Neutrophilic urticaria, described by Winkelmann in 1985, has yet to be completely defined and its clinical significance is poorly understood. Nevertheless, recent publications suggest that it could be a marker for rheumatic disease. The primary objective of this study was to compare the prevalence of rheumatic disease in 2 groups of patients with urticaria: those with conventional urticaria (non-neutrophilic inflammatory infiltrate) and those with neutrophilic urticaria.
Material and methodsWe retrospectively reviewed all biopsy samples taken from urticarial lesions in our hospital between January 1, 1999 and June 28, 2009. Urticaria was classified according to predefined morphologic and histopathologic patterns. We compared the clinical and histologic characteristics of neutrophilic urticaria with those of conventional urticarias in the 84 patients included.
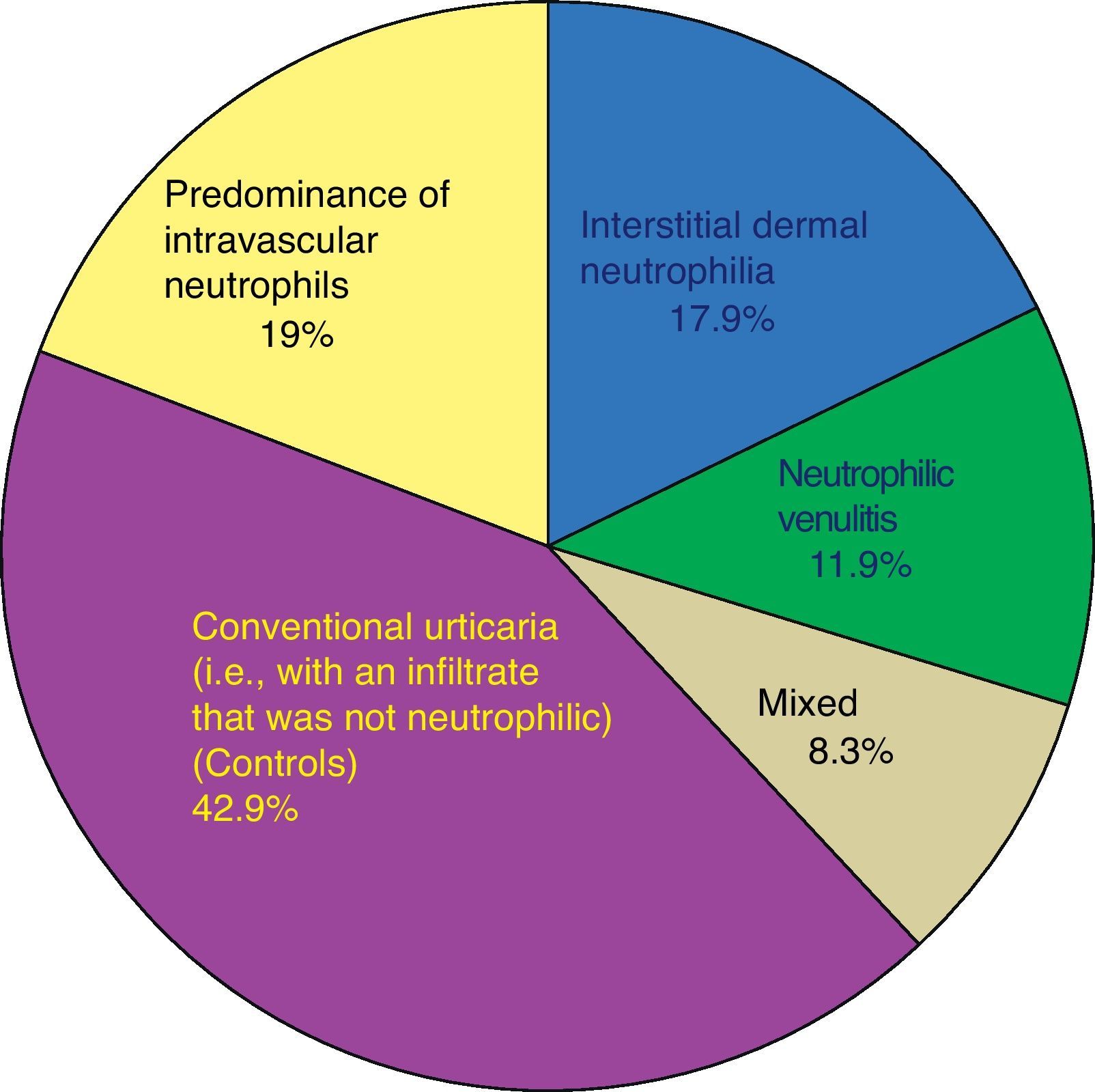
ResultsOf the 84 patients, 57.1% had neutrophilic urticaria. We did not find significant differences between the percentages of patients with rheumatic disease between the neutrophilic and nonneutrophilic urticaria groups. In patients with acute urticaria, we found a significantly higher proportion of samples with histopathologic signs of neutrophilic urticaria as opposed to conventional histopathology. Patients with neutrophilic urticaria also had higher white blood cell counts.
ConclusionsThe percentage of samples with neutrophilic urticaria in this series (57.1%) is higher than the percentages reported in the literature, possibly because we tended to biopsy recent lesions. We highlight that the presence of neutrophils in the biopsies of urticaria is a common finding and does not appear to be associated with other diseases.
La urticaria neutrofílica (UN), descrita por Winkelmann en 1985, es una entidad que no está aún completamente definida y de una relevancia clínica desconocida. No obstante, ha sido considerada en la literatura reciente como marcador de enfermedad reumatológica. El objetivo principal de nuestro estudio es comparar la proporción de enfermedad reumatológica en urticarias con infiltrado predominantemente neutrofílico (UN) respecto a la encontrada en urticarias con infiltrado predominantemente no neutrofílico o convencionales.
Material y métodosDe manera retrospectiva hemos revisado todas las urticarias biopsiadas en nuestro centro entre el 1 de enero de 1999 y el 28 de junio de 2009. Las hemos englobado en varios patrones morfológicos histopatológicos definidos. En los 84 pacientes incluidos hemos comparado las características clínicas e histológicas de las UN con las de las urticarias con infiltrados predominantemente no neutrofílicos o convencionales.
ResultadosDe nuestros 84 pacientes un 57,1% padecían UN. No hemos encontrado diferencias significativas en cuanto a la proporción de enfermedad reumatológica en las UN respecto a las convencionales. Sí hemos encontrado diferencias estadísticamente significativas respecto a la proporción de urticarias agudas con histopatología de UN en relación con aquellas con histopatología convencional, así como un mayor recuento de leucocitos en la UN.
ConclusionesEn nuestra serie la proporción de UN encontradas (57,1%) es mayor que la descrita en la literatura, dato que puede deberse a nuestra tendencia a biopsiar lesiones recientes. Como conclusión de nuestro estudio cabe resaltar que la presencia de neutrófilos en las biopsias de urticaria es un hecho frecuente que no parece asociarse a otras comorbilidades.
Urticaria and angioedema affect at least 20% of the population at some time1 and can be classified according to their clinical characteristics, triggers, or associations with various diseases.2–4
The characteristic lesion of urticaria is the wheal, an edematous pink to red plaque with a pale center. Wheals vary in size, are evanescent, and can coalesce into larger round or archiform lesions.2
The classic histopathologic descriptions of urticaria note the presence of dermal edema, vasodilation, and a perivascular infiltrate of mononuclear cells. The infiltrate consists mainly of lymphocytes, together with neutrophils and eosinophils in varying numbers, usually arranged between the dermal collagen bundles.3,5 To date, however, histopathologic descriptions have varied considerably, owing to the small number of cases that have included histopathology and to the difficulty of establishing the duration of the biopsied lesions; other confounding factors may be involved as well.6
The presence of neutrophils in biopsy specimens of urticarial lesions was first described in Dermatopathology, a 1967 textbook by Montgomery and coauthors, and later by Jones et al7 in a 1983 article in the British Journal of Dermatology (cited in Winkelmann and Reizner8). As early as 1985 Peters and Winkelmann9 posited the existence of a distinct diagnostic entity they called neutrophilic urticaria, characterized by the appearance of wheals in which histology showed neutrophils in the dermal venules and venular walls and no sign of leukocytoclasia, hemorrhage, or fibrinoid necrosis. In Winkelmann and Reizner's8 subsequent retrospective study, they found a diffuse dermal neutrophilic infiltrate in 23 (8.7%) cases and the presence of neutrophils lining or invading the venular walls in another 19 (7.1%) cases. Thus, neutrophilic infiltrates were found in as many as 15.8% of the 256 cases of chronic urticaria. As a result, the histopathologic concept of neutrophilic urticaria was broadened.
In later histopathologic studies of urticaria, higher numbers of neutrophils were found in the dermis of patients with acute urticaria compared to other types and in the reticular dermis of those with pressure urticaria.6 Furthermore, there seems to be a direct relationship between neutrophil and eosinophil counts.6
When Winkelmann et al.5 initially studied the clinical characteristics and comorbidities of 8 patients, no conclusive data emerged with respect to abnormalities in complete blood counts or proteins; nor were there patterns with respect to indicators of autoimmune disease. More recent articles have suggested that urticaria with a neutrophilic infiltrate, or neutrophilic urticaria, might be characterized by shorter flare-ups and by an increase in acute phase reactants. Interleukin-3 and tumor necrosis factor-α seem to be implicated in the pathogenesis of this condition,10 although few studies have focused on how its characteristics differ from those of urticaria with an infiltrate that is not neutrophilic.
More recently, in 2009, Kieffer et al.11 defined a subtype of neutrophilic urticaria characterized by nonedematous lesions lasting up to 48hours. The distribution of the infiltrate and the scant evidence of edema, however, led the authors to consider this subtype to be more similar to acute neutrophilic dermatosis. The authors identified 9 patients with this type of urticaria, which they termed neutrophilic urticarial dermatitis. These patients had interstitial infiltrates of neutrophils distributed either individually or arranged linearly; no vascular damage was observed. The authors concluded that this subtype may be particularly associated with rheumatic disease.
The histopathologic differential diagnosis of neutrophilic urticaria requires mainly consideration of urticarial vasculitis. In theory, they can be distinguished because of the presence of vascular damage in urticarial vasculitis as evidenced by areas of postcapillary fibrinoid necrosis (in venules).1 Nonetheless, rigorous diagnostic criteria have not been applied in most studies of urticarial vasculitis, and in a published series of patients with this disease, fibrin deposition was detected in samples from only 9.9% of patients,12 many of whom presented a neutrophilic infiltrate with only slight or no vascular abnormalities.1 Additionally, in some published cases of hypocomplementemic urticarial vasculitis, clinical features and histologic findings in the urticarial lesions completely overlapped with those of neutrophilic urticaria.13 In a prospective study of lesions clinically suggestive of urticarial vasculitis, it was observed that there was in fact no vasculitis in the majority of cases and that a finding of a predominance of polymorphonuclear cells on histology was associated with the presence of fibrin, leukocytoclasia, low complement levels, and anemia.12 The problem of the overlap between the 2 diagnoses was pointed out by Winkelmann et al.5 in their initial description of neutrophilic urticaria, in which they stated that its peculiar histopathology might be suggestive of an underlying vasculitis. This hypothesis was not subsequently explored, however. To complicate matters further, the true incidence of leukocytoclastic vasculitis is unknown; nor do we understand its prognostic significance in other types of urticaria, such as solar14,15 or cold urticaria.16–18
In short, neutrophilic urticaria is a clinical entity that partially overlaps with urticarial vasculitis. Much about the condition remains poorly understood, including its true incidence and its association with a higher incidence of systemic conditions, particularly of rheumatic disease.
The primary objective of our study was to compare the prevalence of rheumatic disease in 2 groups of patients: those with neutrophilic urticaria (defined as urticaria with a neutrophilic infiltrate) and those with urticaria with a lymphocytic infiltrate that is not predominantly neutrophilic.
Our secondary objectives were to compare the epidemiologic and histopathologic data for neutrophilic urticaria to all other urticarias that do not fall into that category, as well as to findings previously described in the literature.
Material and MethodsWe carried out a descriptive, retrospective study using the database of our hospital's pathology department for the period between January 1, 1999 and June 28, 2009 to locate the cases of urticaria for which the results of skin lesion biopsies were available.
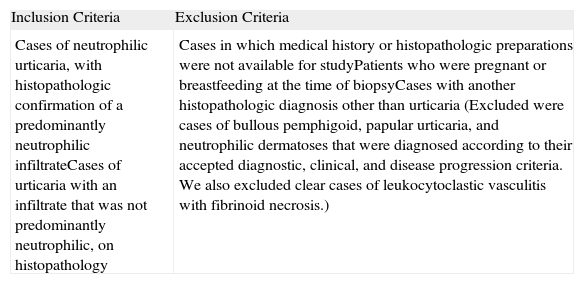
Our inclusion and exclusion criteria are shown in Table 1.
Inclusion and Exclusion Criteria.
| Inclusion Criteria | Exclusion Criteria |
| Cases of neutrophilic urticaria, with histopathologic confirmation of a predominantly neutrophilic infiltrateCases of urticaria with an infiltrate that was not predominantly neutrophilic, on histopathology | Cases in which medical history or histopathologic preparations were not available for studyPatients who were pregnant or breastfeeding at the time of biopsyCases with another histopathologic diagnosis other than urticaria (Excluded were cases of bullous pemphigoid, papular urticaria, and neutrophilic dermatoses that were diagnosed according to their accepted diagnostic, clinical, and disease progression criteria. We also excluded clear cases of leukocytoclastic vasculitis with fibrinoid necrosis.) |
We studied 84 patients for whom we had complete access to both clinical and histopathologic data and in whom we could rule out the possibility of other diseases.
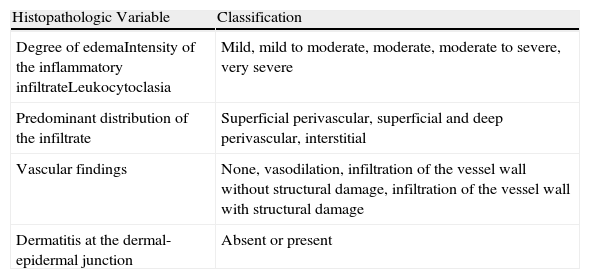
HistopathologyBiopsy specimens were fixed in 10% buffered formaldehyde for at least 24hours and were routinely processed into 5-μm sections and stained with hematoxylin-eosin. Each specimen was examined at different magnifications (up to ×400) and evaluated independently by 2 specialists, a pathologist and a dermatologist (J.F.F. and M.L.V.). Any disagreements were settled with the help of another dermatologist (J.S.P.). The histopathologic aspects analyzed in each case are shown in Table 2.
Histopathologic Features Analyzed.
| Histopathologic Variable | Classification |
| Degree of edemaIntensity of the inflammatory infiltrateLeukocytoclasia | Mild, mild to moderate, moderate, moderate to severe, very severe |
| Predominant distribution of the infiltrate | Superficial perivascular, superficial and deep perivascular, interstitial |
| Vascular findings | None, vasodilation, infiltration of the vessel wall without structural damage, infiltration of the vessel wall with structural damage |
| Dermatitis at the dermal-epidermal junction | Absent or present |
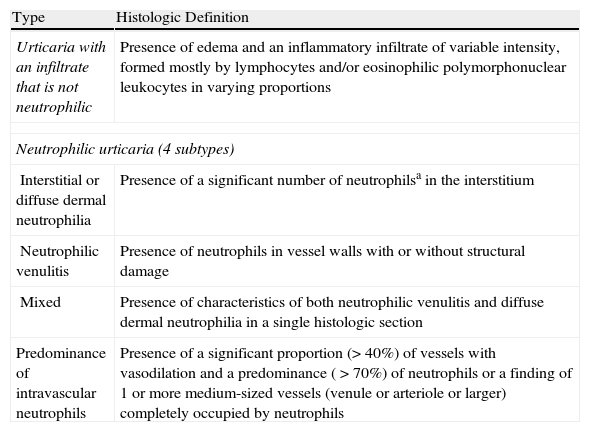
The biopsy that was most representative of the findings for each was classified into one of the following groups:
- 1
Conventional urticaria with an infiltrate that was not neutrophilic (control group)
- 2
Urticaria with a neutrophilic inflammatory infiltrate. This group consists of several subtypes: a) diffuse dermal neutrophilia, b) neutrophilic venulitis, c) mixed (diffuse dermal neutrophilia plus neutrophilic venulitis), and d) urticaria in which the neutrophils were mainly intravascular.
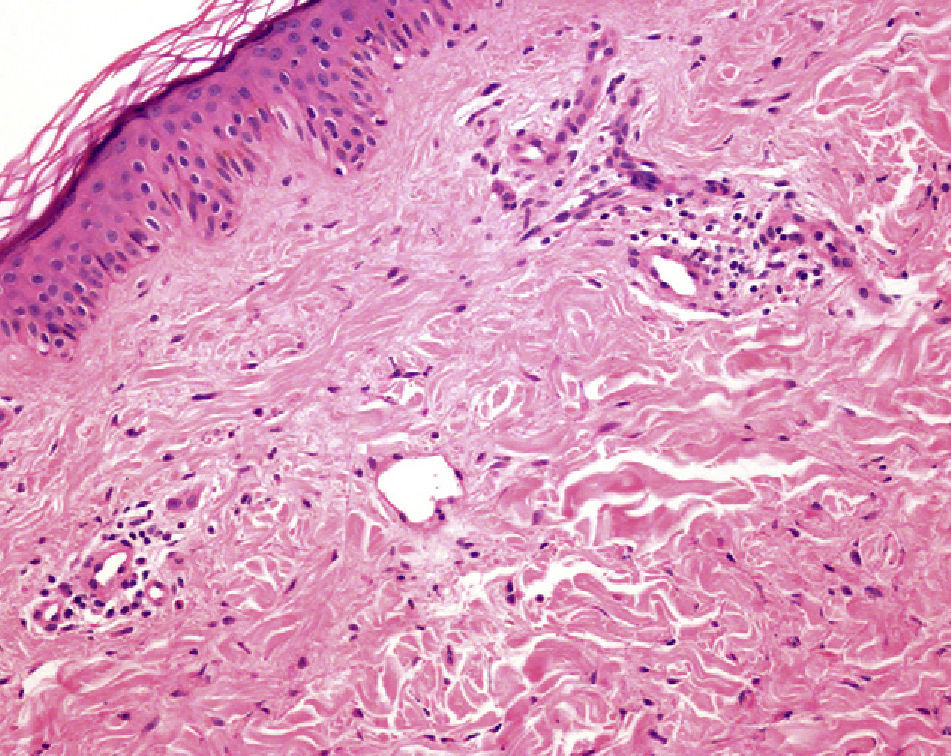
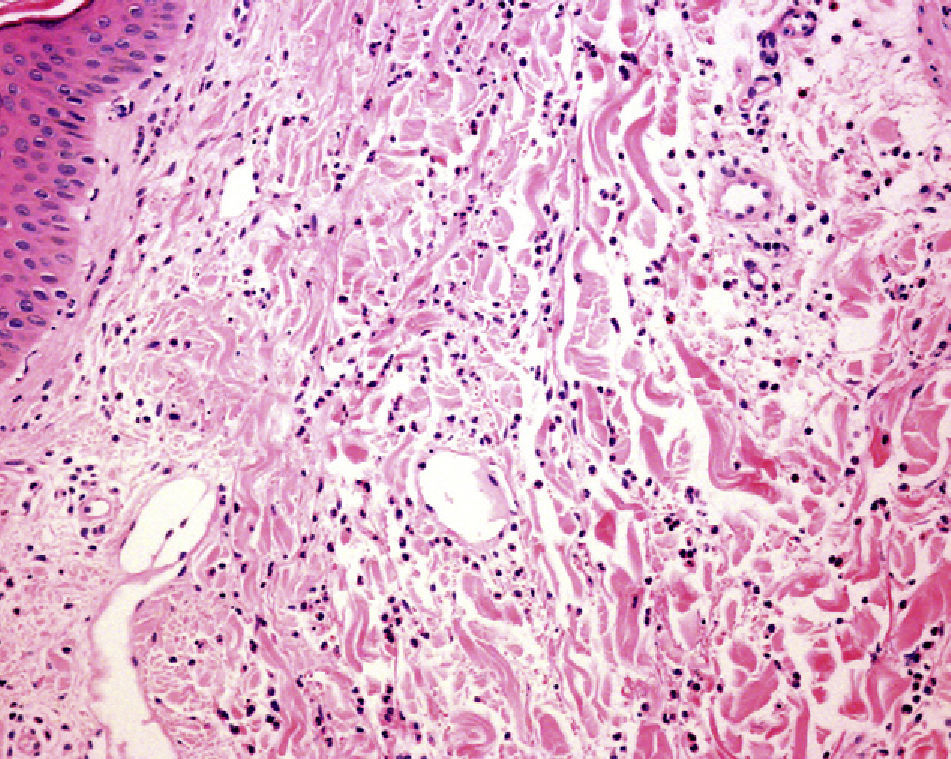
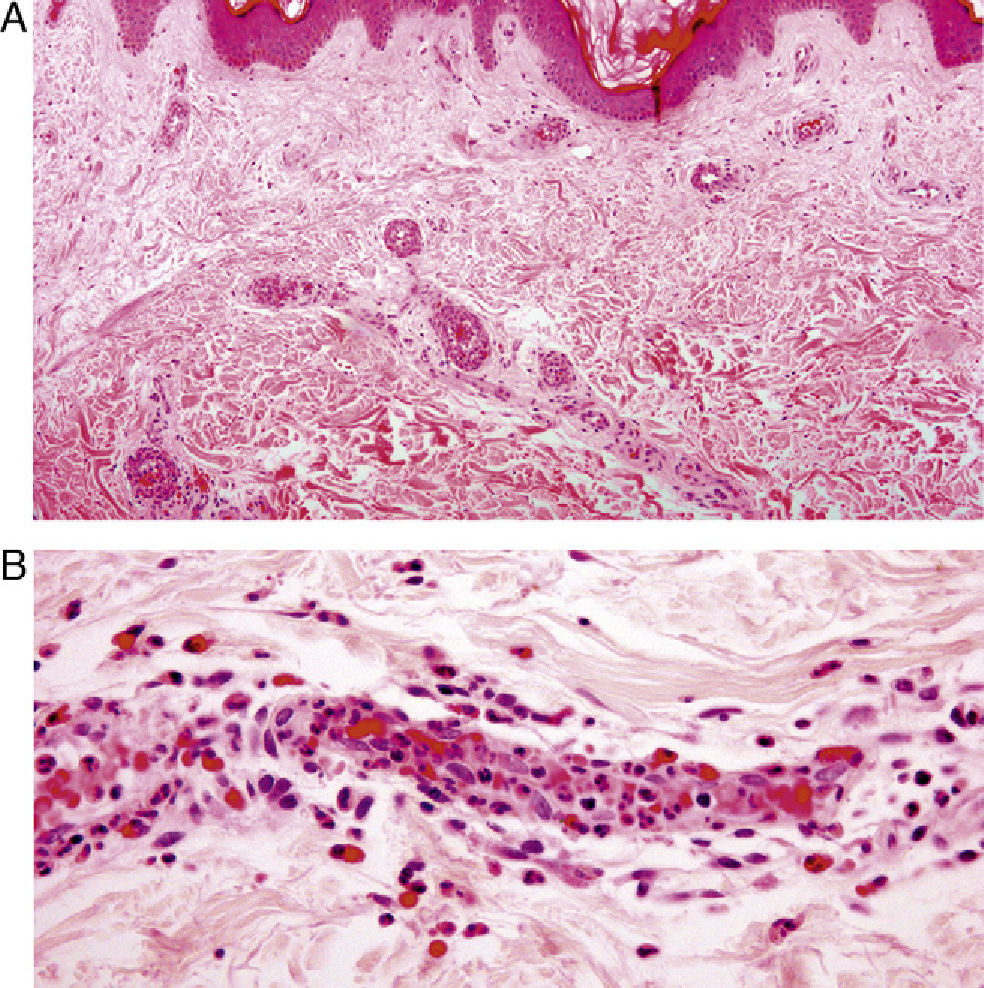
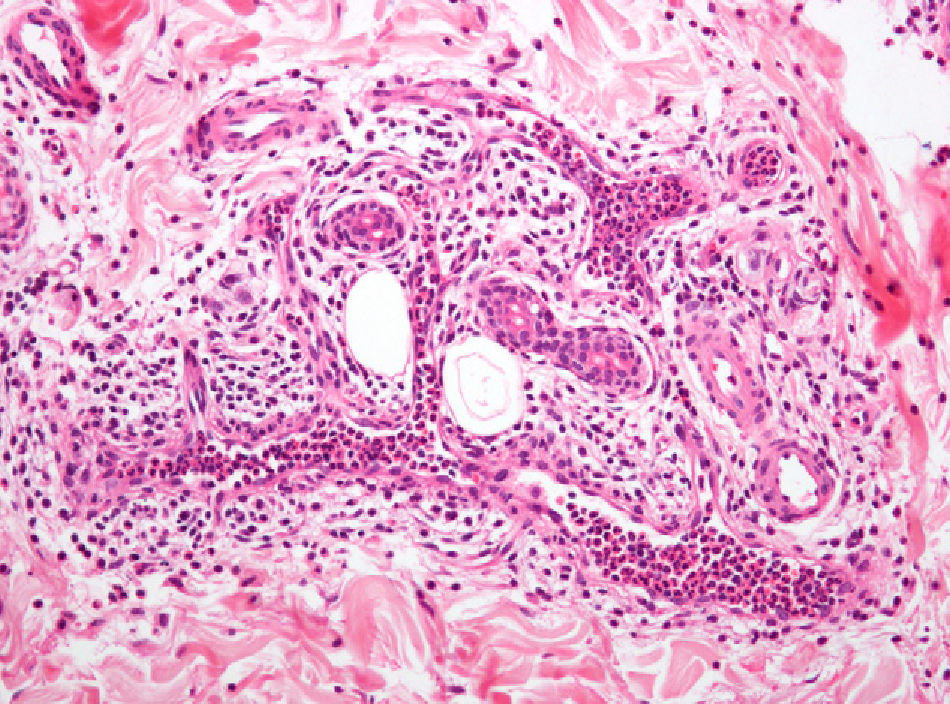
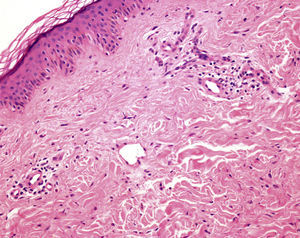
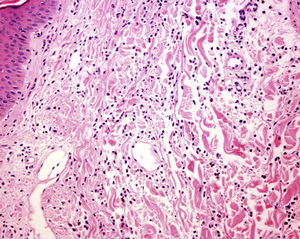
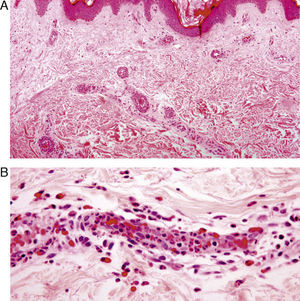
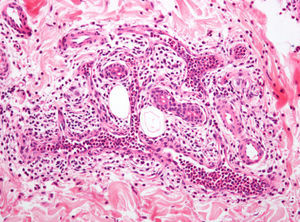
The definitions used for each of these groups and subgroups are specified in Table 3 and are illustrated with prototypical examples (Figs. 1–4).
Histopathologic Definitions of the Different Types of Urticaria in the Study.
| Type | Histologic Definition |
| Urticaria with an infiltrate that is not neutrophilic | Presence of edema and an inflammatory infiltrate of variable intensity, formed mostly by lymphocytes and/or eosinophilic polymorphonuclear leukocytes in varying proportions |
| Neutrophilic urticaria (4 subtypes) | |
| Interstitial or diffuse dermal neutrophilia | Presence of a significant number of neutrophilsa in the interstitium |
| Neutrophilic venulitis | Presence of neutrophils in vessel walls with or without structural damage |
| Mixed | Presence of characteristics of both neutrophilic venulitis and diffuse dermal neutrophilia in a single histologic section |
| Predominance of intravascular neutrophils | Presence of a significant proportion (> 40%) of vessels with vasodilation and a predominance ( >70%) of neutrophils or a finding of 1 or more medium-sized vessels (venule or arteriole or larger) completely occupied by neutrophils |
aSignificant number of neutrophils was defined as the presence of more than 10 to 15 interstitial neutrophils per visual field at a magnification of ×200, in 2 or more fields, whether adjacent or not, provided they are found in a single section.
The following information was collected from patients’ medical histories: age, sex, personal history, smoking history, long-term medication, date of first visit, time since onset of disease, frequency and site of flare-ups, (type of lesion, duration, presence or absence of residual lesion after resolution, and symptoms), associated systemic symptoms, hemoglobin values, total white blood cell and differential counts, blood sugar, transaminase levels, erythrocyte sedimentation rate, presence of antibodies, complement abnormalities, parasites in stool, and serum levels of IgE. Examples of our patients’ lesions are shown in Fig. 5.
Statistical analysis of the data was carried out using the SPSS statistical package, version 18. Statistical significance testing was performed using G-Stat software, version 2.0.
ResultsPatientsOf the 84 patients studied, 58.3% were women. Mean age at the time of biopsy was 46.49 years (range, 12-79 years).
The median duration of urticaria flare-ups prior to biopsy was 45 days and 42.9% of the cases were acute, that is, urticaria that had appeared less than 6 weeks before biopsy. Two patients had physical urticaria triggered by exposure to cold. Most of the biopsied lesions were wheals (64.9%) or plaques (22.1%) in a generalized distribution (34.7%). Lesions lasting more than 24hours were reported by 55% of patients, although only 14.3% had residual lesions. Histopathology of the lesions that had lasted more than 24hours (n = 39) showed that 56.4% had an infiltrate that was not neutrophilic. In the remaining 17 patients (43.5%) with a neutrophilic infiltrate, inflammation was mainly perivascular in 10 cases (with marked presence of intravascular neutrophils in 7, neutrophilic venulitis in 2, and mixed in 1 case). The most frequent symptoms were pruritus (80%), pain (5.3%), or both (5.3%).
Systemic symptoms associated with flare-ups were present in 51.2% of patients. Of the 84 patients, 81% had no rheumatic disease; in the others, the following conditions were observed: adult-onset Still disease (n = 3), lupus erythematosus (n = 3: 2 cases of systemic lupus erythematosus and 1 of chronic discoid lupus), rheumatoid arthritis (n = 2), fibromyalgia (n = 2), migratory joint pain of unknown origin (n = 2), and overlap syndrome, polymyalgia rheumatica, Sjögren disease, seronegative arthropathy, and microscopic polyarteritis nodosa (1 case each). One patient was diagnosed simultaneously with systemic lupus erythematosus and rheumatoid arthritis.
Blood tests revealed that 23.2% of patients had a slight increase in acute-phase reactants and only 1 patient (1.2%) had associated monoclonal hypergammaglobulinemia.
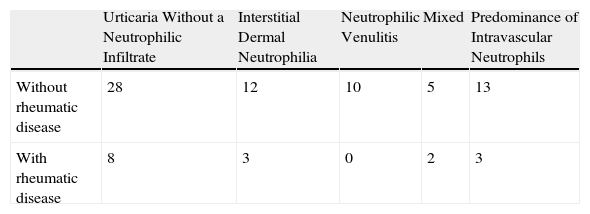
Comparison Between the Two Groups: Neutrophilic Uriticaria Compared to Conventional Uriticaria With a Non-neutrophilic InfiltrateAs age and sex distribution was similar in patients with neutrophilic urticaria and those with an infiltrate that was not neutrophilic, the 2 groups can be considered comparable. With respect to the primary objective of our study, we found no significant differences between the 2 groups in the percentage of patients with rheumatic disease in either the global analysis or the analysis by histopathologic subtypes (Pearson's χ2 test; P = 0.585) (Table 4).
Contingency Table of Presence or Absence of Rheumatic Disease in the Various Histologic Subtypesa.
| Urticaria Without a Neutrophilic Infiltrate | Interstitial Dermal Neutrophilia | Neutrophilic Venulitis | Mixed | Predominance of Intravascular Neutrophils | |
| Without rheumatic disease | 28 | 12 | 10 | 5 | 13 |
| With rheumatic disease | 8 | 3 | 0 | 2 | 3 |
aThe χ2 test showed no significant differences between the groups (P = .585).
It is noteworthy that histopathologic signs of neutrophilic urticaria were more frequent in biopsies of acute urticaria, whereas there was no difference between the 2 groups with respect to the most common duration (more or less than 24hours) of the lesions or the presence of residual hyperpigmentation.
A comparison of various analytic parameters (hemoglobin values, total and differential white blood cell counts, erythrocite sedimentation rate, presence of antibodies, complement abnormalities, and serum IgE levels) showed significant differences only in mean white blood cell counts, which were higher in patients with neutrophilic urticaria.
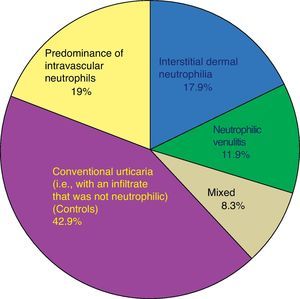
Each biopsy was classified according to the histopathologic patterns mentioned above: the infiltrate was not neutrophilic in 36 patients (42.9%) and neutrophilic in 48 (57.1%). Within the neutrophilic urticaria group, the patterns most frequently found were urticaria with a predominance of intravascular neutrophils (19%) and diffuse dermal neutrophilia (17.9%). The distribution of subtypes is shown in Fig. 6.
In the cases with an infiltrate that was not neutrophilic, the perivascular distribution was either superficial (75%) or superficial and deep (25%), generally without leukocytoclasia (97.2%). Furthermore, while 45.8% of the biopsies showed an interstitial distribution of the infiltrate in cases of neutrophilic urticaria, this pattern was not seen cases with an infiltrate that was not neutrophilic. This difference was statistically significant (Table 5).
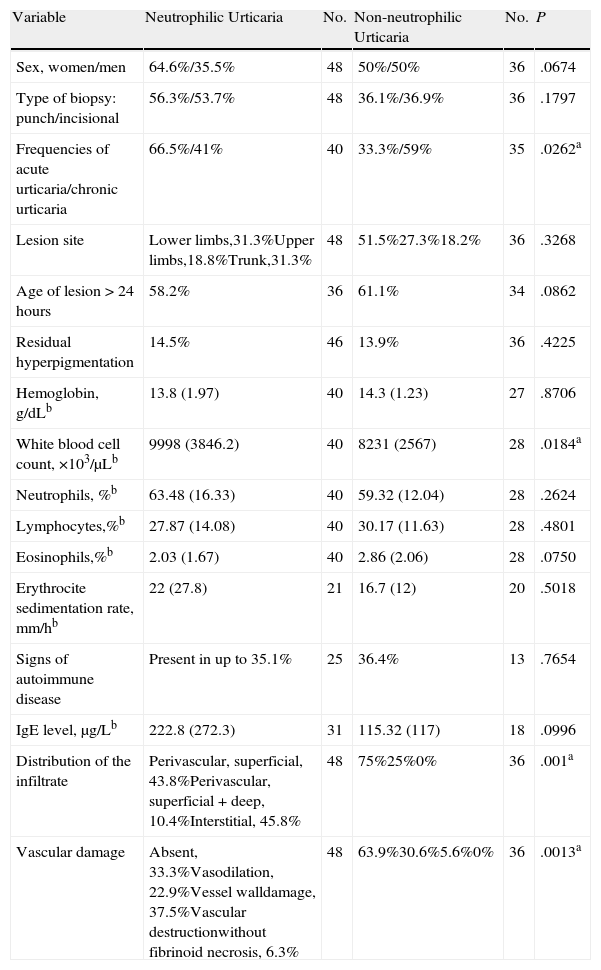
Comparison of Clinical, Analytical, and Histopathologic Data Between Cases With and Without Neutrophilic Urticaria.
| Variable | Neutrophilic Urticaria | No. | Non-neutrophilic Urticaria | No. | P |
| Sex, women/men | 64.6%/35.5% | 48 | 50%/50% | 36 | .0674 |
| Type of biopsy: punch/incisional | 56.3%/53.7% | 48 | 36.1%/36.9% | 36 | .1797 |
| Frequencies of acute urticaria/chronic urticaria | 66.5%/41% | 40 | 33.3%/59% | 35 | .0262a |
| Lesion site | Lower limbs,31.3%Upper limbs,18.8%Trunk,31.3% | 48 | 51.5%27.3%18.2% | 36 | .3268 |
| Age of lesion > 24hours | 58.2% | 36 | 61.1% | 34 | .0862 |
| Residual hyperpigmentation | 14.5% | 46 | 13.9% | 36 | .4225 |
| Hemoglobin, g/dLb | 13.8 (1.97) | 40 | 14.3 (1.23) | 27 | .8706 |
| White blood cell count, ×103/μLb | 9998 (3846.2) | 40 | 8231 (2567) | 28 | .0184a |
| Neutrophils, %b | 63.48 (16.33) | 40 | 59.32 (12.04) | 28 | .2624 |
| Lymphocytes,%b | 27.87 (14.08) | 40 | 30.17 (11.63) | 28 | .4801 |
| Eosinophils,%b | 2.03 (1.67) | 40 | 2.86 (2.06) | 28 | .0750 |
| Erythrocite sedimentation rate, mm/hb | 22 (27.8) | 21 | 16.7 (12) | 20 | .5018 |
| Signs of autoimmune disease | Present in up to 35.1% | 25 | 36.4% | 13 | .7654 |
| IgE level, μg/Lb | 222.8 (272.3) | 31 | 115.32 (117) | 18 | .0996 |
| Distribution of the infiltrate | Perivascular, superficial, 43.8%Perivascular, superficial + deep, 10.4%Interstitial, 45.8% | 48 | 75%25%0% | 36 | .001a |
| Vascular damage | Absent, 33.3%Vasodilation, 22.9%Vessel walldamage, 37.5%Vascular destructionwithout fibrinoid necrosis, 6.3% | 48 | 63.9%30.6%5.6%0% | 36 | .0013a |
aFor a 95% CI, values of P < 0.05 were considered to be statistically significant.
bData are means (SD) unless otherwise indicated.
Vascular abnormalities were observed in 66.7% of the patients with neutrophilic urticaria, with damage to vessel walls but no destruction in 43.8% and with destruction in 6.3%. No fibrinoid necrosis was found in any case. In cases with an infiltrate that was not neutrophilic, there was either no vascular damage (63.9%) or only vasodilation (30.6%). The statistical analysis also showed significant differences between the 2 groups with respect to vascular involvement, which was more frequent and more intense in the neutrophilic urticaria group.
No epidermal abnormalities were observed in any of the cases and only 1 patient with neutrophilic urticaria had interface dermatitis with vacuolar degeneration, with no findings suggestive of connective tissue disease.
Table 5 shows the distribution of other dichotomous variables between the 2 groups (compared with the χ2 test) and some of the quantitative variables (compared with the t test).
DiscussionThe primary objective of our study was to determine whether or not there was a greater prevalence of rheumatic disease among patients with neutrophilic urticaria. However, we failed to find any such association with neutrophilic urticaria in general or with any of its histologic subtypes. According to the literature, the estimated difference in the prevalence of rheumatic disease between patients with neutrophilic urticaria or another type is at least as high as 30% to 50%. The power of our study, with a total of 84 patients, to detect differences not due to chance was approximately 80%.
In our series 14.6% of patients with neutrophilic urticaria and 22.2% of those with conventional urticaria (without such an infiltrate) had rheumatic disease. In contrast, Kieffer et al.11 found rheumatic disease in up to 77.7% of their patients. In their article they defined neutrophilic urticarial dermatosis as marked by the presence of erythematous nonpruritic lesions lasting less than 48hours and histologically characterized by considerable interstitial and perivascular involvement, with neutrophils distributed between the collagen bundles either individually or in lines. Curiously, although the presence of edema was one of their exclusion criteria, edema could be seen in their microphotographs. After a critical reading of their article, we have come to the conclusion that the entity that we have included in the category of diffuse dermal neutrophilia overlaps, at least histopathologically, with the one they called neutrophilic urticarial dermatosis. Moreover, in 59% of our patients with diffuse dermal neutrophilia, the clinical lesions were not evanescent. Our results, therefore, are not consistent with those of Kieffer et al. and lend support to the earlier hypothesis that there is no association between neutrophilic urticaria and other diseases.5 However, our study is not directly comparable to theirs, as our criteria did not exclude patients with histopathologically edematous lesions or require the presence of recurrent flare-ups.
Apart from mentioning the overlap between neutrophilic urticaria and urticarial vasculitis that we have referred to above, current reviews do not consider neutrophilic urticaria to be a well defined subtype of urticaria.2 We thus had to define the criteria and histopathologic patterns needed to classify the biopsies of the urticarial lesions in our study. The inflammatory infiltrates found in biopsies of urticarial lesions are indications of an underlying dynamic process. In a study of 22 patients with chronic idiopathic urticaria from whom 2 biopsies were obtained (one of a lesion that appeared less than 4hours earlier and another of one that appeared more than 12hours earlier), Sabroe et al.19 demonstrated this dynamic process, observing a predominance of polymorphonuclear cells in blood and in vessel walls in the more recent lesions and a tendency towards interstitial distribution in older lesions. In our study we identified a group of patients with neutrophilic infiltrates both in the dermis and in some vessel walls; these results support the theory of the dynamic nature of the inflammatory infiltrate of urticarial wheals.8
In our series 57.1% of patients had a neutrophilic pattern of urticaria. Of these, 17.9% were cases of diffuse dermal neutrophilia. In the series of Winkelmann and Reizner,8 only 15.8% of cases had neutrophilic urticaria and 8.7% of these showed a dermal inifiltrate with a diffuse or interstitial distribution. In 26% of their patients they observed a perivascular concentration of neutrophils,8 as we did in the majority of ours. Toppe et al10 found a predominantly neutrophilic pattern in more cases of clinically acute urticaria (55%) than in chronic urticaria (18%). Neutrophils were found inside vessels or in vessel walls in 29.1% of their biopsies. As mentioned above, the study of Sabroe et al.19 suggested that the distribution depended on the age of the lesion.19 While in our study the exact age of the wheal before biopsy was unknown, our hospital tends to select recent lesions for biopsy and this could account for the higher percentage of neutrophilic urticaria in our series. Furthermore, although our inclusion criteria did not take clinical data into account, the urticarial lesions biopsied in our hospital were those with clinical findings suggestive of neutrophilic vasculitis and, to a lesser extent, clinically atypical cases that raised doubts as to diagnosis or that responded poorly to treatment. Our finding that a neutrophilic pattern was more frequent in patients with chronic urticaria is consistent with the increase in dermal neutrophils found in acute urticaria compared to other types described by Toppe et al.6
Winkelmann et al.5 considered that the rare presence of leukocytoclasia, the absence of fibrinoid necrosis, and the scant presence or total absence of red blood cell extravasation in the histologic sections they reviewed could serve to differentiate cases of neutrophilic urticaria from those of leukocytoclastic vasculitis or urticarial vasculitis. In the light of our histologic findings, however, this possibility seems somewhat doubtful, as we found varying degrees of vascular damage. Dense perivascular infiltrates with leukocytoclasia and, more rarely, small points of fibrinoid necrosis can be found in the biopsies of up to 52% of patients with urticaria.20 Clear vascular damage, with destruction of the vessel walls but without fibrinoid necrosis, was found in only 6.3% of our patients with neutrophilic urticaria. With less rigid criteria for vascular damage, up to 60.4% of those cases could have been considered urticarial vasculitis. In contrast, no vascular abnormalities were found when the infiltrate was not neutrophilic. Our study suggests that the disparity in the frequency of vascular damage found in the various series described in the literature might be due to the inclusion of differing percentages of patients with neutrophilic urticaria.
Blood tests showed only 1 significant difference between the 2 groups: white blood cell counts in peripheral blood were higher in patients with neutrophilic urticaria, a finding described previously.
The main limitation of our study, resulting from its retrospective design, was the lack of homogeneity in the clinical and laboratory data and in the duration of follow-up. Consequently, we were unable to analyze some of the data. Moreover, in the absence of reliable information concerning the age of the wheals, we were unable to study possible differences in the composition of the inflammatory infiltrates and their development over time. The lack of this information and of generally accepted criteria for neutrophilic urticaria may explain why we could not rule out the possibility that in some of the cases included in our study the differences found between the 2 groups might be attributable to having biopsied lesions at different points in their development, making it more difficult to interpret the data.
ConclusionsThe frequency of a neutrophilic inflammatory infiltrate in biopsy specimens of urticarial lesions is high (57.1%), especially in patients with acute urticaria. None of the different histologic patterns found in neutrophilic urticaria seems to be associated with a greater prevalence of rheumatic disease compared to urticaria with infiltrates that are not neutrophilic.
Neutrophilic urticaria could be a reaction pattern that is intermediate between urticaria with an infiltrate that is not neutrophilic and urticarial vasculitis with fibrinoid necrosis. To determine whether neutrophilic urticaria and urticarial vasculitis are 2 different entities, however, would require a prospective study, given the frequent presence of vascular damage in patients with neutrophilic urticaria and its overlap with urticarial vasculitis.
Conflicts of InterestThe authors declare that they have no conflicts of interests.
Please cite this article as: M. Llamas-Velasco, J. Fraga, L. Requena, J. Sánchez-Pérez, E. Ovejero- Merino, A. García-Diez. Urticaria con infiltrado inflamatoria de predominio neutrofílico o urticaria neutrofílica. Estudio de sus características clínicas e histopatológicas y de su posible asociación con enfermedad reumatológica. Actas Dermosifiliogr. 2012;103:511-9.