Papuloerythroderma of Ofuji is a chronic pruritic dermatosis characterized by a generalized rash consisting of coalescing erythematous papules that spare the skinfolds (deck-chair sign).1 Its pathogenesis is unclear: while idiopathic cases have been documented, this condition also occurs as a reaction to other dermatoses2 or to solid or hematologic malignancies.3
We describe the case of a 62-year-old man with a history of hypertension, dyslipidemia, and iliofemoral deep vein thrombosis who was being treated with enalapril, simvastatin, and clopidogrel. He was allergic to penicillin, sulfonamides, and imipenem.
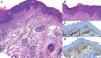
The patient was being treated at our hospital's internal medicine department for a highly pruritic erythroderma that had appeared 1 year earlier. He had been treated with systemic and topical corticosteroids resulting in partial remission and frequent exacerbations that required hospitalization. The patient consulted our outpatient clinic for a widespread, papular, erythematous rash that spared the cervical, mammary, abdominal, antecubital and popliteal skinfolds (Figure 1A). No mucosal or palmoplantar lesions were detected, and the patient showed no signs of lymph node swelling or organomegaly. Laboratory tests revealed a lymphocyte count of 9900/μL with 9% eosinophils; creatinine, 1.4mg/dL; urea, 82mg/dL; total immunoglobulin (Ig) E, 404IU/mL; and β2-microglobulin, 8.3mg/dL. Protein electrophoresis revealed a monoclonal IgG κ band. The remaining tests, which included infectious serology and antinuclear antibodies, complement system, tumor markers, and urine sediment, as well as imaging studies (chest radiograph, skeletal series, and abdominal ultrasound), were normal. Bone marrow histomorphology was also normal. Skin biopsy showed a pattern of subacute spongiotic dermatitis (Figure 1B).
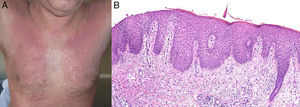
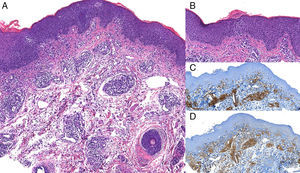
Based on the clinical and histological data and the laboratory abnormalities, the patient was diagnosed with papuloerythroderma of Ofuji associated with monoclonal gammopathy of undetermined significance (MGUS). We began treatment with narrowband UV-B phototherapy (3 sessions per week), topical 0.1% mometasone furoate cream, and oral hydroxyzine (10mg/day), and withdrew the patient's oral corticosteroid treatment. One month after the complete cessation of oral corticosteroids the patient experienced a flare-up of well-circumscribed, brownish, erythematous nodules and tumors on the trunk and extremities (Figure 2). A skin biopsy of one of the new lesions showed a nodular lymphoid infiltrate composed of small and medium-sized cells with cerebriform nuclei. The infiltrate was slightly epidermotropic with isolated foci of exocytosis; some lymphocytes were aligned along the basement membrane (Figure 3, A and B). These lymphocytes were CD3+, CD4+ (Figure 3, C and D), and CD8–, with a polyclonal profile for T-cell receptor γ. Physical examination revealed no lymph node swelling or organomegaly. Peripheral Sézary cell count was normal. The patient was negative for human T-cell lymphotrophic virus types I and II. Based on the diagnosis of papuloerythroderma of Ofuji as a manifestation of cutaneous T-cell lymphoma (CTCL) and MGUS, a new therapeutic approach was proposed. The patient received 3 weekly sessions of psoralen-UVA (PUVA) therapy, 150mg of bexarotene daily, and 3MU of interferon alfa 3 times per week for 1 year, until complete remission was achieved. We subsequently prescribed a maintenance regimen of 1 weekly session of PUVA and 1MU of interferon alfa per week for another year. The patient's CTCL, papuloerythroderma, and MGUS remain in complete remission after 3 years.
A, Image shows a superficial diffuse infiltrate and a nodular infiltrate located predominantly in the papillary and reticular dermis beneath an orthokeratotic epidermis with moderate acanthosis; hematoxylin-eosin, original magnification ×4. B, Image shows thickened dermal collagen and a predominantly lymphocytic infiltrate showing some epidermotropism; hematoxylin-eosin, original magnification ×20. C, CD3+, original magnification ×2: intense staining of lymphocytic infiltrate. D, CD4+, original magnification ×2: most lymphocytes are stained with this immunohistochemical marker.
Since 1984, when Ofuji described a new entity characterized by a cutaneous pruritic rash that spares the skinfolds and is associated with increased IgE levels and peripheral eosinophilia and lymphopenia,1 the pathogenesis of this condition has remained the subject of debate.4 The most widely accepted hypothesis is that papuloerythroderma of Ofuji is a reactive dermatosis: it has been described in association with contact dermatitis, drug hypersensitivity reactions, gastric and lung carcinomas, hematological malignancies, and immunosuppression.5
Papuloerythroderma of Ofuji may be a prelymphomatous manifestation of CTCL. Seventeen cases have been described in the literature, of which eleven showed histological changes compatible with CTCL at the time of diagnosis.4 As in our case, those patients tended to show changes in the morphology of the lesions, with loss of the deck-chair sign.6 It has been proposed that these papuloerythrodermas with histological features of CTCL be classified as papuloerythroderma-like CTCL.4 The literature also describes one case of papuloerythroderma associated with MGUS7 and another associated with myeloma.8
In the case of our patient all 3 of the above entities coincided. Given the simultaneous resolution of both the MGUS and the T-cell lymphoma, it would be interesting to know whether a common immunological alteration underlies both these conditions. The papuloerythroderma seen in our patient may have been a prelymphomatous reactive dermatosis9 or alternatively, from its outset, a papuloerythroderma-like CTCL, which was masked by successive treatments with oral and topical steroids. We are inclined to favor the latter hypothesis.
The association described in the present case, papuloerythroderma of Ofuji associated with CTCL and MGUS, has not been described in the literature, and underscores the diagnostic difficulties posed by reactive dermatoses and cutaneous prelymphomatous T-cell skin dyscrasias. Correct diagnosis of these types of cases will be facilitated by close clinical follow-up and repeated skin biopsies upon observation of the slightest change in the lesions.5,6,9,10
Please cite this article as: Otero-Rivas M, Sánchez-Sambucety P, González-Morán A, Rodríguez-Prieto M. Papuloeritrodermia de Ofuji asociada a linfoma cutáneo de células T Cd3+, Cd4+, Cd8-y gammapatía monoclonal de significado incierto. Actas Dermosifiliogr. 2015;106:435–437.