Olmsted syndrome is a rare disorder of keratinization characterized by bilateral mutilating palmoplantar keratoderma (PPK) with keratotic plaques around mouth, nose and anus, often associated with flexion deformity of digits and nail abnormalities.1 Herein, we describe a case of Olmsted syndrome in a girl with pityriasis amiantacea-like thick plaques over the scalp and follicular hyperkeratosis of legs.
A 10-year-old female presented with well-defined symmetrical hyperkeratotic plaques over palm and sole which started developing from the age of 2 months. The lesions were painful and she was unable to walk properly without shoes. She was born of normal vaginal delivery with no history of consanguineous parents. There was no history of similar complaints in the family including two siblings. She achieved normal developmental milestones. Examination revealed an active girl with normal intelligence and physical parameters. Systemic examination revealed no abnormalities. Cutaneous examination revealed thick hyperkeratotic plaques on palm and soles forming “keratotic sandals” (Fig. 1(a)). Perifollicular hyperkeratotic papules were present over the bilateral lower limbs (Fig. 1(b)). Warty hyperkeratotic plaques were present in gluteal cleft (Fig. 1(c)). but the perioral area was spared. There was flexion deformity of MCP joint of the right hand for last 5 years, onychogryphosis present in the first three toenails of both feet. Onychodystrophy of nails of both the hand was present. Hairs over the scalp, eyebrows and eyelashes were thin and sparse for last 4 years. Hyperkeratotic plaques were present over the scalp which were more pronounced over the occiput (Fig. 1(d)). Oral, genital, ocular mucosa, teeth and joint were normal.
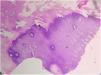
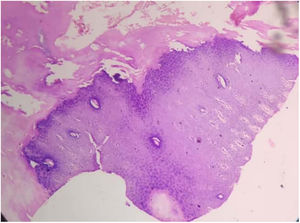
Routine laboratory test and serum zinc level were normal. The X-ray of hands showed flexion deformity of right hand. Histopathological examination showed massive hyperkeratosis, parakeratosis, hypergranulosis and acanthosis (Fig. 2). The patient was prescribed capsule acitretin (0.5mg/kg/day) along with topical urea and salicylic acid. There was partial improvement after 8 weeks (Fig. 3) but the patient was lost to follow up.
Olmsted first described this disease in a 5-year-old male child who had bilateral symmetrical sharply marginated palmoplantar keratoderma and periorificial hyperkeratotic plaque since one year of age. Most cases are sporadic although autosomal dominant, autosomal recessive and X linked forms are also found. Gain of function mutation in TRPV-3 (transient receptor potential vanilloid-3) on chromosome 17 is most common in Olmsted syndrome patient which leads to elevated keratinocyte apoptosis.1 Mutation in MBTPS-2 gene encoding a zinc metalloprotease has been reported in recessive and X linked form of disease. Immune studies have shown basal and suprabasal keratiocyte proliferation with reactivity for K67 marker.2 Males are mostly more commonly than females.3
The disease usually begins when the child starts to walk and grasp objects. Palmoplantar keratoderma is of transgradiens type and is severely disabling. Keratotic papules develop over the periorificial areas and may extend to the flexures. Fissuring of the toes occurs leading to autoamputation of the digits and skin thickening may lead to flexion deformities.4 Our patient had mutilating keratoderma, periorificial papules and flexion deformity. However, there was no pseudoainhum formation. Additionally, she had follicular keratotic papules all over her legs.
Olmsted syndrome patients present with hair abnormalities like alopecia, sparse, thin, woolly and curly hair and madarosis.5 Our patient had diffuse hair loss with sparse, thin and brown hair. Additionally, she had thick dry heaped up pityriasis amiantacea like picture over the scalp. Nail may be dystrophic, lustreless, ridged and rough nail, onychogryphosis, onycholysis, subungual hyperkeratosis and even absence of nails are seen in these patients.5 Short stature in Olmsted syndrome may be due to delayed physical development. Other features include oral leukokeratosis, palmoplantar hyperhidrosis, hypohidrosis, corneal opacities, dental anomalies and hyperkeratotic streaks in skin flexures. Squamous cell carcinoma and malignant melanoma of palmoplantar lesions has been described.6
The presence of periorificial keratotic plaques in a patient with palmoplantar keratoderma is diagnostic of Olmsted syndrome and helps exclude other causes of palmoplantar keratoderma such as Mal de Maleda, pachyonychia congenita and Vohwinkel syndrome. Mutation of KDSR gene, which encodes the enzyme 3-ketodihydrosphingosine reductase, involved in ceramide synthesis, can also present with features similar to Olmsted syndrome. However, such patients have milder palmoplantar keratoderma with prominent erythema and well demarcated scaly plaques over face and genitals.7
Treatment of Olmsted syndrome is difficult, the keratoderma may be controlled by regular pairing, keratolytic agents (salicylic acid, urea, boric acid, shale oil), emollients and oral retinoids.8 Wet dressing and prolonged socking of the affected part in water have been tried with varying success. Systemic treatment with antihistaminic, vitamin E and vit A, antimicrobial, corticosteroids have been tried with not much benefit. Our patient got partial relief with acitretin (0.5mg/kg/day) along with topical keratolytic (20% urea) and emollient. For non-responsive patients, surgical removal followed by skin grafting can be tried. Erlotinib, an epidermal growth factor inhibitor has been described to relieve the hyperkeratosis and pain in three patients in a recent report.9
Less than 80 cases of Olmsted syndrome have been reported in literature. Our patient was unique as she had thick scales over the scalp and keratotic papules over legs apart from the usual manifestations of Olmsted syndrome such as mutilating palmoplantar keratoderma, flexion deformity and hyperkeratosis in the gluteal cleft.
Conflict of interestThe authors declare that they have no conflict of interest.