This is the case of a 72-year-old man, with no significant past medical history who presented to the health center with a 5-year history progressively growing lesion on his ear right helix. He did not complain of associated pain, itching, spontaneous bleeding, or sustained any traumas to the region of interest.
Physical examinationThe physical examination revealed the presence of a 1.5cm nodular excreting lesion with skin-colored appearance, well-demarcated borders, firm consistency, mobile, non-infiltrated, and non-painful upon palpation in the upper third of the right helix (fig. 1). The dermatoscopy did not reveal any characteristic structures and was entirely non-specific.
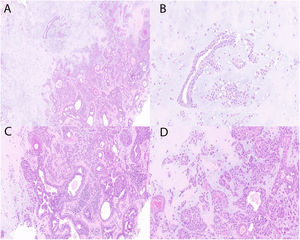
HistopathologyThe punch biopsy performed confirmed the presence of a well-demarcated tumor located in the dermis with a dual component, epithelial, and stromal. Cuboidal cells were seen arranged in cords, along with tubulo-alveolar structures surrounded by stroma exhibiting chondroid differentiation (fig. 2).
What is your diagnosis?
DiagnosisChondroid syringoma.
Disease progression and treatmentAfter achieving the final diagnosis of chondroid syringoma, surgical excision was performed with satisfactory cosmetic results.
CommentChondroid syringoma, also known as cutaneous mixed tumor, is a rare benign adnexal tumor originating from the sweat glands, with an estimated incidence ranging from 0.098% to 0.01%.1 Back in 1859, Billroth described a salivary gland tumor with similar morphological characteristics for the first time. A century later, in 1961, Hirsch and Helwig first introduced the term chondroid syringoma.1 The etiology and risk factors of chondroid syringoma are still unknown. Clinically, it presents as a slowly growing subcutaneous tumor nodule, covered by normal-looking or slightly erythematous skin that often presents as a solitary lesion. Chondroid syringoma is often asymptomatic, has a firm consistency, and is typically 0.5cm to 3cm in size. Lesions >3cm are considered giant and have a relatively high likelihood of being malignant. Chondroid syringomas often occur between the ages of 20 and 60 and are more common in men than women, with a ratio of 2:1.1,2 It is very rare in children and was first described in kids back in 2007.3 The most common locations are the nose, cheeks, upper lip, scalp, forehead, chin, eyelids, ears, and neck. It is less common in the trunk, limbs, and genitals. The clinical presentation is nonspecific, which is tremendously challenging for dermatologists.1,2 The differential diagnosis of chondroid syringomas includes epidermal cysts, neurofibromas, dermatofibromas, pilomatrixomas, trichoepitheliomas, histiocytomas, and basal cell carcinomas.1,2 The confirmatory diagnosis is histopathological reporting the presence of a dual component, one epithelial—with cells arranged in cords or tubulo-alveolar structures—and the other one stromal with fibrous, myxoid, and/or chondroid features.1,2,4 Islands of squamous cells, keratin cysts, calcification foci, ossification foci, and even adipose metaplasia can sometimes be found. Chondroid syringomas can be categorized into eccrine or apocrine based on the epithelial component. The former consists of small luminal spaces coated by a single layer of cuboidal epithelial cells, while the latter consists of tubulo-alveolar structures coated by a double layer of cuboidal epithelial cells, with the outer layer being flatter and of myoepithelial origin.1,2 Typical findings of malignancy include cellular atypia, more mitoses, neural and vascular invasion, infiltration of underlying tissues, and the presence of necrosis.5,6 The treatment of choice is complete surgical excision, after which recurrence is exceptionally rare. Other therapeutic options include electrocoagulation, dermabrasion, or vaporization with argon laser or CO2 laser.4 Malignant chondroid syringoma is extremely rare, more common in women, and tends to occur on the extremities and trunk. It has the potential for local and distant spread, being the lymph nodes, lungs, and bones common sites for metastasis.5,6