Topical minoxidil and oral finasteride are the only drugs approved for the treatment of androgenetic alopecia (AGA) in Spain. However, the management of this condition is highly variable because numerous treatments are used off-label. The main aim of this study was to describe the prescribing habits of dermatologists in Spain for male AGA (MAGA) and female AGA (FAGA).
Material and methodsDescriptive cross-sectional study using online questionnaires completed by dermatologists working in Spain.
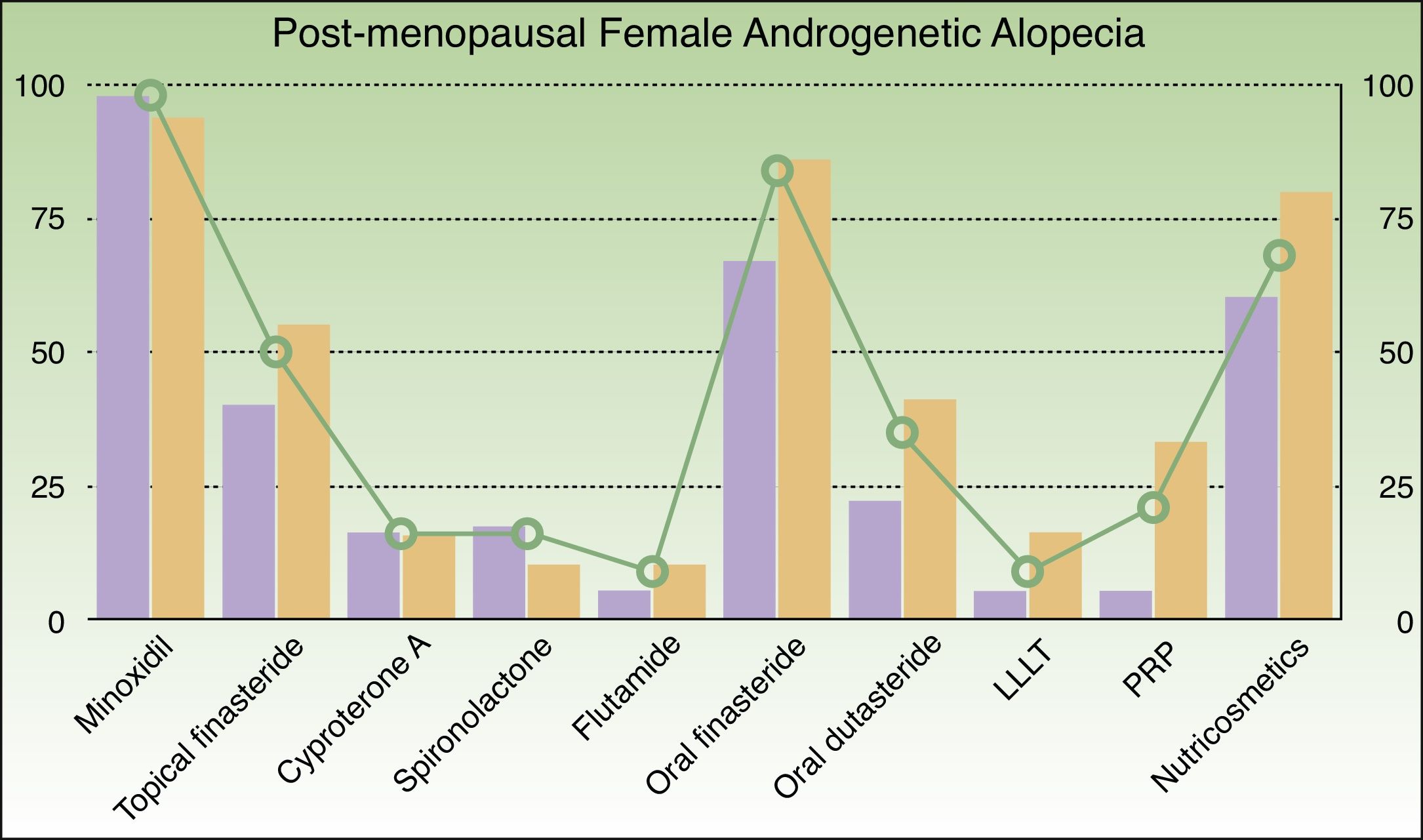
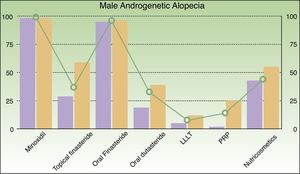
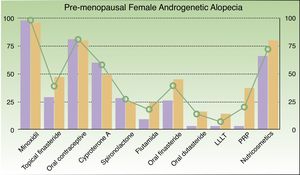
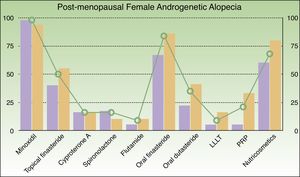
ResultsThe responses of 241 dermatologists were analyzed. The most common treatments prescribed for MAGA were minoxidil (98%), oral finasteride (96%), nutricosmetics (44%), topical finasteride (37%), oral dutasteride (33%), platelet-rich plasma (14%), and low-level laser therapy (8%). For premenopausal FAGA, the most common treatments were topical minoxidil (98%), oral contraceptives (81%), nutricosmetics (72%), cyproterone acetate (58%), oral finasteride (39%), topical finasteride (39%), spironolactone (27%), platelet-rich plasma (20%), oral dutasteride (20%), oral flutamide (18%), and low-level laser therapy (7%). Finally, for postmenopausal FAGA, the most common treatments prescribed were topical minoxidil (98%), oral finasteride (84%), nutricosmetics (68%), topical finasteride (50%), oral dutasteride (35%), platelet-rich plasma (21%), spironolactone (16%), cyproterone acetate (16%), oral flutamide (9%), and low-level laser therapy (9%).
A limitation of our study is that we did not analyze novel AGA treatments such as oral minoxidil and dutasteride mesotherapy.
ConclusionsThe most common treatments prescribed for AGA by dermatologists in Spain are topical minoxidil, oral finasteride, and nutricosmetics for MAGA and postmenopausal FAGA and topical minoxidil, oral contraceptives, and nutricosmetics for premenopausal FAGA.
A pesar de que los únicos fármacos con indicación aprobada en nuestro país para la alopecia androgénica (AGA) son minoxidil tópico y finasterida oral, es común la utilización de numerosas terapias fuera de indicación, provocando una gran variabilidad en el manejo de estos pacientes. El objetivo principal de este trabajo fue describir los hábitos de prescripción de los dermatólogos en España en AGA masculina (MAGA) y AGA femenina (FAGA).
Material y métodosEstudio descriptivo transversal mediante cuestionarios digitales autocumplimentados por dermatólogos que ejercen en territorio español.
ResultadosSe incluyeron las respuestas de un total de 241 dermatólogos. En MAGA los tratamientos más utilizados fueron en este orden: minoxidil tópico (98%), finasterida oral (96%), nutricosméticos (44%), finasterida tópica (37%), dutasterida oral (33%), plasma rico en plaquetas (14%) y láser de baja potencia (8%). En FAGA premenopáusica: minoxidil tópico (98%), anticonceptivos orales (81%), nutricosméticos (72%), acetato de ciproterona (58%), finasterida oral (39%), finasterida tópica (39%), espironolactona (27%), plasma rico en plaquetas (20%), dutasterida oral (20%), flutamida oral (18%) y láser de baja potencia (7%). En FAGA posmenopáusica: minoxidil tópico (98%), finasterida oral (84%), nutricosméticos (68%), finasterida tópica (50%), dutasterida oral (35%), plasma rico en plaquetas (21%), espironolactona (16%), acetato de ciproterona (16%), flutamida oral (9%) y láser de baja potencia (9%). Como limitaciones de nuestro estudio, no se incluyeron terapias novedosas para AGA como minoxidil oral o microinyecciones de dutasterida.
ConclusionesLos agentes terapéuticos más utilizados en MAGA y FAGA posmenopáusica por los dermatólogos en España fueron minoxidil tópico, finasterida oral y nutricosméticos, mientras que en FAGA premenopáusica fueron minoxidil tópico, anticonceptivos orales y nutricosméticos.
Androgenetic alopecia (AGA) is a condition characterized by progressive hair follicle miniaturization under certain hormonal conditions in genetically predisposed individuals.1 It is the most prevalent form of alopecia in both men and women, although its prevalence and the hair loss pattern differ between the sexes. AGA is an age-dependent disorder estimated to affect 70% of Caucasian men in their lifetime.2 In women, prevalence varies from 30% to 50% depending on the study.2–4
Untreated, AGA leads to progressive hair loss, with an annual rate of decrease in hair density of 6%.5 Despite this, there are only 2 drugs approved for the treatment of male AGA in Spain: topical minoxidil and oral finasteride. In the case of female AGA, the only approved treatment is topical minoxidil. However, many other therapies are commonly prescribed off label, a practice that has given rise to considerable variation in the management of these patients.
The primary objective of this study was to describe the prescribing habits of dermatologists in Spain for male and female AGA. The secondary objectives were to describe the relative frequency of AGA compared to other types of alopecia in the dermatology office in Spain and to evaluate the differences between the public and private sector in prescribing habits.
Patients and MethodsWe designed a cross-sectional, descriptive study based on a questionnaire. The questionnaire was completed by dermatologists working in Spain using Google Forms (see supplementary material). Respondents were asked to provide the following information: consultation setting for their patients with alopecia, distribution by population group of patients with AGA (men, premenopausal women, or postmenopausal women), and the treatments prescribed for each group. They were asked specifically about topical minoxidil, oral finisteride, topical finisteride, oral dutasteride, platelet-rich plasma (PRP), low-level laser therapy (LLLT), nutricosmetics, and hair transplantation, as well as oral contraceptives, cyproterone acetate and other oral antiandrogens in women (flutamide, spironolactone, finisteride, and dutasteride). The specific question asked relating to hair transplantation was whether the dermatologists performed hair transplantation procedures themselves. Statistical analysis was carried out using the SPSS statistical package v.24. The Chi-square test with Yate's correction when necessary was used for the comparison of proportions between different groups. Statistical significance was set at a value of P less than .05.
ResultsIn total, 241 questionnaires were included in the study. Of the respondents, 209 were staff physicians (86.7%) and 32 were residents (13.7%). Of the staff physicians, 18 (12%) treated patients in a specialized trichology unit, and the rest worked in a general office.
With respect to the sector in which the dermatologists saw patients with AGA, 58 (24%) worked in the public sector, 51 (21%) in private practice, and 132 (55%) in both sectors. The geographical distribution of the respondents by autonomous community was as follows: Madrid (24%), Andalusia (19%), Galicia (10%), Murcia (9.1%), the Balearic Islands (9%), Catalonia (5%), and others (< 5%), including Cantabria, Castile-La Mancha, Castile-Leon, Ceuta, the Valencian Community, Extremadura, the Canary Islands, La Rioja, Navarre, the Basque Country, and Asturias.
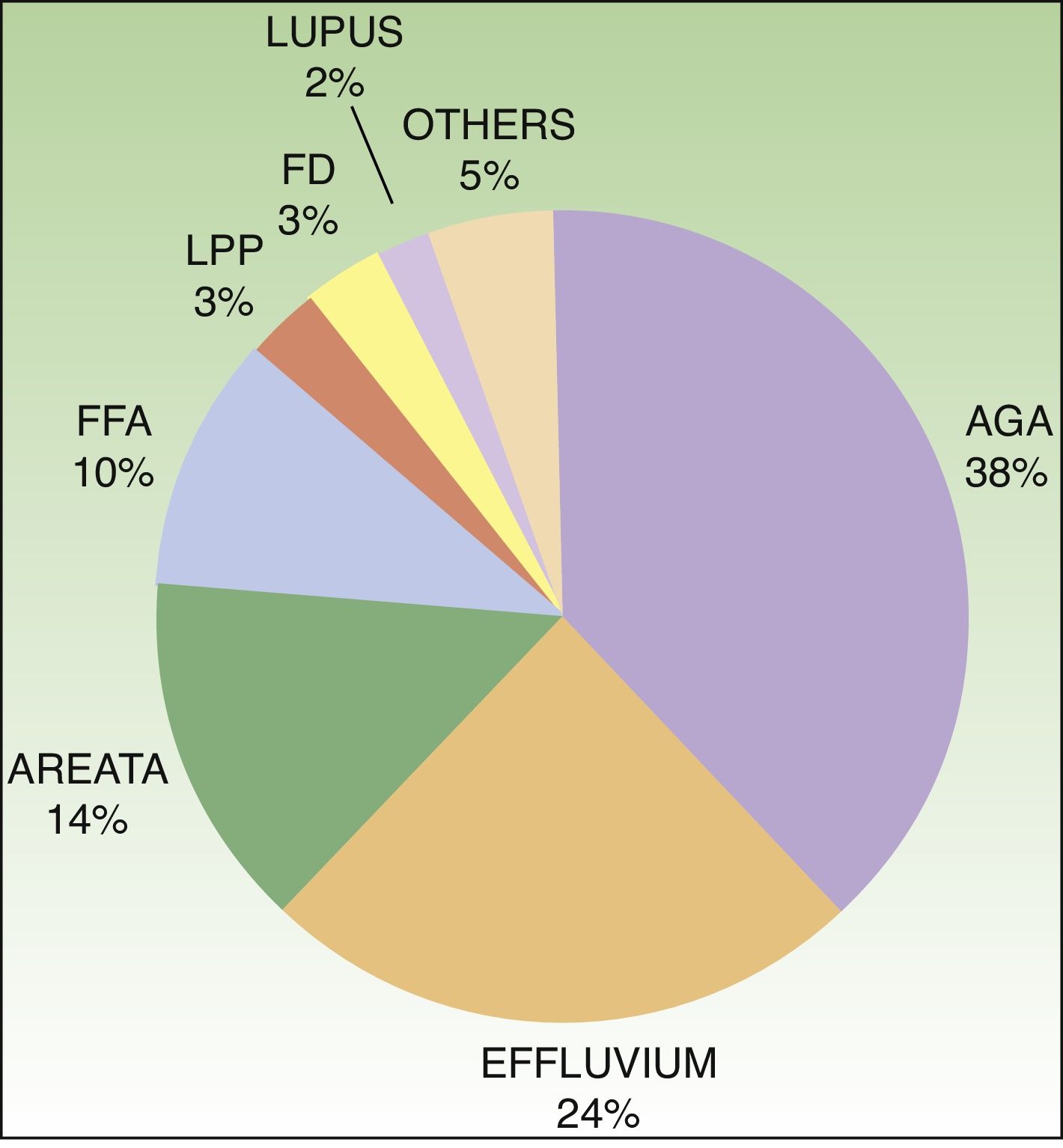
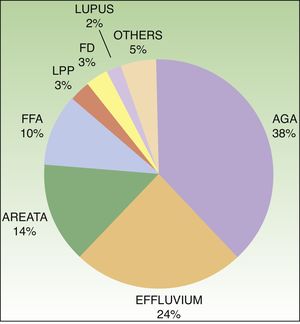
AGA was the most frequent motive for consultation (Fig. 1) in both the public and private sectors, accounting for 38% of all visits. The next most common was telogen effluvium (24%), followed by alopecia areata (14%), frontal fibrosing alopecia (10%), lichen planopilaris (3%), folliculitis decalvans (3%), lupus alopecia (2%), and other types of hair loss (5%). Statistically significant differences were found between the public and private sectors in the most frequent motive for consultation: AGA (31% vs 42%; P = .026), alopecia areata (18% vs 10%; P = .002) and fibrosing frontal alopecia (13% vs 7%; P < .001).
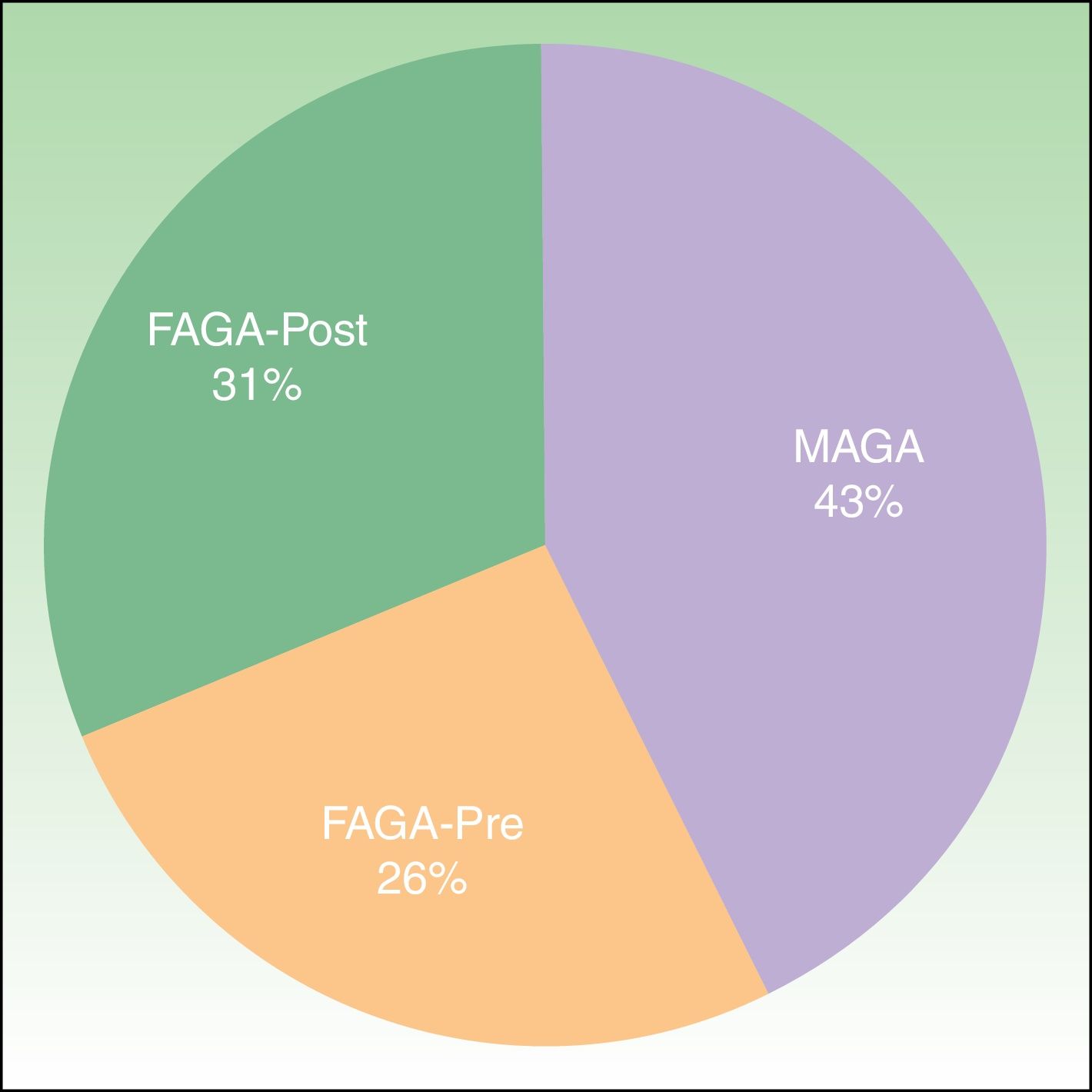
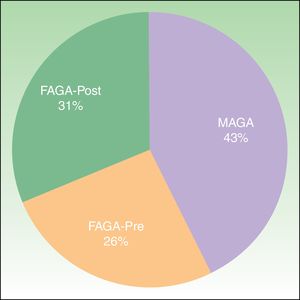
Of the patients who consulted a dermatologist because of AGA, 57% were women and 43% men. Of the women, 31% were postmenopausal and 26% were premenopausal (Fig. 2). No statistically significant differences were found between the public and private sectors in this distribution.
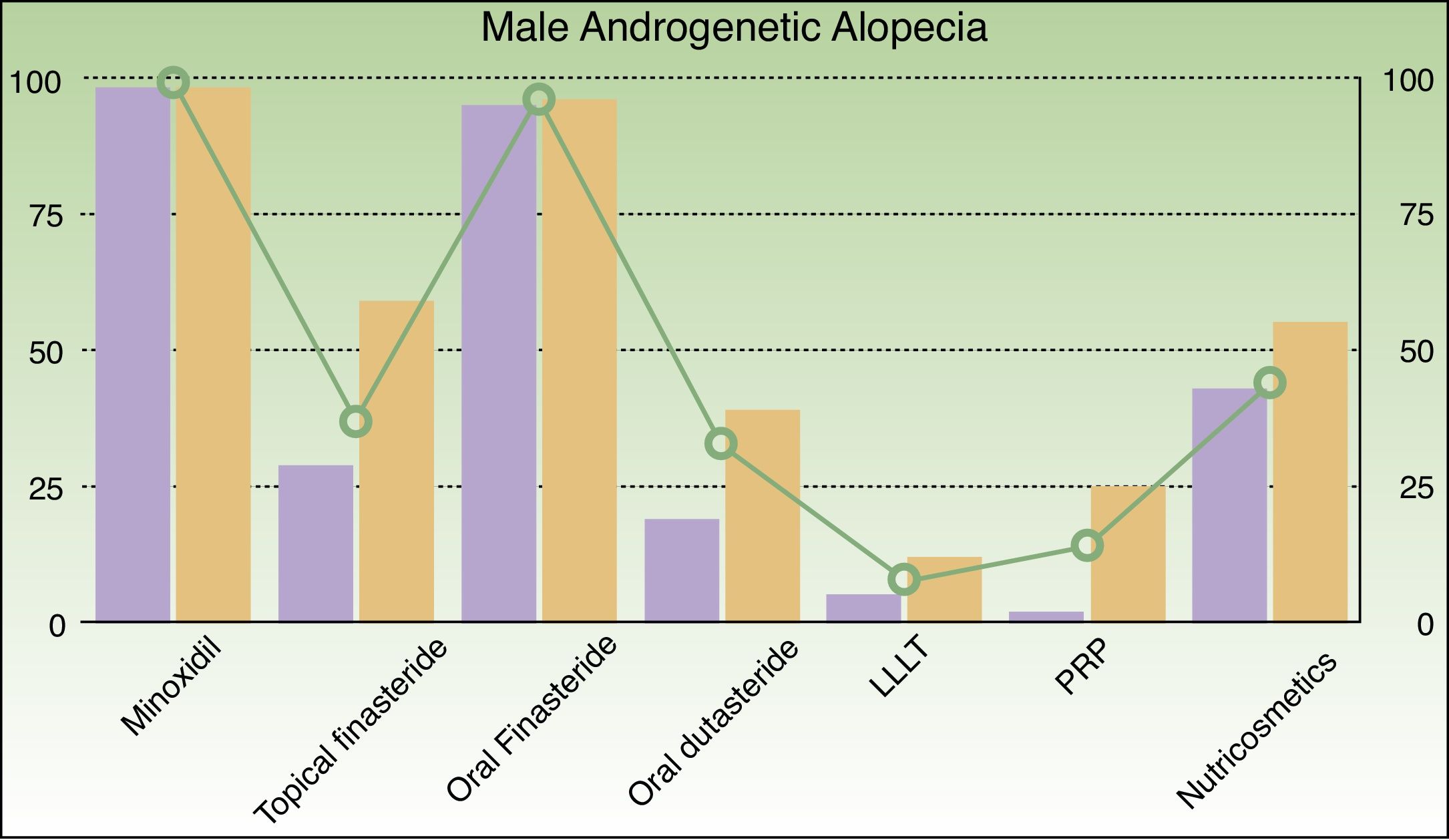
In men with AGA (Fig. 3), the most frequently prescribed treatments were as follows: topical minoxidil (98%), oral finasteride (96%), nutricosmetics (44%), topical finasteride (37%), oral dutasteride (33%), PRP (14%), and LLLT (8%). Statistically significant differences were found between the public and private sectors in the prescription of certain treatments: topical finasteride (29% vs 59%; P = .001), oral dutasteride (19% vs 39%; P < .034), LLLT (5% vs 12%; P = .012), and PRP (2% vs 25%; P < .001).
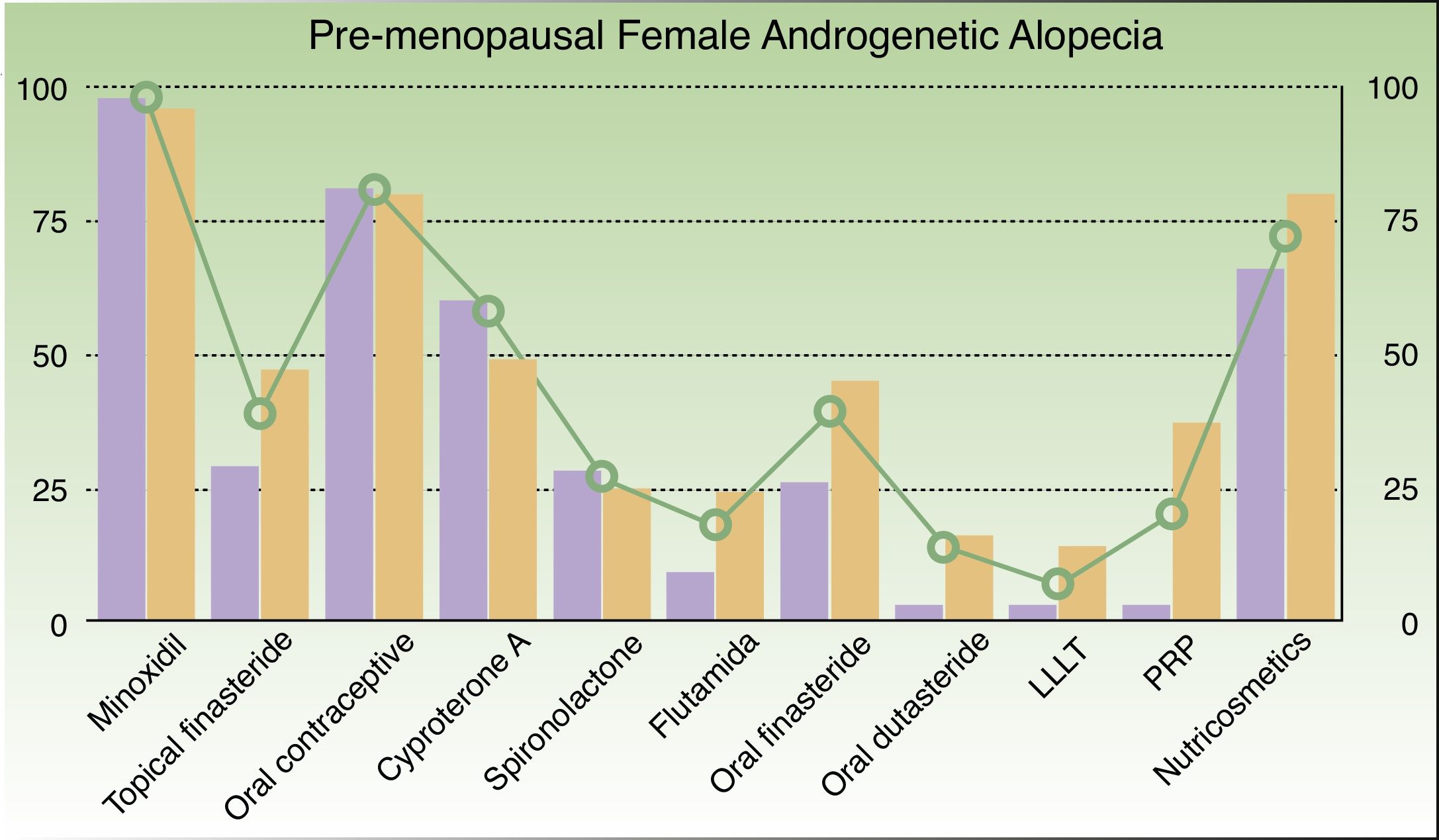
In premenopausal women with AGA (Fig. 4), the most frequently prescribed treatments were as follows: topical minoxidil (98%), oral contraceptives (81%), nutricosmetics (72%), cyproterone acetate (58%), oral finasteride (39%), topical finasteride (39%), spironolactone (27%), PRP (20%), oral dutasteride (20%), oral flutamide (18%), and LLLT (7%). Statistically significant differences were found between public vs private prescription for topical finasteride (29% vs 47%; P = .002), oral flutamide (9% vs 24%; P < .001), oral finasteride (26% vs 45%; P < .001), oral dutasteride (3% vs 16%; P < .001), LLLT (3% vs 14%; P < .001), PRP (3% vs 37%; P < .001), and nutricosmetics (66% vs 80%; P = .034).
In postmenopausal women with AGA (Fig. 5), the most frequently prescribed treatments were as follows: topical minoxidil (98%), oral finasteride (84%), nutricosmetics (68%), topical finasteride (50%), oral dutasteride (35%), PRP (21%), spironolactone (16%) cyproterone acetate (16%), oral flutamide (9%), and LLLT (9%). Significant differences were found between public and private prescription for the following drugs: oral finasteride (67% vs 86%; P < .001, oral dutasteride (22% vs 41%; P < .001), LLLT (5% vs 16%; P < .001), PRP (5% vs 33%; P < .001), and nutricosmetics (60% vs 80%; P < .001).
Of the dermatologists who responded to the survey, only 3.7% reported that they performed surgical procedures involving hair transplantation whereas 96.3% referred their patients to another specialist for this intervention.
DiscussionThe present study provides an up-to-date overview of the prescribing habits of Spanish dermatologists in patients with AGA. First, the findings confirm that AGA continues to be the most common motive for consultation in trichology, followed by telogen effluvium, alopecia areata, and frontal fibrosing alopecia. The most common scarring alopecia in our study was frontal fibrosing alopecia, confirming the dramatic increase in the incidence of this disorder suggested by earlier studies.6 Patients diagnosed with AGA reported a significant decline in quality of life. Hair loss can affect the individual's self-esteem and lead to depression.7 The high incidence of AGA and its impact on patients’ quality of life have made it the most frequent cause of consultation in trichology.
We found a similar gender distribution in patients with AGA as that reported by earlier studies: 43% men, 31% postmenopausal women, and 26% premenopausal women.2
Despite the high prevalence of AGA, there are very few approved treatments. Topical minoxidil and oral finasteride are the most studied treatments for male AGA. Both of these drugs have been shown to be effective and have good tolerability in placebo-controlled RCTs,8,9 supporting their position as first-line treatment options. In fact, most of the dermatologists surveyed cited topical minoxidil as the most commonly prescribed drug for both male AGA and pre- and postmenopausal female AGA (Fig. 6).
With respect to antiandrogens, the use of oral finasteride as a first-line treatment in male AGA is confirmed. However, despite the greater effectiveness reported for oral dutasteride,10–14 this drug is not at the top of the list of drugs prescribed in this setting. The belief that dutasteride is more likely to have an adverse effect on the patient's sex life—a supposition ruled out by a meta-analysis15—is probably a factor in the low prescription rate of oral dutasteride in patients who could benefit from its greater efficacy.
To date, only 1 published study has compared the efficacy of antiandrogen drugs in the treatment of female AGA in premenopausal women and it has been criticized for having a high risk of bias.16 Flutamide at a dose of 250mg daily for one year achieved a slight improvement in patients with alopecia, while cyproterone acetate 50mg and finasteride 5mg were considered ineffective. In our study, however, we found that cyproterone acetate was the oral antiandrogen most often prescribed in premenopausal female AGA, followed by finasteride, spironolactone, dutasteride, and oral flutamide. It should be noted that shortly after the data in the present study were collected, the Spanish Agency of Medicines and Medical Devices published an informative note on serious cases of hepatotoxicity associated with the off-label use of oral flutamide in which it advised against such use.17
Also striking is the high frequency of the prescription of nutricosmetics in both male and female AGA. Although the therapeutic effectiveness of these treatments is doubtful,18 they are used in monotherapy or as adjuvants to increase patient adherence to the medical treatments.
We also observed an increase in the prescription of 2 new therapies for AGA in both sexes: topical finasteride and LLLT.10 LLLT is an emerging light therapy. A recent review of 21 studies on the effectiveness of LLLT in male and female AGA, alopecia areata, and chemotherapy-induced alopecia showed it to be a treatment option in both male and female patients with AGA who have not responded to or were not candidates for the first-line treatments.19 While its effectiveness is supported by several scientific studies, the optimum treatment protocol and intensity or duration of treatment for LLLT has not yet been defined.20–22
We also found significant differences in prescribing habits between the public and private sectors. In general terms, topical finasteride, oral dutasteride, PRP, and LLLT were particularly used in the private sector. This difference is very likely due to the higher cost to the patient of these new treatments. In the case of PRP, a recent meta-analysis showed positive results in patients with AGA, above all in mild cases or cases with a short history, irrespective of the age or sex of the patient.23
Finally, it is striking that only 3.7% of dermatologists perform hair transplantation procedures. This may be due to a variety of reasons, including the lack of knowledge and skill in these techniques when the dermatologist was in training and the growing number of clinics run by other specialists that offer hair transplantation interventions. The added value to the patient when a dermatologist performs a hair transplantation intervention has been discussed in an earlier article.24
Our study reveals considerable variation in the clinical management of AGA in Spain. Prescription guidelines for the treatment of AGA could help to improve the situation and ensure that patients benefit from the therapies supported by the most scientific evidence.
Our study had certain limitations: no questions were included about some new treatments for AGA, including oral minoxidil (Sinclair, personal communication), and micro-injections of dutasteride.25 Furthermore, we did not calculate the optimum sample size before carrying out the study and we did not monitor the distribution of the survey; as a result it was impossible to determine the percentage of response. Since the results of the study are based on the responses of the dermatologists who completed the survey, they could be affected by memory bias.
ConclusionsThe treatments most prescribed by dermatologists in Spain for male AGA and female AGA in postmenopausal women were topical minoxidil, oral finasteride, and nutricosmetics. In premenopausal women, the most common treatments were topical minoxidil, oral contraceptives, and nutricosmetics. AGA was the most common motive for consultation among patients with hair loss, followed by telogen effluvium, alopecia areata, and frontal fibrosing alopecia. Treatment with topical finasteride, oral dutasteride, PRP, and LLLT were more often prescribed in the private sector.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank the members of the Dermachat working group for their collaboration in this study.
Please cite this article as: Pindado-Ortega C, Saceda-Corralo D, Buendía-Castaño D, Fernández-González P, Moreno-Arrones ÓM, Fonda-Pascual P, et al. Estudio transversal acerca de los hábitos de prescripción en alopecia androgénica de los dermatólogos en España en 2017. Actas Dermosifiliogr. 2018;109:536–542.