The patient was an 82-year-old man with a history of ischemic heart disease, aortic valve replacement for severe stenosis, gastrointestinal hemorrhage, benign prostatic hypertrophy, and insertion of a pacemaker.
He had undergone excision of several basal cell carcinomas from the nose and dorsum of the left hand, in addition to one situated in the right nasolabial fold that had been excised some years earlier. He also had a history of actinic cheilitis and Bowen disease on the right forearm.
On this occasion he was seen in outpatients for a pruritic plaque that had arisen in right nasolabial fold 4 months earlier and showed rapid growth.
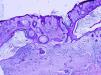
Physical ExaminationOn examination there was a well-defined erythematous plaque measuring 2.9×1.5cm. The plaque was formed of confluent yellowish papules and nodules that gave it a lumpy appearance. The border of the plaque was in contact with the scar of a previous operation (Fig. 1).
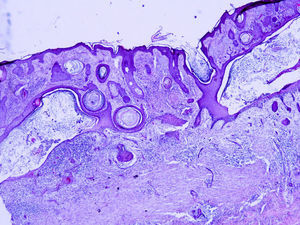
HistopathologyOn histopathology, the epidermis showed mild acanthosis with orthokeratotic hyperkeratosis and marked solar elastosis. Large, fine-walled cystic structures that contained multilayered basophilic keratin were observed in the papillary and superficial reticular dermis. The few sebaceous glands remaining were hypoplastic. The scar of the previous operation was visible beneath the cysts. Some areas of irregular epithelial cords were present between the cyst and the scar, but there was no atypia and the cords were considered to be reactive (Fig. 2).
What is Your Diagnosis?
DiagnosisActinic comedonal plaque.
Clinical CourseThe patient died of unrelated causes soon after consultation.
CommentIn 1980, Eastern and Martin1 described 5 patients under the heading actinic comedonal plaques. A further 3 isolated cases have been reported since that time.2–4 In 2003, Morgan et al.5used the term multiple follicular cysts, infundibular type with vellus hair and solar elastosis of the ears to describe 3 cases of unilateral plaques on the auricle of the ear that, in our opinion, satisfied the criteria for actinic comedonal plaques.
The majority of cases occur in men of advanced age, with marked solar damage and a history of nonmelanoma skin cancer or actinic keratosis. All cases presented single plaques with nodules or cysts and dilated follicular orifices, with a bluish, yellowish, or erythematous color, probably depending on the predominant type of lesion. The upper limbs are the most common site, though lesions have also been reported on the face and on the ear. Histopathology shows marked solar elastosis, with a thin or acanthotic epidermis, and occasionally there is moderate dyskeratosis. Comedones and follicular dilatation are observed in all cases, with a reduced number of sebaceous glands, while the eccrine glands are unaffected. In 1 case, the lesions appeared to be epithelial invaginations, as also observed in our case.
The actinic comedonal plaque is considered to be a localized variant of Favre-Racouchot syndrome because of its clinical and histopathological similarity. However, the lesions in Favre-Racouchot syndrome are bilateral and localized in the periorbital areas and the temples.
The lesion must be distinguished clinically and histopathologically from comedonal nevus. However, comedonal nevus is usually present at birth or appears during childhood, and often presents a linear distribution. From a histopathological point of view, the lesions must also be differentiated from the residual phase of coral reef granuloma and from chronic Staphylococcus aureus infection,6 though there is typically a history of infection in the area. Although dyskeratosis is occasionally observed in actinic comedonal plaque, differentiation from actinic keratosis is rarely a problem. An important factor in our case was the clinical similarity of the lesion with basal cell carcinoma, which was the provisional clinical diagnosis.
Treatment by surgery or with topical corticosteroids2 or vitamin A derivatives3 has been unsuccessful. Tetracyclines only improved the inflammatory appearance of the lesions.3 Resolution has been reported in some cases after cryotherapy.2
Please cite this article as: Piqué-Duran E, García-Vázquez O, Tang K. Placa abollonada en surco nasogeniano. Actas Dermosifiliogr. 2015;106:63–64.