A 43-year-old woman with Fitzpatrick skin type II and no personal or family history of skin cancer presented with a tumor nodule of 4 months’ duration on her forehead; no other physical findings were observed.
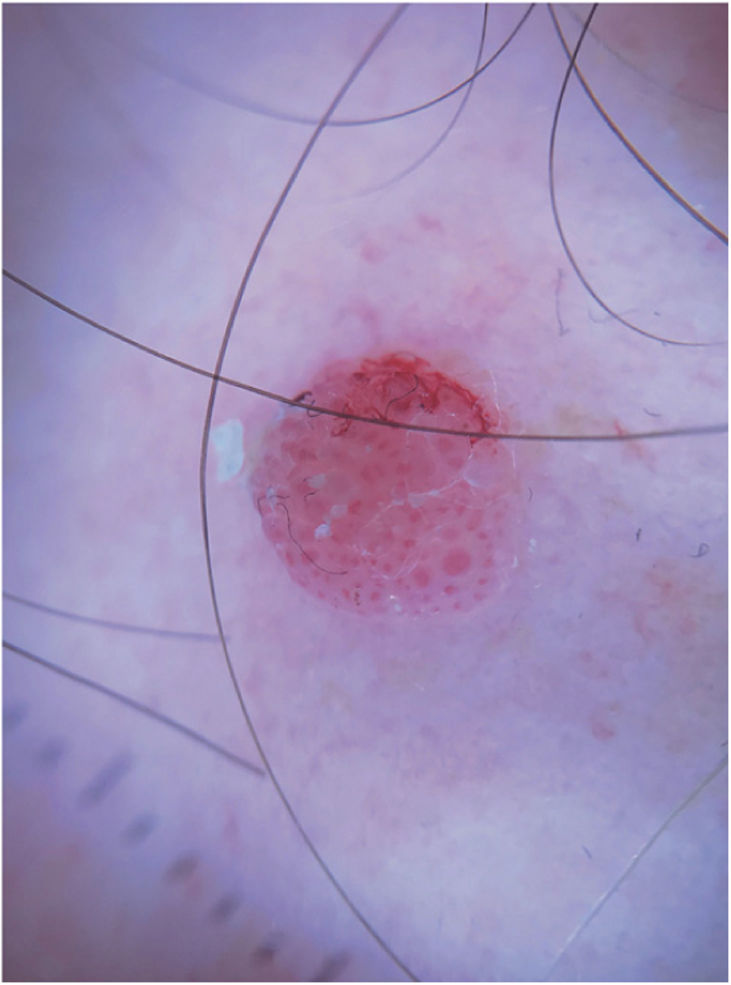
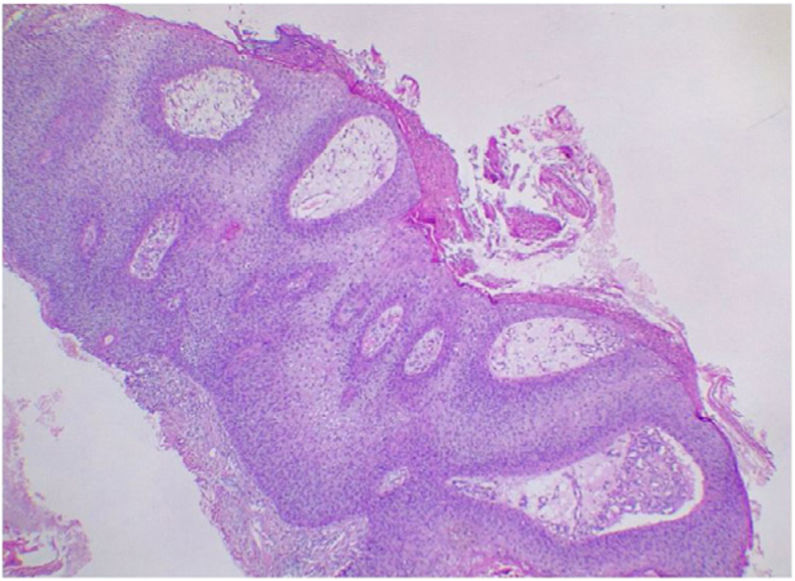
Physical ExaminationThe nodule was a pink hemispheric friable tumor with a diameter of 6mm and a tendency to bleed (Fig. 1). Dermoscopy showed central red blood cells and peripheral glomerular and hairpin vessels against a whitish background. Other findings included a hemorrhagic area and the fabric fiber sign (Fig. 2).
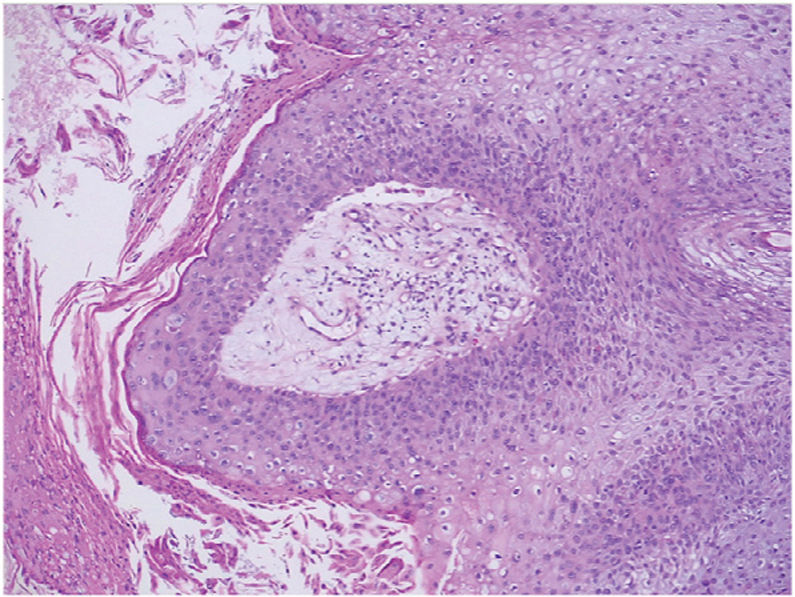
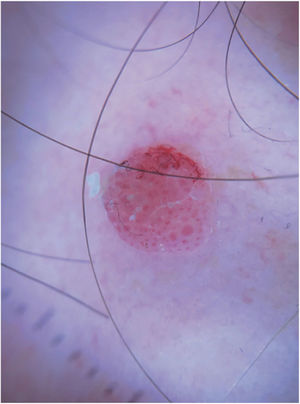
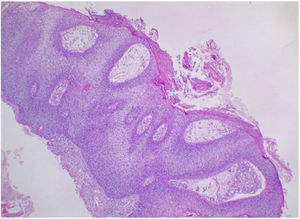
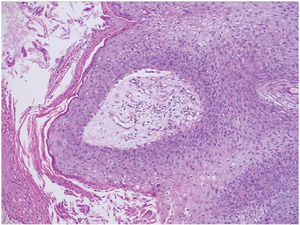
HistopathologyHistopathologic examination with hematoxylin and eosin staining showed hyperkeratosis, parakeratosis, papillomatosis, and acanthosis due to the presence of mature basaloid and squamous cells, with the latter tending to form characteristic eddies. Granular cells with perinuclear vacuolation and keratohyalin granules of varying sizes were observed in some of the superficial layers (Figs. 3 and 4).
What Is Your Diagnosis?.
DiagnosisInverted keratosis follicularis.
Clinical Course and TreatmentThe nodule was initially treated by shave biopsy, but it recurred. It disappeared completely after 3 cycles of cryosurgery administered at 3-week intervals.
CommentInverted keratosis follicularis is a rare benign adnexal tumor originating from the infundibular portion of the hair follicle.1
It is most often located in the head and neck region and is slightly more common in men. It typically presents as a solitary unpigmented exophytic tumor that grows progressively over months or years. The differential diagnosis includes various keratinizing lesions, such as squamous cell carcinoma, viral warts, and seborrheic keratosis, and other tumors such as basal cell carcinoma.2 Pigmented forms of inverted keratosis follicularis can simulate melanoma.3,4
Diagnosis is based on histologic findings, as clinical forms can mimic a range of conditions. Histopathology shows papillomatosis, acanthosis, and characteristic squamous eddies.5
Dermoscopy is not pathognomonic, but it can help reach a diagnosis. The most common findings are radially arranged hairpin vessels surrounded by a whitish halo with a keratotic center or a yellow-whitish amorphous central area surrounded by vessels in a radial pattern; less common findings, seen in our patient, are pink blood cells surrounded by a whitish halo.6
Excision or destruction is the standard treatment for inverted follicular keratosis given its benign nature. Resolution following application of imiquimod cream 3 times a week for 8 weeks has been reported.7
Conflicts of InterestThe authors declare that they have no conflicts of interest.