excision of 2 opposing Burow triangles (east-west advancement flap10), and in third place the Rieger flap.
- –
The columella was also a cosmetic subunit in which it was difficult to reach consensus because few cases affect this site.11 In the end, the first choice was the upper lip double transposition flap, second was Burow triangles, and third the nasolabial flap.
- –
With respect to the upper eyelid,12 few defects cannot be closed by direct suture. When a flap is required, the lateral advancement flap gained the highest score, followed by the reverse Tripier flap and the reverse Tenzel flap.
- –
The lower eyelid, on the other hand, is an area that requires flaps even for small defects due to the risk of ectropion.13 The first choice of flap for this subunit was the lateral advancement or Tenzel flap (Fig. 4A), followed by the classic Tripier or myocutaneous transposition flap from the upper eyelid and, in third place, the Imre flap, which is a rotation flap using skin from the infraorbital cheek adjacent to the defect.
- –
For defects of the lateral canthus of the eye, the Limberg flap (Fig. 4B) received the highest score, followed by the lateral advancement flap with 2 Burow triangles (the puzzle flap),14 and the M-plasty.
- –
The glabellar flap (Fig. 4C) received by far the highest score for defects of the medial canthus of the eye,15 followed by the island flap, and, in third place, the A-T flap.
- –
In the majority of cases, the infraorbital cheek was reconstructed using the Mustardé flap (Fig. 5A), followed by the rotation flap from lower areas of the cheek (the Blascovicz flap), and the Limberg flap in third place.16
- –
The Limberg flap was preferred for the zygomatic region of the cheek (Fig. 5B), followed by the lateral rotation flap, and the M-plasty in third place.
- –
The Limberg flap was also the most voted for the buccal cheek, followed by the crescentic flap and the lateral advancement flap.
- –
Curiously, only 2 flaps were nominated for the parotid-masseteric region of the cheek, the Limberg flap in first place, and the lateral rotation flap in second.
- –
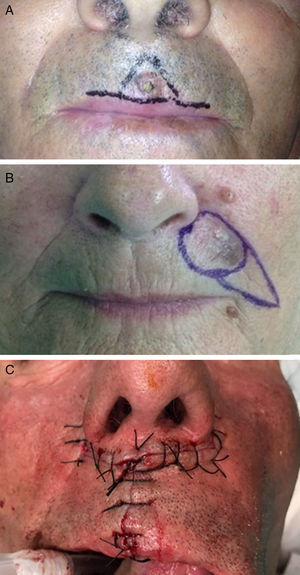
The central area (philtrum) of the upper lip was reconstructed by the majority of participants using the A-T flap (Fig. 6A).17 In second place was the flag flap and, in third, the island flap.
Figure 6.A, A-T flap for the philtrum of the lip. B, Subcutaneous island pedicle flap for the upper lip. C, The bilateral perialar horizontal advancement flap for the vermilion of the upper lip.
Photograph A courtesy of Dr. Soledad Saénz Guirado. Photograph B courtesy of Dr. Antonio Clemente Ruiz de Almirón. Photograph C courtesy of Dr. Francisco Vilchez.
- –
In the lateral zones of the upper lip, the island flap (Fig. 6B) was the flap of choice, followed by the A-T flap and the Bernard-Webster flap.18
- –
When a simple wedge is insufficient to repair a full-thickness defect of the vermilion of upper lip and a flap must be used, the bilateral perialar horizontal advancement flap described by Celsus (Fig. 6C) was the most widely used, followed by the pedicled rotation flap in 2 stages from the lower lip (the lip switch or Abbe flap), and in third place the inverted Karapandzic flap, which is a rotation-advancement flap of skin from the upper lip, following the nasolabial sulcus.19
- –
The most widely used flap in the vermilion of lower lip was the advancement flap with double crescents from the chin, proposed by Turgut20 (Fig. 7), followed by the rotation-advancement flap from the skin of the lower lip and nasolabial sulcus (the classic Karapandzic) and the Abbe pedicled rotation flap from the upper lip.
- –
In the central region of the lower lip, the flap of choice was the A-T flap, followed by the flag flap and the M-plasty.
- –
The majority of participants reconstructed the chin using an A-T flap (Fig. 8),21 with a rotation flap along the labiomental fold in second place, and the lateral advancement flap in third.
- –
The flap that received most votes for the helix of the ears was the helical advancement flap (Fig. 9A),22 followed by the retroauricular advancement flap and the Trendelenburg reduction plasty.
- –
The Limberg flap was the flap of choice for the antihelix, followed by the single or double (O-Z) rotation flap and the A-T flap in third place.
- –
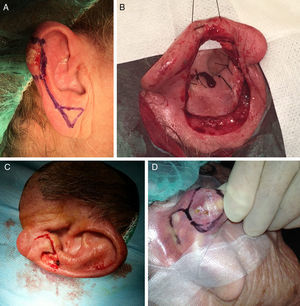
The majority of participating surgeons used a revolving-door flap to repair the concha of the ear (Fig. 9B). Healing by second intention was considered a very useful alternative to flaps in this region. In third place, the preauricular transposition flap in 2 stages.
- –
The Limberg flap was the flap of choice for the earlobe (Fig. 9C), followed by the modified bilobar flap using retro- and infra-auricular skin (the Gavello flap),23 and an advancement flap in third place.
- –
The retroauricular area was repaired by the majority of participating dermatologists using a Limberg flap (Fig. 9D), followed by rotation flaps, and an advancement flap in third place.
- –
And finally the scalp cosmetic unit, which was reconstructed by the majority of participants using an O-Z rotation flap (Fig. 10), followed by the triple Limberg flap and healing by second intention.24
List of the 3 Reconstruction Techniques of Choice for Each Cosmetic Subunit.
| First Choice of Flap | Second Choice of Flap | Third Choice of Flap | |
|---|---|---|---|
| Central forehead | Flag | A-T | O-Z |
| Lateral forehead | Limberg | Inferior rotation | A-T |
| Brow | Island | Flag | O-Z |
| Dorsum of the nose | Rieger | Limberg | A-T |
| Lateral wall of the nose | Limberg | Lateral advancement | Bernard-Webster |
| Nasal ala | Nasolabial | Limberg | Spiral |
| Tip of the nose | Bilobar | East-west | Rieger |
| Columella | Double transposition | East-west | Nasolabial |
| Upper eyelid | Lateral advancement | Reverse Tripier | Reverse Tenzel |
| Lower eyelid | Tenzel | Tripier | Imre |
| Lateral canthus | Limberg | Puzzle | M-plasty |
| Medial canthus | Glabellar | Island | A-T |
| Infraorbital cheek | Mustardé | Blascovicz | Limberg |
| Zygomatic cheek | Limberg | Mustardé | M-plasty |
| Buccal cheek | Limberg | Crescentic | Burow triangle |
| Parotid cheek | Limberg | Lateral rotation | |
| Upper lip philtrum | A-T | Flag | Island |
| Lateral upper lip | Island | A-T | Bernard-Webster |
| Vermilion of upper lip | Bilateral perialar horizontal advancement | Abbe | Reverse Karapandzic |
| Central lower lip | A-T | Flag | M-plasty |
| Lower lip vermilion | Double crescentic | Karapandzic | Abbe |
| Chin | A-T | Rotation | Lateral advancement |
| Helix of the ear | Helical advancement | Retroauricular advancement | Reduction plasty |
| Antihelix of the ear | Limberg | Rotation | A-T |
| Concha of the ear | Revolving-door | Second intention | Transposition |
| Earlobe | Limberg | Modified bilobar (Gavello) | Advancement |
| Retroauricular | Limberg | Rotation | Advancement |
| Scalp | O-Z | Triple Limberg | Second intention |
The list of the best 3 skin flaps for each one of the 28 facial cosmetic subunits is a practical guideline that can help dermatologists to choose the best reconstruction technique in specific cases.
The availability of digital devices with wi-fi connection in the majority of operating rooms will make it possible to perform online searches for surgical solutions when repairing surgical defects, with the advantage of an immediate search result. For this reason, and to facilitate access, a schematic version of these guidelines has been included on the online atlas of dermatologic surgery (www.cirugiaderma.es) in the section on flaps of choice (http://www.cirugiaderma.es/colgajos%20de%20eleccion.htm).
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Russo F, Linares M, Iglesias ME, Martínez-Amo JL, Cabo F, Tercedor J, et al. Técnicas reconstructivas de elección por unidades estéticas faciales. Actas Dermosifiliogr. 2017;108:729–737.