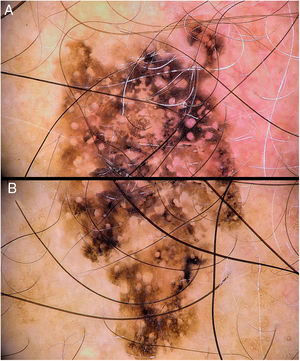
A 54-year-old man visited our department for assessment of a skin lesion in the parietal area, which had been growing gradually since it was detected the previous year. The lesion was a dark-brown and black macule with irregular borders, measuring 15 mm at its largest diameter (Fig. 1).
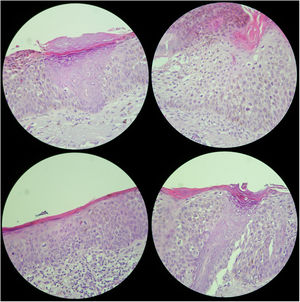
What is your diagnosis?Pigmented Bowen disease (Fig. 2).
CommentDermatoscopy revealed dark-brown and black pigmented areas with a granular appearance, sparing the follicular orifices, together with a pigmented pseudonetwork. No hyperkeratotic areas, scabs, or vascular structures were observed. The surrounding skin presented clear signs of photoaging. An excision biopsy of the lesion confirmed the diagnosis of pigmented Bowen disease (with clearly atypical cytology, with abnormal anisokaryosis and mitosis, as well as lack of involvement of the acrosyringia) with a central area showing a lichenoid infiltrate, with intense surrounding solar elastosis (Fig. 3).
Bowen disease is defined as an intraepidermal carcinoma. It occurs more frequently in women over 60 years of age and is located in regions subject to chronic exposure to sunlight. In overall terms, it may give rise to squamous cell carcinoma in between 3% and 5% of cases.1 The pigmented variety is considered to be rare (less than 2%, according to a series of more than 400 cases2). Different dermoscopic findings have been reported for this entity, including whitish desquamation, black or brown scabs, areas that appear to show regression, pigment (brown or greyish-blue in granular distribution, imitating remains of an atypical network, like globules or irregularly distributed areas of pigment), hypopigmented areas, variable vascular pattern (predominantly glomerular, or atypical—punctate, linear, arboriform, or forked).3–5
The clinical and dermatologic presentation of Bowen disease is highly variable. They can often be difficult to differentiate from those of seborrheic keratosis, actinic keratosis, or even the pigmented variety of melanocytic lesions.
We report a case of Bowen disease with an unusual clinical and dermoscopic presentation. Although epiluminescence provided orientation regarding the nature of the lesion and made it possible to consider a differential diagnosis that included pigmented actinic keratosis as the most probable option, the biopsy for diagnosis by means of histology is essential.
Please cite this article as: Martin-Gorgojo A, Comunión-Artieda A, Guzmán-Sierra A. Mácula pigmentada en cuero cabelludo. Actas Dermosifiliogr. 2021;112:61–62.