Penile paraffinoma is a skin reaction that develops after the injection of paraffin or mineral oil into the penis in order to increase its size. The condition is relatively common in some eastern European and Asian countries and we believe immigration will cause its frequency in Spain to rise. The procedure is usually performed by nonmedically qualified persons and under poor hygienic conditions. The skin reaction to the exogenous material typically develops months or years after the injection.1
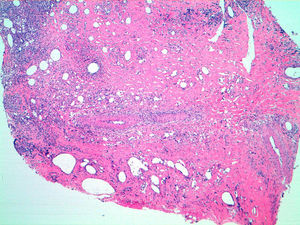
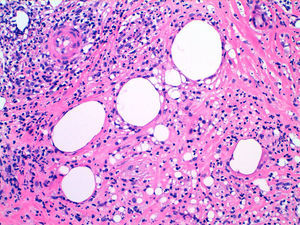
We present the case of a 27-year-old man from Romania who consulted for ulcerated lesions on the penis. Although the patient initially omitted the fact, he later stated that for the previous 4 years until 2 months prior to consultation he had undergone repeated injections of a viscous material into the shaft of the penis in order to increase its size. He also stated that progressively enlarging ulcerated lesions had appeared on the penis and that they had worsened in appearance over the previous months. He had therefore applied the contents of oral antibiotic capsules to the area, but with no improvement. On physical examination there was a marked deformity of the shaft of the penis, which was indurated on palpation, and there were 2 ulcerated lesions with maximum diameters of 3 and 2cm, respectively, located on the lateral surfaces of the penis (Fig. 1). Fistulous tracts were present on the ventral surface, with no visible secretion. The glans was not affected. Histopathology of the larger lesion showed an epithelial ulcer with dermal fibrosis and empty vacuoles, consistent with paraffinoma (Figs. 2 and 3). Staining with periodic acid-Schiff, silver methenamine, and Ziehl-Neelsen was negative. Blood tests were normal and a swab from the ulcers isolated a large number of different colonies, with no predominant microorganism. Culture for fungi was negative. Serology was negative for hepatitis C and human immunodeficiency virus and positive for hepatitis B, herpes simplex virus type 1, herpes simplex virus type 2, and syphilis (VDRL titer 1:2; TPHA, 1:10 240). The patient was diagnosed with penile paraffinoma, and topical therapy was applied with potassium permanganate poultices. The lesions showed some improvement, and the necrotic areas healed. However, after offering the patient surgical reconstruction, he stopped coming to the visits, and we were therefore unable to repeat the serology and we considered the syphilis cured.
Penile paraffinoma is also known as sclerosing lipogranuloma of the penis. The most common etiology of this condition is the injection of highly viscous materials, such as mineral oils, petrolatum, or paraffin, and this is still being performed in eastern Europe, Asia, and Russia.2 The practice was first performed, however, in 1899 by an Austrian surgeon called Robert Gersuny, who injected mineral oils into a child after orchiectomy for genital tuberculosis.1 The motivation for patients to undergo this intervention include a desire to increase the size of the penis, to treat erectile dysfunction, and to satisfy their sexual partners.3
The mean age of affected patients is around 28 years, and symptoms typically develop a year after implantation of the material. Clinical manifestations usually consist of deformity, impotence, erythema, and edema leading to paraphimosis and pain. The main complications are infection, ulceration, necrosis, and the formation of fistulas.4 There have also been reports of migration of the material, with invasion of the corpora cavernosa5 and regional lymphadenitis.6
As stated above, histology shows multiple pseudocystic spaces associated with signs of a foreign body reaction. This response is almost always present, as the human body has no enzymes that metabolize mineral oils.
The differential diagnosis should include infectious diseases, both sexually transmitted and others, and it is usually therefore necessary to biopsy the lesion and take samples for culture and serology. Diseases such as lupus vulgaris and atypical mycobacterial infection secondary to the injection of sterile material must be excluded. Squamous cell carcinoma must be considered in the case of ulcerated lesions with hard serpiginous borders. A history of injection of paraffin into the penis is the key to clinical diagnosis.
First-line treatment consists of early complete surgical excision of the foreign body and of the associated reaction, with closure by first intention when possible.7 Antiseptics and antibiotics will only treat secondary infections of the lesions. Cases with a good response to systemic corticosteroid therapy have been reported.3
Penile paraffinoma is a condition with an increasing incidence in Spain due to the rise in the number of patients from eastern European and Asian countries. As patients usually deny having had these injections, dermatologists and urologists must suspect this diagnosis when examining genital ulcers that do not correlate with other diseases.
Please cite this article as: Gómez-Armayones S, Penín R, Marcoval J. Parafinoma de pene. Actas Dermosifiliogr. 2014;105:957–959