Tumor thickness is of great importance in the management of cutaneous malignant melanoma (MM): this variable not only affects prognosis but is also a key factor in planning surgical margins and selecting candidates for sentinel node biopsy. Breslow depth is the standard histologic measure of thickness, but technological advances have provided imaging techniques such as cutaneous ultrasound that can potentially assess tumor thickness and enable prompt initiation of definitive treatment.
Objectivesa) To evaluate the utility of ultrasound assessment of tumor thickness in MM, and b) to analyze histologic variables that affect ultrasound assessments of thickness.
Materials and methodsRetrospective study of a consecutive series of 79 primary cutaneous MMs in which tumor thickness had been assessed by 15-MHz ultrasound before surgery. We gathered data from histology reports, studying Breslow depth and the presence of ulceration, regression, inflammatory infiltrate, and associated nevi. Correlation coefficients were calculated to evaluate the strength of association between Breslow depth and thickness assessed by ultrasound. We also calculated the sensitivity, specificity, and positive and negative predictive values of ultrasound measurement in the diagnosis of MMs more than 1mm thick. Associations between histologic variables and the overestimation of thickness by ultrasound were also analyzed.
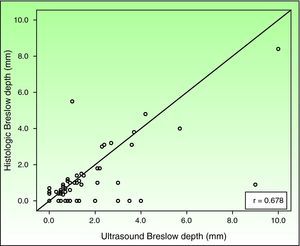
ResultsThe 79 primary MMs studied had a mean (SD) Breslow depth of 0.8 (1.4) mm. There was moderate correlation and agreement between Breslow depth and the ultrasound assessment of thickness (Pearson correlation coefficient, 0.678; intraclass correlation coefficient, 0.78). The tendency of ultrasound to overestimate thickness was nonsignificantly related to the presence of a moderate to intense infiltrate and associated nevi (P>.05). The sensitivity of ultrasound for the diagnosis of MM over 1mm thick was 82%; specificity was 80%, and positive and negative predictive values were 54% and 94%, respectively.
ConclusionsUltrasound imaging quite correctly identifies thin MMs and can be useful for planning adequate surgical margins; however, there are limitations on its usefulness in the diagnosis of thick MMs. Additional studies are required to confirm whether certain histologic characteristics, such as the presence of a moderate to intense inflammatory infiltrate or associated nevi can lead to overestimation of thickness by ultrasound, limiting the clinical utility of this imaging technique in MM management.
El espesor tumoral es una variable de gran trascendencia en el manejo clínico del melanoma maligno cutáneo (MMC), ya que no solo establece el pronóstico, sino que además determina la planificación de márgenes quirúrgicos y selecciona a aquellos pacientes candidatos a biopsia selectiva de ganglio centinela. El índice de Breslow (IB) es el procedimiento histométrico estándar para la determinación del espesor tumoral del melanoma. El desarrollo de técnicas de imagen, como la ecografía cutánea (EC), plantea la posibilidad de realizar una estimación no invasiva que agiliza la instauración del tratamiento definitivo.
Objetivosa) Evaluar la EC como instrumento de medición del espesor tumoral en el MMC, y b) analizar los factores histológicos que influyen en la estimación del espesor ecográfico.
Material y métodosEstudio retrospectivo de una serie consecutiva de 79 melanomas cutáneos primarios. En todos los casos, se practicó un estudio ecográfico preoperatorio con una sonda de 15 Mhz para la determinación del espesor tumoral (EE). Se analizaron los exámenes histológicos, estudiándose el IB, además de la presencia de ulceración, regresión, infiltrado inflamatorio y nevus. Se estudian el grado de correlación y el nivel de concordancia entre los valores de EE e IB. Se estiman la sensibilidad, la especificidad y los valores predictivos de la EC en el diagnóstico de melanomas de espesor >1mm. Se analiza la relación de las variables histológicas en la determinación del EE.
ResultadosSe estudian 79 melanomas primarios, IB medio: 0.8mm (DE: 1,4). La EC evidenció un grado de correlación y un nivel de concordancia moderado con respecto al IB (coeficiente de correlación de Pearson: 0.678, coeficiente de correlación intraclase: 0.78, respectivamente). La EC mostró tendencia a sobrestimar el espesor histológico en relación con la presencia de infiltrado inflamatorio moderado-intenso y nevus, sin alcanzar significación estadística (p>0.05). La EC mostró valores de sensibilidad y especificidad, y valores predictivos positivo y negativo para el diagnóstico de melanomas gruesos (>1mm) del 82, el 80, el 54 y el 94%, respectivamente.
ConclusiónLa EC permite discriminar con bastante precisión melanomas finos y planificar márgenes quirúrgicos adecuados, pero presenta limitaciones para el diagnóstico de melanomas gruesos. Son necesarios más estudios para confirmar si determinadas características histológicas del tumor, como la presencia de infiltrado inflamatorio moderado-intenso y nevus, pueden condicionar una sobrestimación del espesor ecográfico, limitando su aplicabilidad clínica en el manejo del MMC.
Tumor thickness is of great importance in the management of cutaneous malignant melanoma because it is used to determine the prognosis and is a key factor in planning surgical margins and selecting candidates for sentinel node biopsy.1
Breslow depth is the standard measure of tumor thickness in primary cutaneous melanoma.2 A histologic measurement, Breslow depth requires a preoperative excisional skin biopsy and, in addition to being invasive, the procedure may delay definitive surgical treatment because it involves a 2-stage intervention.Cutaneous ultrasound is a noninvasive imaging technique for visualizing the interior layers of the skin. The use of this tool in the field of dermatology has been studied in recent years.2 Although the majority of early studies used 20-MHz probes capable of measuring lesions at a depth of 6 to 8mm, many others used lower-resolution probes (10-15MHz) because these were available in most hospitals. However, the current trend is to use higher-resolution probes (75-100MHz), which measure lesions confined to the epidermis and dermis more accurately. In cutaneous malignant melanoma, cutaneous ultrasound offers the possibility of estimating tumor thickness in vivo, thus avoiding excisional biopsy and speeding up surgical treatment planning.3–5 Results of recent studies of the validity and utility of cutaneous ultrasound in the management of cutaneous malignant melanoma have been inconsistent.6–12
The aim of this study was to evaluate cutaneous ultrasound as a tool for measuring tumor thickness in cutaneous malignant melanoma. The histologic variables that affect ultrasound assessment of tumor thickness are also analyzed.
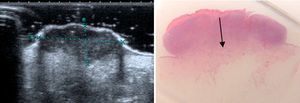
Material and MethodsThis retrospective study evaluated the records of a consecutive series of patients with cutaneous malignant melanomas who underwent surgery between 2008 and 2010 in the dermatology department of the Hospital Costa del Sol. In all cases, members of the hospital's radiology department had performed a preoperative assessment of the lesion using a Toshiba Aplio XG 15-Mhz ultrasound probe to determine tumor thickness. Tumor thickness had been calculated automatically as the maximum vertical distance from the entry echo to the lowest hypoechoic signal, expressed in mm (Fig. 1). The histologic measure of thickness (Breslow depth) had been determined by a pathologist experienced in dermatopathology using an ocular micrometer to measure the maximum distance between the highest level of the stratum granulosum of the epidermis and the deepest point of the tumor, expressed in mm (Fig. 1). The histologic presence of ulceration, regression (absent, < 50%, > 50%), inflammatory infiltrate (absent, mild, moderate, severe), and associated nevi had also been recorded.
The study was approved by the ethics committee of Hospital Costa del Sol.
Statistical AnalysisWe compared the ultrasound measurement of tumor thickness against the results obtained with the gold standard method (Breslow depth), using the Pearson correlation coefficient and the intraclass correlation coefficient to quantify the degree of correlation and agreement between the 2 variables. To study the association between histologic variables (ulceration, regression, inflammatory infiltrate, and presence of nevi) and ultrasound assessment of thickness, bivariate analysis was performed, taking as the dependent variable the overestimation of thickness by ultrasound (+ 0.1mm) compared with Breslow depth, using χ2 tests and, where appropriate, the Fisher exact test. Statistical significance was set at P<.05. Finally, we studied the sensitivity, specificity, and positive and negative predictive values of cutaneous ultrasound against those of the gold standard for the correct classification of thick melanomas (Breslow depth > 1mm) with a 95% CI.
ResultsWe studied 79 melanomas from 79 patients (53% of them women) with a mean (SD) age of 56.8 (16.2) years; 42% were located on the trunk, 40% on the limbs, and 18% on the head and neck. Melanomas in situ accounted for 45% of the tumors (n=35) and the remaining 55% were invasive tumors (n=44; 27 melanomas ≤ 1mm, 17 melanomas > 1mm). The mean Breslow depth of the series was 0.8 (1.4) mm. The mean thickness as measured by ultrasound was 1.2 (1.7) mm. The histologic findings are summarized in Table 1.
The Pearson correlation coefficient between ultrasound assessment of thickness and Breslow depth was 0.678 (P<.001) (Fig. 2). The value of the intraclass correlation coefficient measuring agreement between the ultrasound assessment of thickness and Breslow depth was 0.78 (95% CI, 0.61-0.88).
Bivariate analysis showed that ultrasound tended to overestimate tumor thickness in the presence of moderate to severe inflammatory infiltrate and nevi, though this tendency was not statistically significant (P>.05) (Table 2).
Relationship of Ultrasound Assessment of Thickness and Histological Variables.
| No Overestimation | Overestimation (+ 0.1 mm) | P | |||
| n | % | n | % | ||
| Regression | |||||
| Absent | 4 | 80.0 | 1 | 20.0 | 0.43 |
| < 50% | 38 | 58.5 | 27 | 41.5 | |
| > 50% | 4 | 44.4 | 5 | 55.6 | |
| Ulceration | |||||
| Yes | 2 | 33.3 | 4 | 66.7 | 0.23 |
| No | 44 | 60.3 | 29 | 39.7 | |
| Inflammatory infiltrate | |||||
| Absent-mild | 28 | 65.1 | 15 | 34.9 | 0.26 |
| Moderate-severe | 18 | 50.0 | 18 | 50.0 | |
| Associated nevus | |||||
| Yes | 10 | 43.5 | 13 | 56.5 | 0.15 |
| No | 36 | 64.3 | 20 | 35.7 | |
Classic sensitivity tests showed that the sensitivity of ultrasound for the diagnosis of thick melanomas (Breslow depth > 1mm) was 82%, specificity was 80%, and positive and negative predictive values were 54% and 94%, respectively (Table 3).
DiscussionIn this study we analyzed the accuracy of cutaneous ultrasound as a tool for measuring tumor thickness in a consecutive series of 79 primary melanomas. Of interest is the high proportion of minimally invasive melanomas in situ, a finding that we attribute to the systematic use of dermoscopy in the diagnosis of pigmented skin lesions and to the continuous application of primary prevention strategies in our population.
We found moderate correlation and agreement between ultrasound and histologic measures, whereas most earlier studies6–10 have reported good correlation. Tacke et al.,6 using a 20-MHz probe on a series of 259 melanomas, reported a correlation coefficient of 0.88 (lesions of 0.55 to 0.95mm were classified incorrectly by ultrasound in 34% of cases and lesions of 1.30 to 1.70mm were classified incorrectly in 50% of cases). Conversely, Serrone et al.,7 using a 20-MHz probe on a series of 261 lesions, reported a correlation coefficient of 0.95 in melanomas larger than 1.51mm, finding the lowest correlation in lesions smaller than 0.75mm. The results reported by Kaikaris et al.,8 using a 14-MHz probe, were similar (r=0.283 in melanomas of 1–2mm and r=0.869 in melanomas larger than 2mm). Many factors make comparison between studies difficult, including the use of diverse probes, differences between the series studied, the inclusion of benign lesions (mainly nevi),7 and the exclusion of in situ lesions9 in the belief that ultrasound does not visualize epidermal lesions.
Some histologic features of tumors may alter the ultrasound assessment of thickness.10 Hoffman et al.11 found that the cause of 80% of cases of overestimation was the presence of inflammatory infiltrate. In our series, cutaneous ultrasound tended to overestimate tumor thickness in comparison with the histologic measure in the presence of moderate to severe inflammatory infiltrate and associated nevi, though no statistical significance was found (P>.05). These histologic features act as artifacts and interfere with the ultrasound assessment of the tumor because cutaneous ultrasound does not differentiate between tumor cells and inflammatory or nevus cells.
The sensitivity, specificity, and positive and negative predictive values for the diagnosis of thick melanomas (>1mm) were 82%, 80%, 54%, and 94%, respectively. These results suggest that cutaneous ultrasound would properly stage the tumor and allow a single surgical intervention to be planned in approximately 80% of melanomas. However, it would not provide an accurate measurement on which to base a therapeutic decision in 20% of melanomas. Cutaneous ultrasound showed high discriminatory capacity for thin melanomas but was less successful at discriminating thick melanomas. Some authors have developed diagnostic algorithms that increase the diagnostic accuracy for thick melanomas by combining clinical, dermoscopic, and ultrasound findings, reaching a sensitivity of 97% and a specificity of 100%.12
Almost half the melanomas assessed by ultrasound as thick were in fact thin (< 1mm). This finding is explained by the frequent association of inflammatory infiltrate and nevi with the melanomas in our series. This tendency towards overestimation can be remedied by using higher-frequency probes, which have a higher resolution.13
The results of one study, in line with our findings, showed a particularly good correspondence between ultrasound and histologic measurements using a 30-MHz probe when the lesions were smaller than 1mm in a series of 68 melanomas and an even better correspondence in lesions on the sole (r=0.945).14 In contrast, Machet et al.,15 using a 20-MHz probe, found lesions on the sole to be difficult to measure because of the thickness of the stratum corneum.
In the ultrasound estimation of tumor thickness our results contrast with those published in a recent prospective study of 54 cutaneous malignant melanomas, which reported sensitivity, specificity, and positive and negative predictive values in the diagnosis of thick melanomas (> 1mm) of 86%, 97%, 95%, and 91%, respectively.16 The diagnostic accuracy of cutaneous ultrasound in that study was striking despite the lower ultrasound resolution of the probe used by the authors (10 Mhz). These results could be explained by the high proportion of melanomas later found to be thick on histology, which would be more accurately measured by ultrasound assessment because the presence of other histologic factors would not alter their ultrasound assessment as thick melanomas.
The present study had several limitations. The small size of our series made it difficult to interpret the results with regard to the influence of histologic findings on the ultrasound assessment of thickness, so it was not possible to establish causal relationships between histologic and ultrasound findings. Interpersonal variability may interfere in the ultrasound assessment of tumor thickness, though the use of standardized procedure minimizes this bias.
Technological advances in ultrasound, such as the use of contrast agents,5 and the incorporation of new in vivo microscopy techniques, including dermoscopy17,18 and confocal microscopy,19 are encouraging and their combined use will improve the preoperative diagnosis of melanoma in the near future.
In conclusion, cutaneous ultrasound is a tool of great interest in the preoperative study of cutaneous malignant melanoma. It identifies thin melanomas fairly accurately and can be useful for planning appropriate surgical margins. Further studies are necessary to confirm whether certain histologic characteristics of the tumor, such as the presence of moderate to severe inflammatory infiltrate and associated nevi, can lead to an overestimation of thickness by ultrasound, limiting the clinical utility of this imaging technique in the management of cutaneous malignant melanoma.
Ethical ConsiderationsProtection of persons and animalsThe authors state that no experiments on humans or animals were performed in this study.
Data confidentialityThe authors state that no patient data appear in this article.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Canedo I, et al. Evaluación de la ecografía cutánea de 15 Mhz en la estimación preoperatoria del espesor tumoral en el melanoma maligno. Actas Dermosifiliogr. 2013;104:227–31.