Pachydermodactyly, from the Greek pachy (thick), dermos (skin), and dactylos (digits), is a very rare form of acquired benign digital fibromatosis. It is characterized clinically swelling of the medial and lateral aspects of the proximal interphalangeal joints of practically all the fingers of the hands (with the exception of the thumb). We describe a clinically striking new case that responded satisfactorily to corticosteroid infiltration and we discuss the different therapeutic options available.
A 15-year-old patient with no past medical history of interest was referred to dermatology outpatients for evaluation of thickening of the second, third, and fourth fingers of both hands that had started to develop 2 years earlier. An additional finding was that the patient attended a gymnasium 4 days a week to perform weight training.
Physical examination revealed very marked, diffuse thickening at the level of the proximal interphalangeal joints of all the fingers of the hands, except the thumbs and fifth fingers. Movement was not limited (Fig. 1) and there were no others skin changes.
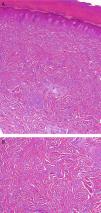
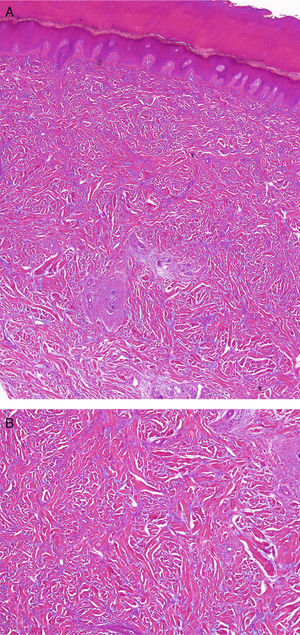
Histology of a skin biopsy taken from the lateral aspect of the second finger of the right hand showed thickening of the dermis with an increase both in collagen fibers and, to a lesser extent, in fibroblasts (Fig. 2, A and B). Few changes were detected in the epidermis, though minimal hyperkeratosis with compact orthokeratosis was observed.
A, Histology image in which thickening of the dermis may be observed, associated with an increase of both collagen fibers and, to a lesser extent, fibroblasts (hematoxylin-eosin, original magnification x10). B, Histology image at higher magnification showing the increase of the collagen fibers and fibroblasts (hematoxylin-eosin, original magnification x20).
A full laboratory work-up, including renal and liver function and markers of autoimmunity, was completely normal. X-rays of the hands showed no bone or joint abnormalities, and magnetic resonance revealed thickening of the dermis that extended down to the subcutaneous cellular tissue.
It was decided to treat the patient with corticosteroid injections into the affected area. We used a solution of triamcinolone acetonide, 40 mg/mL, mixed with an equal volume of 2% mepivacaine solution, and performed injections (2-3mL of the solution into each thickened area) in 2 sessions, 2 months apart. This achieved a marked decrease in the size and firmness of the lesions after the 2 sessions (Fig. 3).
Pachydermodactyly is a rare condition, with only 80 published cases to date.1 It is included in the group of the fibromatoses and since it was first described by Bazex et al.2 in 1973 it has been referred to by various names, including knuckle pads, pseudo-knuckle pads, heloderma, and subcutaneous fibroma.
Our patient presented a model case with regard to age and sex, as pachydermodactyly is usually seen in young patients (mean age at presentation, 21.2 years), although the age range of published cases is from 5 to 69 years, and the condition is more common in men, with a male to female ratio of 3 to 2.3 This predominance in men has been related to the possible etiology and pathogenesis of the disorder as, although this is not yet fully understood, it has been suggested that pachydermodactyly may be a reactive disorder secondary to repeated minor exogenous trauma.4 This proposal is based on the finding that pachydermodactyly shows a relationship with numerous occupations and activities such as martial arts and climbing,5 work in food-processing factories,3 patients with obsessive compulsive disorders associated with tics affecting the hands,6 or weight lifting, as in the case we present.
Our case is also highly illustrative of the clinical manifestations, as the typical findings are asymptomatic and symmetrical swelling of the sides of the fingers. The second, third, and fourth fingers are most commonly affected, but the fifth finger and even the dorsum of the hand can occasionally be affected.1 There are usually no epidermal changes, though mild erythema, fine desquamation, or lichenification may sometimes be observed.1,7 Hand movements are not affected.
The diagnosis is clinical. The most typical findings on histology are a thickening of the dermis, which may be accompanied by a benign proliferation of fibroblasts, and an increase in collagen fibers that extends down to the subcutaneous cellular tissue. Hyperkeratosis (ortokeratosis or parakeratosis) may also be observed, as well as a decrease in the elastic fibers and mucin.1 Plain x-rays are normal and magnetic resonance shows an increase in soft tissue volume around the joints.
The main differential diagnosis is with knuckle pads. These nodules, which can be idiopathic (true) or due to recurrent trauma (pseudo-knuckle pads), are differentiated from pachydermodactyly by the site of the lesions; in pachydermodactyly the lesions typically affect the sides of the fingers whereas knuckle pads are found on the dorsal surface. In addition, they are usually more circumscribed lesions.8
Another disease that we must consider is juvenile hyaline fibromatosis. This disease, due to a genetic abnormality that alters the regulation of collagen synthesis, leads to the appearance of multiple subcutaneous nodules on the fingers. However, it also causes other changes, such as bone lesions, ulceration, gingival hypertrophy, and tumors on the scalp and nose.1
Certain types of polyarthritis that affect the proximal interphalangeal joints, such as psoriatic arthritis and rheumatoid arthritis, must also be considered in the differential diagnosis. The diagnosis of these dermatoses is facilitated by the clear presence of inflammatory signs.8
Published reports on pachydermodactyly focus little on its treatment. Some authors even advocate therapeutic abstention, suggesting only that patients stop performing the activities that gave rise to the exogenous trauma. This approach comes from the fact that pachydermodactyly is a benign dermatosis that interferes little with movement. However, in our opinion, the disease can have a significant impact on the quality of life of some patients, and therapy should not therefore be ignored. At the present time, the 2 treatment options considered are local corticosteroid infiltration and surgical treatment by resection of the fibrous tissue.1 Descriptions on how to perform these procedures (the surgical technique or the dose and regimen of corticosteroid infiltration) are scarce.
In our patient we used a solution of triamcinolone acetonide, 40 mg/mL, mixed with an equal volume of 2% mepivacaine solution, and we performed injections in 2 sessions, 2 months apart. At each session we injected a total of 2-3mL of the solution into each thickened area. The cosmetic result was acceptable, and there was mild periarticular hypopigmentation. Thus, with the caution that comes from a report of a single case, we propose this therapeutic regimen as one of the treatment options in similar cases.
Please cite this article as: Plana Pla A, Bassas Vila J, Toro Montecinos M, Ferrandiz Foraster C. Paquidermodactilia tratada con éxito con infiltraciones de triamcinolona. Actas Dermosifiliogr. 2014 105:319–321.