An 8-year-old girl with no relevant personal or family medical history presented with asymptomatic facial lesions that had appeared several months earlier and had not responded to topical corticosteroids. The patient had no history of atopic dermatitis. She was in good general health, with no joint pain, fever, abdominal pain, or weight loss.
Physical ExaminationThe patient presented numerous firm, skin-colored, monomorphous papules distributed in periorificial areas (perioral, perinasal, periocular), accompanied by erythema and desquamation (Fig. 1). Similar lesions were present in the vulvar area (Fig. 2). The physical examination was otherwise completely normal.
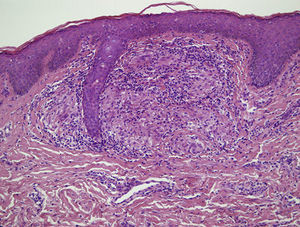
HistopathologyA biopsy of a vulvar lesion revealed a dense lymphohistiocytic perivascular infiltrate in the upper dermis as well as the formation of noncaseating epithelioid granulomas (Fig. 3). The epidermis was spared. Ziehl-Neelsen and periodic acid-Schiff stains were negative. The presence of Demodex folliculorum was not detected in the follicles.
Additional TestsA complete blood count and biochemistry profile revealed no abnormalities. Levels of angiotensin-converting enzyme (ACE) and immunoglobulins were normal. A Mantoux test was negative and a chest radiograph showed no anomalies.
What Is Your Diagnosis?
DiagnosisChildhood granulomatous periorificial dermatitis (CGPD).
Clinical Course and TreatmentTopical corticosteroids were suspended. Treatment with oral erythromycin was started, but little improvement was noted. The patient was switched to oral metronidazole (250mg/d). A striking improvement was noted after 2 weeks and the lesions had resolved completely at 4 weeks.
CommentChildhood granulomatous periorificial dermatitis (CGPD) is a benign, self-limited skin disease that has many characteristics in common with the perioral dermatitis typically seen in middle-aged women. The disease was first described in 1970 by Gianotti,1 who reported a case series of 5 children with monomorphous papules that resembled perioral dermatitis. Other names have been used to describe this entity, including facial Afro-Caribbean cutaneous eruption (FACE), sarcoid-like granulomatous dermatitis, and Gianotti-type perioral dermatitis.2 The term childhood granulomatous periorificial dermatitis, first used by Urbatsch et al.3 in 1989, is currently the most widely accepted term because it most accurately encompasses the characteristics of the entity. CGPD usually affects prepubertal children, and the incidence of the disease may be higher in black patients, although publication bias may account for the difference.
CGPD is characterized by the appearance of lesions in the form of monomorphous skin-colored papules distributed across the periorificial regions of the face, which may be accompanied by erythema and desquamation. Unlike perioral dermatitis, CGPD generally does not manifest with pustules.4 Extrafacial involvement can include the perivulvar region, the neck, the upper trunk, and the limbs. The lesions are usually asymptomatic and tend to resolve without scarring. The etiology of CGPD is unknown, but it appears that topical corticosteroids, especially fluorinated corticosteroids, can trigger or exacerbate the process.2
Histologic findings show a perivascular and perifollicular lymphohistiocytic infiltrate and the formation of epithelioid granulomas that can be either caseating or noncaseating.2,3 The presence of granulomas is not a necessary criterion for diagnosis. The differential diagnosis should include rosacea, acne vulgaris, sarcoidosis, Blau syndrome, lupus miliaris disseminatus faciei, candidiasis, angular cheilitis, atopic dermatitis, demodicidosis, and benign cephalic histiocytosis.2 It is important to ask about constitutional symptoms, joint pain, and respiratory involvement. A laboratory workup including angiotensin-converting enzyme levels and a chest radiograph should be ordered in order to rule out sarcoidosis. In the case of our patient, it was possible to rule out these possible diagnoses on the basis of the medical history and the additional test results.
Treatment options include the suspension of topical corticosteroids and the application of various topical antibiotics, including erythromycin and 0.75% metronidazole, with variable results. In patients with extensive or refractory lesions, systemic treatment with erythromycin or doxycycline is recommended (the latter in children older than 8 years of age).5 A recent case report described the successful treatment of CGPD with oral metronidazole, as in our patient.6
Please cite this article as: Mayor-Ibarguren A. Lesiones periorificiales en una niña. Actas Dermosifiliogr. 2016;107:773–774.