Dermatology plays a fundamental role in the health of the trans community and the LGTBIQ+ collective (an acronym for lesbians, gays, trans, bisexuals, intersex, “queer” and other identities).
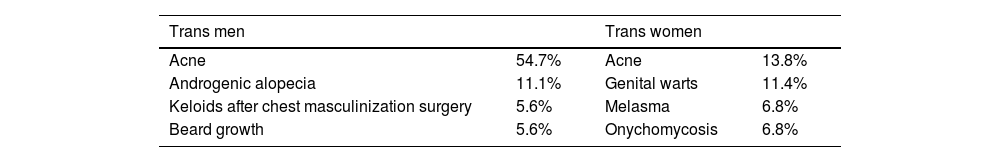
In 2021, a dermatological clinic exclusive to trans and non-binary patients was established in a public hospital in Argentina. Below, the most frequent reasons for consultation observed in this community will be described (Table 1).
Over 23 months (from June 2021 through April 2023), a total of 109 patients were treated: 49.5% trans men (TM), 40.4% trans women (TW), 9.2% non-binary (NB), and only 0.9% gender fluid.
In TM treated with testosterone hormone therapy, acne typically begins 6 months into therapy and improves within 1 to 2 years. The use of intramuscular testosterone undecanoate—1000mg applied quarterly with the target of reaching blood levels between 3.5 and 7 ng/mL—has wider plasma peaks vs its topical presentation, which may also contribute to acne.1,2 In cases of hormone therapy-induced acne, it is often necessary to treat mild acne as if it were moderate.
For patients with severe acne (Fig. 1), nodulocystic or scarring, isotretinoin is the drug of choice.3 If the patient has not had surgery that damages their ability to conceive, and they have vagina-penis intercourse, even while on hormone therapy and experiencing amenorrhea, it is necessary to prescribe hormonal contraceptives. Progestins are preferred as they do not interfere with hormone therapy.4
The risk of developing androgenic alopecia in TM is lower vs cis men and usually occurs 3 to 5 years after starting testosterone. Therapy consists of applying topical and/or oral 5% minoxidil (1 to 5mg doses). Topical use on the beard area or oral intake are effective options to achieve the beard density desired by these patients.5
Although finasteride and dutasteride do not interfere with serum testosterone levels, their use should be delayed until secondary sexual characteristics have developed completely, which occurs around 2 years. It is essential to assess the desire for gestation, as these drugs are contraindicated during pregnancy.6
Another frequent reason for consultation for TM is scars after chest masculinization surgery (Fig. 2). Treatment options include intralesional corticosteroids, 5-fluorouracil, silicone patches, 5% imiquimod, and surgical excision. In our experience, we administered monthly intralesional injections with triamcinolone 6mg/mL and 5-fluorouracil 50mg/mL plus topical 5% imiquimod applied 5 times a week, with good results.7
Hormone treatment in TW involves estradiol—either orally or transdermally—which can also be combined with spironolactone or cyproterone acetate due to its anti-androgenic action.8
In TW, hair removal should be seen as a medical necessity and is essential to perform this procedure before any genital surgical procedures.8 Non-permanent hair removal techniques can cause pseudofolliculitis of the lower jaw. The ideal treatment is laser hair removal, either diode or Alexandrite, and the discontinuation of mechanical hair removal methods. Topical treatment with retinoids, low-potency corticosteroids, benzoyl peroxide, or clindamycin can also be prescribed.8
Melasma is another common reason for consultation in TW on hormone therapy.8 Of note that they may view it positively as it usually affects more cis women.
Facial and body feminization through fillers is a common procedure in TW. Currently, silicone injections are prohibited due to the high morbidity and mortality risk involved.2,8
In our experience, TW patients who consulted for siliconomas were sex workers with a past medical history of human immunodeficiency virus (HIV). A 3-to-6-month regimen of topical corticosteroids+minocycline 200mg/day was prescribed with poor therapeutic response.
The high prevalence of venereal infections in the trans population supports the implementation of voluntary testing for HIV and other venereal infections.8,9 Dermatology consultations should be an opportunity to educate about safe sexual practices.2
In our experience, we observed a high prevalence of HIV in TW sex workers. In contrast, no TM was infected with the virus.
Among NB patients, consultations were not associated with hormonal or surgical gender affirmation practices, as most had not undergone them. The most common reason for consultation was androgenic alopecia.
In conclusion, the trans community presents specific dermatoses due to gender affirmation processes that require individualized therapies.
For an inclusive consultation, a respectful environment is essential using appropriate pronouns and not assuming the patient's gender identity, genitality, or sexuality. Moving towards a non-binary model of medicine may be the first step for the LGTBIQ+ community to access the health care system through prevention rather than illness.9,10
Conflicts of interestNone declared.