A 55-year-old man, with no relevant medical history, presented with skin lesions on both legs that had appeared 5 months earlier and had become more evident and itchier in the preceding days. He had no associated general symptoms.
Physical ExaminationPhysical examination revealed multiple brownish-red nummular purpuric plaques with superficial scaling on the lower limbs (Fig. 1). The lesions did not disappear under pressure. Dermoscopy revealed punctate hemorrhagic stippling and hemosiderin deposits.
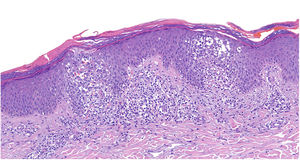
HistopathologyDermal histopathology showed a psoriasiform spongiotic dermatitis with irregular parakeratosis, superficial perivascular infiltrate, and red blood cell extravasation (Fig. 2). Direct immunofluorescence and T-cell receptor clonality analysis of a skin biopsy specimen were both negative.
Additional TestsInitial laboratory analyses, including a complete blood count, biochemistry and coagulation parameters, and urinalysis, revealed no abnormalities. An autoimmunity study was negative for antinuclear antibodies, antineutrophil cytoplasmic antibodies, and cryoglobulins. Patch test results were negative.
What is your Diagnosis?
DiagnosisBased on the clinical and histological findings, the patient was diagnosed with Doucas and Kapetanakis eczematoid purpura.
Clinical Course and TreatmentThe lesions resolved after 6 months of treatment with topical corticosteroids, oral colchicine, and oral nicotinamide, leaving residual hyperpigmentation (Fig. 3).
CommentPigmented purpuric dermatoses (PPD) is a heterogeneous group of benign and chronic dermatoses. They are characterized clinically by the appearance of reddish purple macules and petechiae secondary to capillaritis, and can evolve to hyperpigmented macules as a consequence of hemosiderin reabsorption. They fundamentally affect the lower limbs and are often asymptomatic.1,2
Doucas and Kapetanakis eczematoid purpura is a rare subtype of PPD characterized by itching and scaling on the petechial and hyperpigmented lesion. It was first described in 1949 by Doucas and Kapetanakis.3 It manifests clinically as a symmetrical skin eruption that mainly affects the lower extremities. The primary lesion is a group of red-violaceous punctate macules that do not disappear under pressure. It is therefore essential to include cutaneous vasculitis in the differential diagnosis. This condition can necessitate emergency consultation.4 The lesions can be isolated or can coalesce to cover larger areas, and very frequently show superficial desquamation and lichenification. They usually evolve to develop a brownish or golden coloration and can either disappear or leave a yellowish discoloration that persists for some time. Macules may be accompanied by itching and burning sensations during the period of greatest activity.
Common histological findings in PPD include a superficial perivascular lymphocytic infiltrate in the dermis, red blood cell extravasation, and hemosiderin deposits.
Treatment of PPD can be challenging. However, there is no consensus on treatment and recommendations are based on small series or case studies. Our patient responded well to treatment with topical corticosteroids, colchicine, and nicotinamide.
Conflicts of InterestThe authors declare that they have no conflicts of interest.