Morphea is a skin-limited scleroderma characterized by sclerosis of variable depth and extent, which can pose a therapeutic challenge.1
We describe a case of morphea associated with neuropathic ulcers that responded to apremilast.
A 57-year-old woman presented to dermatology in March 2018 with a 4-month history of pretibial ulcers that appeared after minimal trauma or hot-water burns, accompanied by decreased sensation in the area. She had undergone gastric bypass in April 2014, after which she lost 44kg and developed protein-calorie malnutrition with vitamin deficiency corrected by nutritional supplements. She also had peripheral psoriatic arthritis since 2016, treated with leflunomide. On examination, there were well-demarcated ulcers on indurated plaques with a shiny, dyschromic surface and absent adnexal structures on the legs (Fig. 1); similar plaques without ulcers were present on the forearms.
On further questioning, she reported that 3 months after surgery she developed edema, erythema, and arthromyalgias in the limbs along with paresthesias and hypoesthesia, which were attributed to nutritional deficiency. No eosinophilia was documented. In 2016, electromyography demonstrated axonal sensorimotor polyneuropathy of the upper and lower limbs. She denied Raynaud phenomenon, finger edema, GI or respiratory symptoms, and had not been on tryptophan supplements. Blood tests – including complete blood count, autoimmunity, and nutritional, iron, and thyroid profiles – were normal.
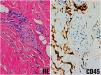
The clinical suspicion was ulcers due to neuropathy overlying morphea plaques. Histologic study of a lesional biopsy showed dermal fibrosis with absence of adnexal structures (Fig. 2), and immunohistochemistry (S100 and CD45) demonstrated a perineural lymphocytic infiltrate without eosinophils (Fig. 3).
With a diagnosis of morphea, leflunomide was switched to methotrexate 10–20mg/week, along with hyperbaric oxygen therapy, micrografts, and courses of antibiotics for ulcer superinfection. Over the next 2 years there was clear, sustained improvement. Although ulcers healed where morphea regressed, the process was very slow, and new ulcers appeared in areas where cutaneous sclerosis persisted. In May 2022, apremilast was added, with progressive improvement from the first month, complete re-epithelialization of the ulcers by 5 months (Fig. 4), resolution of arthromyalgias, remission of morphea with reappearance of adnexal structures, and cessation of neurologic symptoms, with a normal electromyogram in November 2022. Methotrexate was discontinued 3 months into apremilast, and she remained asymptomatic through the last clinical follow-up 18 months after treatment initiation.
Morphea (localized scleroderma) follows a characteristic clinical course, beginning with an inflammatory phase that evolves to scar-like sclerosis; its pathogenesis involves an underlying immune dysfunction with additional genetic and environmental factors, most often without a clear trigger.2
Compared with systemic sclerosis, morphea is not associated with sclerodactyly, Raynaud phenomenon, capillary abnormalities, or internal organ involvement; extracutaneous symptoms are therefore uncommon, occurring more often when skin disease is extensive or deep and typically being articular.1,3 Neurologic involvement is uncommon and is seen mainly in pediatric patients, almost exclusively in linear morphea of the head.4
The peripheral neuropathy observed in our patient is not described in standard dermatology texts as a clinical feature of this disease. Histologically, however, perineural lymphoplasmacytic inflammation has been observed in more than half of morphea biopsies studied, increasing to 84% when immunohistochemistry is used. Although the infiltrate is preferentially perineural, about 5% of samples show additional intraneural inflammation. Unlike our patient, most reported cases are asymptomatic.5 Even so, this histologic finding has proved useful as a tool in the differential diagnosis favoring morphea over other inflammatory skin diseases.6
For treatment, the most widely used drugs are methotrexate and corticosteroids. Other systemic therapies have been used for refractory cases – including mycophenolate, bosentan, infliximab, tofacitinib, and abatacept – but there are insufficient data to support their routine use.1
Phosphodiesterase-4 inhibition has shown the ability to prevent and reverse a profibrotic cytokine milieu in preclinical models of dermal fibrosis.7 In a recently published 5-case series of morphea, apremilast was used as bailout therapy with a favorable response; in one case, similar to ours, there was improvement in previously unexplained hand arthralgias.8
In conclusion, apremilast – given its activity in cutaneous fibrosis and the clinical response in this case and others in the literature – may be an alternative for complicated morphea or in patients with intolerance or lack of response to other agents.
Conflicts of interestNone declared.