Necrobiosis lipoidica is a rare chronic granulomatous disease. Multiple treatment approaches are available, but results are generally minimal and inconsistent. Some publications report variable results with photodynamic therapy (PDT) as a second line of treatment for refractory cases. We report 4 cases of necrobiosis lipoidica treated satisfactorily with conventional PDT using methyl aminolevulinate or 5-aminolevulinic acid BF-200 as the photosensitizing agent. All 4 patients were women with diabetes mellitus who had undergone treatment at least twice in the past, with little improvement. The lesions resolved completely with PDT, leaving only residual atrophy after a mean of 3.2 sessions per lesion.
La necrobiosis lipoidica (NL) es una enfermedad granulomatosa crónica poco frecuente para la que existen multitud de tratamientos disponibles. No obstante, estos ofrecen habitualmente mínimos e inconsistentes resultados. En algunas publicaciones se describe el tratamiento con terapia fotodinámica (TFD) como tratamiento de segunda línea en casos refractarios, con resultados variables. Comunicamos cuatro casos de NL tratados satisfactoriamente con TFD convencional con MAL y BF-200 ALA. Las cuatro pacientes eran mujeres afectas de diabetes mellitus y todas habían recibido al menos 2 tratamientos previos con escaso resultado. Tras una media de 3,2 sesiones de TFD por lesión, las cuatro pacientes presentaron una resolución completa de las lesiones, persistiendo únicamente atrofia residual.
Necrobiosis lipoidica (NL) is a rare, chronic, granulomatous disease that typically affects young women and is frequently associated with diabetes mellitus (DM).1 Clinically, the disease is characterized by the progressive appearance of plaques with a raised red-violaceous border and an atrophic yellow-brown center. The plaques are usually located bilaterally on the anterior surface of the lower extremities. Other less common locations include the upper extremities, face, and scalp.2,3 Although they are typically asymptomatic, some patients may experience pruritus, dysesthesia, or pain.1–3 Histologically, they are characterized by degeneration of collagen, formation of granulomas in palisade and thickening of the vascular walls.4
NL has historically been a difficult disease to treat. Several therapeutic options are available, although most of them provide minimal and inconsistent results.1 Some publications describe the use of photodynamic therapy (PDT) as second-line treatment in refractory cases, with variable results.5–8
We describe our experience in the treatment with PDT of 4 patients with NL.
Case DescriptionsTable 1 shows the clinical characteristics of the 4 patients treated in our department using PDT.
Clinical Characteristics of Patients Treated With Photodynamic Therapy: Age, Medical History, Time Since Onset of the Disease, Treatments Previously Received, Number of Sessions Administered, Photosensitizing Agent Administered, Response Observed, and Follow-up Time From End of Treatment.
| Case | Age | Medical History | Time Since Onset, mo | Previous Treatments | No. of Sessions | Photosensitizing Agent | Response | Follow-Up Time, mo |
|---|---|---|---|---|---|---|---|---|
| 1 | 21 | DM1, Graves-Basedow | 72 | Pentoxifylline, ASA, clobetasol, tacrolimus, calcitriol, PDL | 11 | MAL | Complete | 14 |
| 2 | 32 | DM1 | 8 | Pentoxifylline, clobetasol | 18 | MAL | Complete | 2 |
| 3 | 22 | DM1 | 120 | Clobetasol, pimecrolimus, PDL | 10 | MAL, BF-200 ALA | Complete | 7 |
| 4 | 61 | DM2, leiomyosarcoma | 2 | Clobetasol, cryotherapy | 6 | MAL, BF-200 ALA | Complete | 6 |
Abbreviations, ASA indicates acetylsalicylic acid; BF-200 ALA, 5-aminolevulinic acid; DM1, type 1 diabetes mellitus; DM2, type 2 diabetes mellitus; MAL, methyl-aminolevulinate; PDL, pulsed dye laser.
The 4 patients were women, aged 21, 22, 31, and 61 years. All had DM; the first 3 had type-1 DM and the last had type-2 DM. All had received at least 2 prior treatments, with minimal or no response. These treatments included topical corticosteroids, topical calcineurin inhibitors, topical calcitriol, pentoxifylline, acetylsalicylic acid, pulsed dye laser, and cryotherapy.
The time from diagnosis to start of PDT was 2, 8, 72, and 120 months, respectively. The first 2 cases were treated with methyl aminolevulinate (MAL; Metvix®, Galderma, Lausanne, Switzerland). Cases 3 and 4 combined MAL and 5-aminolevulinic acid (BF-200 ALA; Ameluz®, Biofrontera, Leverkusen, Germany). The photosensitizing agent was incubated for 3 hours in the case of MAL, and 2 hours and 30 minutes in the case of BF-200 ALA, in accordance with the protocol that we follow in our hospital. The illumination used was red visible light (Aktilite® CL128, Galderma, Lausanne, Switzerland), with a peak wavelength of 630 nm and total energy of 37 J/cm2, for a period of 9 minutes 50 seconds. Anesthesia was not needed in any of the cases owing to the good tolerance of the technique.
Two sessions with an interval of 2 weeks between sessions were initially indicated. The lesions were then re-evaluated, and a new cycle of treatment was indicated if the effect obtained was insufficient. The mean total number of sessions per patients was 11.3 (interval, 6–18). Each of the lesions received an average of 3.2 sessions (interval, 1–5). The fluorescence observed with the Wood light was low intensity.
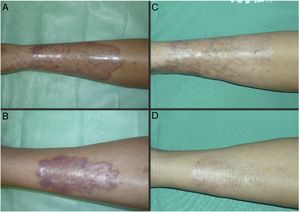
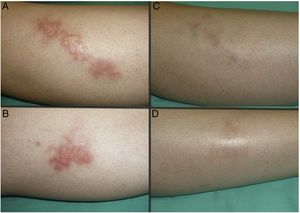
Figs. 1 and 2 show the appearance of the lesions at the start and after treatment. The plaques, with raised violaceous edges, resolved completely; only residual atrophic skin persisted. No signs of active disease were therefore visible after completion of the treatment. Also noteworthy is the rapid improvement of the symptoms after starting treatment. Specifically, the patient in case 1 suffered intense dysesthesia, for which she had been studied in a neurophysiology department. After start of treatment and from the first sessions, the patient presented a considerable improvement in symptoms and became completely asymptomatic.
Subsequently, during follow-up, cases 1, 2, and 3 presented new NL plaques, some of which were distant from the original plaques. Due to the chronic course of the disease, it is difficult to distinguish whether this is persistence or the appearance of new lesions. Nevertheless, the new lesions continue to respond well to treatment with PDT.
DiscussionPhotodynamic therapy is a technique approved for the treatment of actinic keratosis, superficial basal cell carcinoma, and Bowen disease. Its use is increasingly frequent off data sheet in infectious and inflammatory diseases. One of these new indications may be treatment of NL. Its immune-modulating effect, the product of modified cytokine expression (IL1-β, IL-2, and TNF-α) and immune specific response induction, may explain the response of the NL lesions to PDT5,9
In this regard, several articles have been published on single cases satisfactorily treated with conventional PDT.10,11 Nevertheless, the first publications of case series treated with PDT showed more discreet results, such as the study by Berking et al., in which they retrospectively analyzed 18 cases of patients with NL treated with PDT with MAL, and in which they obtained an overall response rate of 39%, with a single case of complete response and more than 60% of nonresponding patients.6
More recently, the Kaae group published a series of 65 patients with NL treated with conventional PDT and natural daylight PDT with MAL. In their article, those authors place particular emphasis on the need to perform prior superficial curettage of the lesions, as this would increase levels of protoporphyrin IX and, thus, increase the efficacy of the PDT. The percentage of complete responses obtained was 66%, with 90% partial responses and with no statistically significant differences between conventional PDT and natural daylight PDT.8 Our results are closer to those of this second study. Nevertheless, we have no experience in prior curettage of the lesions or in the use of natural daylight in the treatment of NL.
With regard to predictive factors of response to PDT in NL, those authors found no statistically significant differences between response and age, sex, duration, and number of lesions. DM was not a predictive factor.8
Due to the chronic course of the disease, the appearance of new lesions during follow-up is frequent. In these cases, new treatment cycles may be indicated. Our impression is that the patients who respond well initially continue to do so with the new sessions. We have not considered maintenance treatment in any of the cases.
In conclusion, we report 4 patients with NL, treated with conventional PDT with a complete response. The latest publications situate PDT as one of the most effective treatments, with response rates of between 39% and 90%.6,8 Long periods of treatment are frequently required to obtain definitive results. Because pain may be a limiting factor, some publications support the use of natural daylight PDT with similar results to those of conventional PDT.8 Due to the low levels of evidence of existing published studies, prospective randomized, controlled prospective studies are required to try to define the real potential of this technique.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bernia E, Llombart B, Bancalari B, Diago A, Serra-Guillén C. Tratamiento de la necrobiosis lipoídica con terapia fotodinámica convencional: serie de 4 casos tratados con éxito. Actas Dermosifiliogr. 2020;111:605–608.