Since the outbreak of the COVID-19 pandemic, few cases of psoriasis flares associated to SARS-CoV-2 infection have been reported, most of them in patients with previous history of the disease.1 Drugs used against COVID-19, interruption of active treatments and the viral infection itself have been put forward as possible factors contributing to this phenomenon.1,2 Moreover, episodes of many other autoimmune and autoinflammatory diseases have been related to SARS-CoV-2 infection.3
In September 2020, a 71-year-old man presented with diarrhoea and generalized weakness over the previous week, without other symptoms.
His body temperature was 35.8°C. Basal oxygen saturation was 96%. Blood test was unremarkable except for C reactive protein (CRP) (12.45mg/dl), D-dimer (1882.0ng/ml), LDH (306.0U/L) and ferritin (976.0ng/ml). Chest X-ray revealed bilateral and peripheral areas of consolidation compatible with COVID-19. A polymerase chain reaction study on nasopharyngeal swab was positive for SARS-CoV-2.
He was given methylprednisolone boli and support measures. During the first days of admission, inflammatory markers gradually descended to normal. Due to diarrhoea, stool culture was performed, which came out negative. Faecal antigens of rotavirus, adenovirus nor astravirus were not detected.
During admission, weakness progressed to tetraparesis, with inability for limb movement against resistance. A lumbar puncture was carried out and cerebrospinal fluid came back negative for HSV 1 and 2, VZV, EBV, enterovirus and cytomegalovirus. He was diagnosed with Guillain-Barré syndrome (GBS), treated with intravenous immunoglobulin and recovered without sequelae.
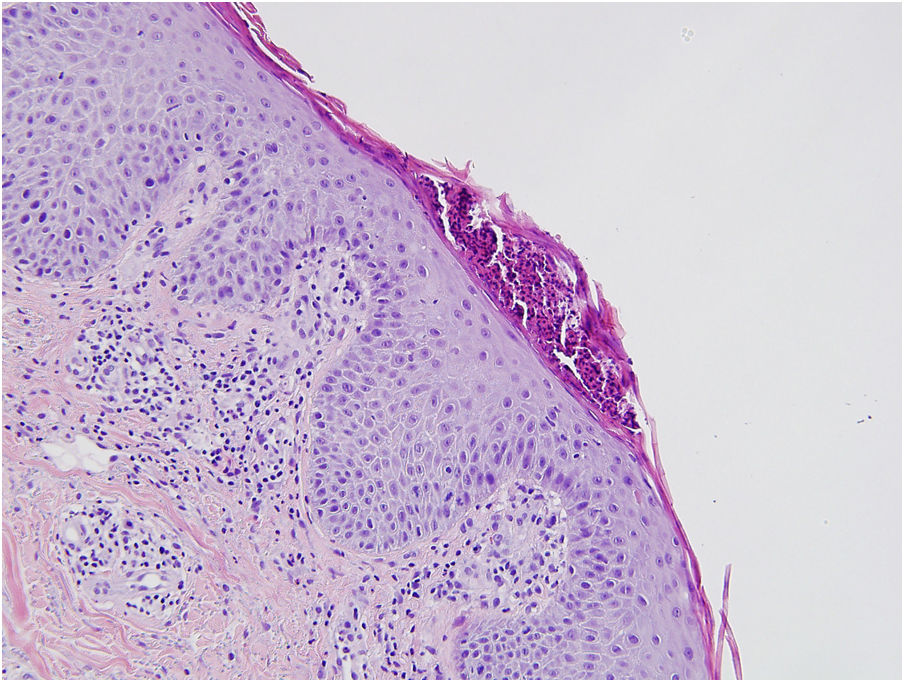
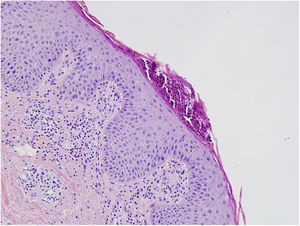
One month later, he was readmitted due to generalized erythema and slight desquamation involving the whole body surface, including facial and acral areas (Fig. 1). Nails and mucosae were unaltered. Conspicuous plantar hyperkeratosis was noted. He was hemodynamically stable and apyretic, but presented shivers. He stated that the lesions had appeared during his first admission as discreet erythematous maculae, which steadily progressed. There was no personal or family of dermatosis, and he denied having started any new medication over the previous months. Blood cell count revealed moderate leucocytosis (12350 WBC/ml). CRP was 8.054mg/dl, and ferritin 37ng/ml. A blood smear showed no abnormalities. Serologies for hepatitis B and C virus, HIV and Treponema pallidum were negative.
A skin biopsy was performed, whose results allowed the diagnosis of psoriasis to be made (Fig. 2).
Treatment with 200mg of cyclosporin twice daily was started (5mg/kg/day), with a favourable response, and tapered over the next seven weeks. However, after cessation of cyclosporin, some involvement persisted as erythrosquamous plaques, Beau lines and nail pitting.
Much attention has been paid to how immunosuppressive treatment of psoriasis could increase the risk and severity of SARS-CoV-2 infection. However, the effects of the infection itself on the course of skin disease have been less thoroughly discussed.
There are few reports of flares, both vulgar and pustular, related to COVID-19 in patients with previously known psoriasis,1,2,4 as well as psoriatic spondyloarthritis onset concomitant with COVID-19.3 Only one case of new onset psoriasis after COVID-19 has been described in a 62-year-old woman with pustules and a family history of the disease.1 We present a case of psoriatic erythroderma reactive to COVID-19 in a patient with no known personal or family history of dermatoses.
Exacerbation of psoriasis in this context has been attributed to different factors. Firstly, the use of hydroxychloroquine, known to disrupt the balance of the epidermal barrier through its inhibition of cholesterol metabolism and epidermal transglutaminase.4 Secondly, the interruption of psoriasis treatments to avoid complications of the infection.1 Thirdly, the administration and subsequent tapering of corticosteroids in the management of COVID-19.1,2
Nonetheless, the aforementioned factors have not necessarily been present in every reported patient.1,4 It is possible that these factors participate in the pathogenesis of this phenomenon in individual cases in which they are present, but SARS-CoV-2 infection itself also seems to be an important inductor on its own. The virus is thought to trigger many autoimmune and autoinflammatory processes, such as macrophage-activation syndrome, vasculopathies, several forms of arthritis (viral, reactive, rheumatoid, etc.) and demyelinating diseases.3 The coincidence of the development of both GBS and psoriatic erythroderma in a same patient shortly after COVID-19 provides an example of this.
The exact mechanism through which SARS-CoV-2 induces psoriasis is unknown. The massive production of cytokines in response to the infection (so-called cytokine storm) creates an inflammatory milieu which favours the genesis of this disease.3,5 Elevated levels of IL-17 have been detected in COVID-19 patients compared to controls, among other mediators.5 This hypothesis is plausible, as other infective agents have been implicated in the pathogenesis of psoriasis, including viruses such as rhinoviruses.2
A case of new onset psoriasis secondary to SARS-CoV-2 infection, the first one to present as erythroderma, is described. Cutaneous complications are a source of significant morbidity linked to COVID-19, as it can not only aggravate previous psoriasis, but also precipitates severe skin disease requiring admission in previously healthy patients.