Pachydermodactyly is a rare, benign form of acquired digital fibromatosis that mainly affects male adolescents without a family history.1 It is characterized by asymptomatic bilateral symmetric swelling of the lateral aspects of the proximal interphalangeal (PIP) joints of the second, third, fourth, and occasionally fifth fingers.1,2 Although diagnosis is essentially clinical, skin biopsy shows compact orthokeratotic hyperkeratosis, increased numbers of collagen fibers and fibroblasts, and no inflammatory changes.1 Blood and imaging tests are normal.3
We report the case of a 19-year-old man with no past personal or family history of interest who presented with asymptomatic swelling of the PIP joints. The swelling had appeared 2 to 3 years earlier and had initially affected the lateral surfaces of the joints of the fifth finger of the left hand. Similar changes gradually appeared on the PIP joints of the second, third, fourth, and fifth fingers of both hands (Fig. 1). During the interview, the patient reported that he often interlocked the fingers of his hands. The physical examination revealed multiple tics involving the face, the trunk, and both arms. The blood results were normal and tests for antinuclear antibodies and rheumatoid factor were negative. Radiography of both hands and nuclear magnetic resonance imaging showed thickening of the soft tissues around the PIP joints on the second through fifth fingers of both hands, with no evidence of bone or joint abnormalities. The only abnormal finding in the bone scan was dorsolumbar scoliosis, with asymmetry in the right coxofemoral joint in relation to the scoliosis. Skin biopsy showed nonspecific lesions that nonetheless were compatible with pachydermodactyly (Fig. 2). We requested psychiatric evaluation and the patient was diagnosed with generalized anxiety disorder associated with tics. Anxiety disorder group therapy at the psychiatry department was recommended. The patient's skin lesions have remained stable to date.
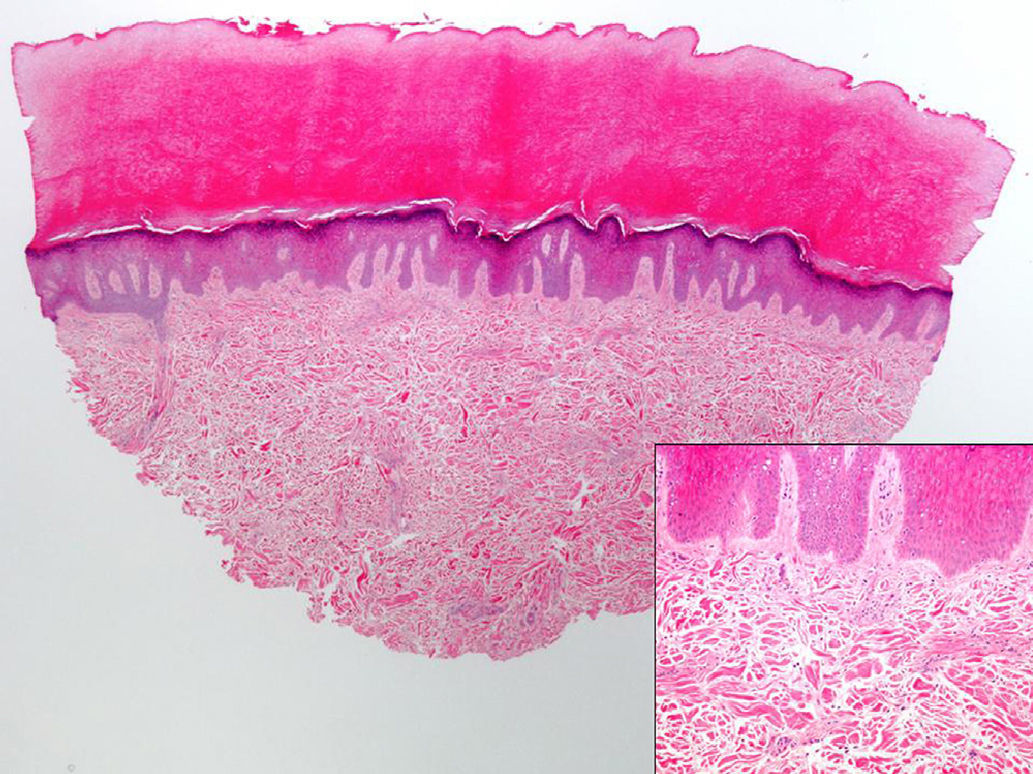
Histological examination showed a thickened dermis with thickened collagen bundles and increased numbers of fibroblasts, without inflammation. The epidermis showed orthokeratotic hyperkeratosis (hematoxylin-eosin, original magnification ×5). The inset on the right shows the collagen bundles and fibroblasts at higher magnification (hematoxylin-eosin original magnification ×20).
The etiology of pachydermodactyly is unknown, although several authors have suggested that the disorder could be caused by repetitive minor trauma involving the repeated rubbing of fingers during continuous interlocking movements.2,4 This would explain why pachydermodactyly does not affect thumbs and involves fifth fingers less frequently.3 We saw our patient repeatedly interlocking his fingers during consultation and his mother confirmed that he had being doing this for years. Minor traumas of this nature have been associated with activities such as climbing,1 occupational exposure (poultry processing),5 and underlying psychiatric disorders. There have been reports of pachydermodactyly associated with serious psychiatric disorders, such as obsessive-compulsive disorder, related disorders such as Asperger syndrome or tic disorders, and behavior disorders, such as anxiety disorders.2,3,6 Our patient was diagnosed with generalized anxiety disorder associated with tics. He did not fulfil the diagnostic criteria for obsessive-compulsive disorder or Asperger syndrome.
Pachydermodactyly is probably more common than believed and is likely to be underdiagnosed because it is asymptomatic and does not interfere with joint movement. Effective medical interventions do not exist for pachydermodactyly, but triamcinolone hexacetonide injections7 and surgical resection of subcutaneous fibrotic tissue have produced good cosmetic results in some cases.1,3
Rapid clinical diagnosis is important as it will reassure patients and avoid unnecessary tests and studies and inappropriate treatment.
While the association between pachydermodactyly and psychiatric morbidity is uncommon, given its importance, we believe that all patients diagnosed with pachydermodactyly should be evaluated by a psychiatrist, and particularly those who repeatedly interlock or rub their hands, causing finger friction. These patients would benefit from adequate psychological and/or psychiatric treatment, and partial remission of pachydermodactyly lesions has been reported following the elimination of the causes of repetitive minor trauma.
Please cite this article as: Carrascosa R, Godoy A, Gordillo C, de Argila D. Paquidermodactilia en un paciente con trastorno de ansiedad generalizada asociado a tics. Actas Dermosifiliogr. 2014;105:625–626.