Traditionally, psoriasis was considered to be a purely cutaneous disease affecting otherwise healthy patients (except for joint involvement). Recent studies have, however, shown a relationship between psoriasis and cardiovascular disease, with increased mortality in patients who have severe forms of psoriasis.
Dermatologists are thus in a position to play an important role in identifying patients at greater risk of cardiovascular disease and detecting potential risk factors that are, for the most part, manageable and avoidable.
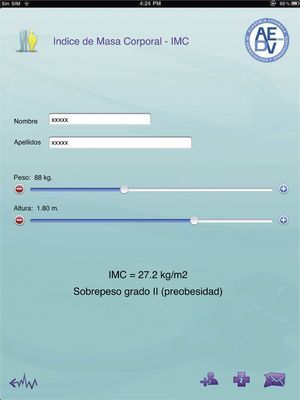
To this end, we designed a multiplatform application that provides a simple and intuitive tool to determine body mass index, whether or not metabolic syndrome is present, and cardiovascular risk. The application runs on iOS, Android, and the webpage of the Psoriasis Group of the Spanish Academy of Dermatology and Venereology (AEDV).
La psoriasis se ha considerado tradicionalmente (en ausencia de artropatía) como una enfermedad puramente cutánea que afecta por lo general a individuos sanos. Pero estudios recientes han demostrado una relación entre psoriasis y enfermedad cardiovascular, con un incremento de la mortalidad de aquellos pacientes con psoriasis graves.
En este sentido, los dermatólogos podemos desempeñar un importante papel en la identificación de aquellos pacientes con un mayor riesgo de enfermedad cardiovascular detectando potenciales factores de riesgo en su mayoría tratables y evitables.
Por este motivo hemos diseñado una aplicación multiplataforma que permite calcular de una manera sencilla e intuitiva el índice de masa corporal, la presencia o no de síndrome metabólico y el riesgo cardiovascular de nuestros pacientes, disponible para dispositivos móviles iOS, Android y en la página web del Grupo de Psoriasis de la Academia Española de Dermatología y Venereología (AEDV).
Psoriasis affects between 1.5% and 3% of the world population. When there is no joint involvement, it has traditionally been considered as a chronic inflammatory disease of the skin that affects otherwise healthy individuals, with a negative impact on their quality of life.1 However, recent studies have suggested that psoriasis is not an isolated phenomenon but occurs in association with other conditions, such as cardiovascular diseases, and that mortality is higher in patients with severe forms of psoriasis.2–4
The link between psoriasis and arteriosclerosis seems to arise as a result of both the increased prevalence of various cardiovascular risk factors and chronic inflammatory phenomena in these patients.
It is not uncommon for dermatologists to be the only health care professional to see an apparently healthy individual with psoriasis. Dermatologists can therefore play an important role in identifying patients who, in addition to psoriasis, may have an elevated risk of cardiovascular disease and early death. Thus, we can detect potential modifiable and avoidable risk factors, recommend lifestyle changes, and refer individuals at risk to their family physician in the event that pharmacological treatment or a closer follow-up is needed.
Despite the progress in our understanding of psoriasis and our realization that it is a chronic inflammatory disease not limited to the skin, large barriers remain when incorporating this knowledge into clinical practice. As physicians, dermatologists should provide the patients with advice and counseling about their disease. If we manage to get the patients to better understand the relationship between psoriasis and other diseases, we can encourage greater determination on their part to change their lifestyle, give up deleterious habits, and adhere to therapy.5
Psoriasis and Metabolic SyndromeObesity, especially abdominal obesity (also known as central obesity), is associated with resistance to the effects of insulin on peripheral glucose and fatty acid utilization. This can lead to type 2 diabetes. Insulin resistance, with the resulting hyperinsulinemia and hyperglycemia, as well as adipokines (cytokines secreted by adipocytes), can lead to endothelial vascular dysfunction, an abnormal lipid profile, hypertension, and vascular inflammation, all of which favor the development of arteriosclerotic cardiovascular disease.6
The term metabolic syndrome was proposed to indicate a situation where certain metabolic risk factors for the development of type 2 diabetes and cardiovascular disease (abdominal obesity, hyperglycemia, dyslipidemia, and hypertension) are present at the same time.7
Definitions of metabolic syndrome vary, although the most widely used are those proposed by the National Cholesterol Education Program/Adult Treatment Panel (NCEP/ATP III) and the International Diabetes Federation (IDF).
The 2001 definition of metabolic syndrome by the NCEP/ATP III (updated in 2005) established diagnosis of metabolic syndrome when 3 or more of the 5 criteria listed in Table 1 are present.8,9
Definition of Metabolic Syndromea According to the National Cholesterol Education Program/Adult Treatment Panel (NCEP/ATP-III) 2005.
| Men | Women | |
| Waist circumference | >102cm | >88cm |
| Serum triglycerides | ≥150mg/dL or lipid-lowering treatment | |
| Serum HDL cholesterol | <40mg/dL or lipid-lowering treatment | <50mg/dL or lipid-lowering treatment |
| Blood pressure | ≥130/85mm Hg or antihypertensive treatment | |
| Fasting glucose | ≥100mg/dL or treatment for hyperglycemia |
Abbreviation: HDL, high-density lipoprotein.
The IDF proposed its criteria for metabolic syndrome in 2004. In this case, central obesity is an essential criterion (with variation according to race/ethnic origin of the patient—in the case of Europeans, a waist circumference >94cm for men and >80cm for women).10 Two of the other 4 criteria, which coincide with those of the ATP-III, also need to be met.
According to different meta-analyses, meeting the definition of metabolic syndrome is associated with a relative risk of type 2 diabetes of 5.12 (95% CI, 3.26–8.05), although the difference seems minimal when only fasting glucose levels are considered.11 Other studies estimate the relative risk of cardiovascular death to be 1.74 (95% CI, 1.29–2.35).12–14
Although metabolic syndrome has been proposed as a simple clinical tool for predicting type 2 diabetes and cardiovascular disease, many authors have questioned the concept of this syndrome in recent years. Criticisms include the lack of agreement in the diagnostic criteria, the lack of a unique pathophysiological mechanism, the omission of important known risk factors (age, tobacco use, sex, low-density lipoprotein [LDL] cholesterol, etc.), the inclusion of patients already diagnosed with diabetes and cardiovascular disease, and the fact that treatment is no different to when the components are taken separately. Thus, some authors propose that metabolic syndrome be considered a premorbid condition rather than a clinical diagnosis, although the concept is clearly useful for health education.15–18
Several studies have found an association between psoriasis and metabolic syndrome. According to Gisondi et al.,19 in a case–control study, 30.1% of patients aged over 40 years with psoriasis met the criteria for metabolic syndrome, with an odds ratio (OR) of 1.65 (95% CI, 1.16–2.35), regardless of tobacco use. The association was stronger in patients with longer-standing disease.
Other studies have found a higher prevalence, up to 44%, for metabolic syndrome in psoriasis patients over 40 years.20
Psoriasis and ObesityObesity has reached epidemic proportions in Europe, where the prevalence has tripled in the past 20 years. It is estimated that 150 million adults (20% of the population) and 15 million children and adolescents (10%) are obese. According to data from the Spanish Health Survey (2003), 13.3% of the Spanish population is obese. The predominance of obesity is slightly higher in women (13.5%) than men (13%).
Diagnosis of obesity is established according to body mass index (BMI) which is calculated by dividing weight in kilograms by the square of height in meters. According to the value, patients can be classified as normal weight (18.5–24.9kg/m2), overweight (25–29.9kg/m2), or obese (>30kg/m2) (Table 2).
Definition of Obesity According to Body Mass Index (BMI).
| BMI, kg/m2 | Definition |
| 18.5–24.9 | Normal weight |
| 25.0–26.9 | Grade I overweight |
| 27.0–29.9 | Grade II overweight (preobesity) |
| 30.0–34.9 | Grade I obesity |
| 35.0–39.9 | Grade II obesity |
| 40.0–49.9 | Grade III obesity (morbid obesity) |
| ≥50 | Grade IV obesity (super-obesity) |
For years, psoriasis has been known to be associated with obesity,21 although it has been debated whether obesity causes or is a consequence of psoriasis.22
In an Italian case–control study of 560 patients, for a BMI of 26–29kg/m2 and >30kg/m2, the OR of having psoriasis was 1.6 and 1.9, respectively, compared to absence of obesity.23 A British study of 127706 patients with mild psoriasis and 3854 patients with severe psoriasis showed that for severe psoriasis and mild psoriasis, the OR for obesity was 1.8 and 1.3, respectively, compared to absence of psoriasis.24
Several hypotheses have been put forward to explain the association between psoriasis and obesity, such as social isolation, poor dietary habits, depression, alcohol consumption, and sedentary lifestyle (in particular in patients with psoriatic arthritis). In fact, only 43% of obese patients with psoriasis in the study of Herron et al.25 exercised for 30minutes or more 2 or 3 times a week, compared to 59% of nonobese patients with psoriasis.
Given that obesity is now considered as a proinflammatory state and that fatty tissue is thought of as an organ with immune and endocrine functions, it is easier to understand why obese patients might be predisposed to the development of psoriasis. Tumor necrosis factor (TNF) α expression is increased in adipocytes of obese rats, and this finding has also been demonstrated in humans. Some authors maintain that the proadipogenic effects of TNF-α are caused by direct autocrine or paracrine effects in the adipose tissue. Furthermore, TNF-α is thought to contribute to insulin resistance.26
Finally, we should remember that body weight can have an effect on the efficacy of psoriasis drugs. It has even been suggested that systemic treatment of psoriasis in obese patients could protect against cardiovascular disease, as shown in a study with methotrexate.27 Finally, it is necessary to consider the increase in the risk of adverse reactions when these patients are treated with certain drugs (acitretin, methotrexate, ciclosporin, etc.).25,27,28
Psoriasis and Cardiovascular RiskArteriosclerosis is responsible for most cases of coronary artery disease. A wide range of factors, often acting in combination, are associated with an increased risk of developing atheromatous plaques in the coronary arteries and other arteries.
The importance of detecting these risk factors lies in the fact that, for the most part, they can be modified by applying specific preventive measures. In the INTERHEART study, which included patients from 52 countries, 90% of the population risk of a first myocardial infarction was accounted for by 9 factors: tobacco use, dyslipidemia, hypertension, diabetes, abdominal obesity, psychosocial factors, daily fruit and vegetable consumption, regular consumption of small amounts of alcohol, and regular physical activity (the last 3 being protective factors).29
During the last few years, different multivariate models have been developed to estimate 10-year cardiovascular risk in asymptomatic and apparently healthy individuals. A common feature of all these models is that most of the risk factors are not dichotomic, but rather provide a graduated risk according to their value. This is not the case with metabolic syndrome.
The Framingham30 and REGICOR (Registre Gironí del Cor)31,32 tables estimate the 10-year risk of developing coronary artery disease (regardless of whether the outcome is death), whereas the SCORE (Systematic Coronary Risk Evaluation) tables estimate the 10-year risk of death from any cardiovascular cause (including cerebrovascular accident).33 The SCORE tables are recommended by the Spanish Interdisciplinary Committee for Cardiovascular Prevention (CEIPC). Different tables are available for low- and high-risk populations. In contrast, the REGICOR tables have been chosen as the reference tables by the health services of several Spanish autonomous communities, as they have been validated in the Spanish population.
In most of the studies performed (of a case–control design), psoriasis patients had a statistically significant increase in total cholesterol, LDL cholesterol, and triglycerides compared to controls without psoriasis. In addition, a decrease in serum high-density lipoprotein (HDL) cholesterol has been observed in patients with psoriasis. HDL is a fundamental factor in inverse cholesterol transport, and exerts an anti-inflammatory, antithrombotic, antioxidant, and fibrinolytic effect.34,35 There is therefore an inverse relationship between HDL levels and the development of arteriosclerosis.
In addition, it should be remembered that certain drugs (such as ciclosporin and acitretin) used in the treatment of psoriasis could be partly responsible for changes in the lipid profile. TNF-α inhibitors can induce triglyceride elevations, but they would have beneficial effects on HDL levels.36
Different studies have shown that tobacco use is an independent risk factor for developing psoriasis, and that there is an association with more severe forms of psoriasis and poorer response to treatment.37 The association is particularly strong in the case of pustular psoriasis.26
In contrast, the association between psoriasis and hypertension is debatable, as the studies have offered contradictory results albeit with a majority pointing to such an association,4,38,39 and even an association with more severe hypertension.40
Application for Calculating the BMI, Metabolic Syndrome, and Cardiovascular RiskIn view of the results presented above, the role of dermatologists in screening for metabolic syndrome and cardiovascular risk in patients with psoriasis is decisive.41 But in practice, few dermatologists spend any time during a visit on determining these indicators of cardiovascular health. Calculation of the BMI is a tedious process, the cutoff levels for metabolic syndrome depend on the sex of the individual, and the REGICOR tables are somewhat complicated for someone not accustomed to using them regularly.
Therefore, at the dermatology department at the Hospital Son Llàtzer, Spain, we have automated the diagnosis of metabolic syndrome by integrating its assessment into the electronic medical records and obtaining the data through smart forms. These can retrieve the clinical and laboratory data of the patients so that we only have to enter waist circumference and blood pressure. The results can subsequently be exported to a spreadsheet.
However, this tool only represents a local solution. In order to help other dermatologists to detect patients with greater cardiovascular risk, we developed a multiplatform application that allows all these calculations to be done simply and intuitively. The project had the backing of the Psoriasis Group of the Spanish Academy for Dermatology and Venereology (AEDV) and funding from Laboratorios Janssen. Our development partner was the company EC-Europe. Versions were produced for the iOS operating system (for iPhone, iPd Touch and iPAD terminals) (Fig. 1) and Android, and an integrated web tool was made available on the webpage of the Psoriasis Group of the AEDV. The applications for all these platforms can be downloaded for free. Table 3 shows the web addresses for accessing the different versions of the tool, which is divided into 3 parts:
- -
BMI calculator (Fig. 2). On entering the patient's weight and height, BMI is calculated in kg/m2 and classified into normal weight, overweight (grades I and II), or obese (grades I-IV).
- -
Metabolic syndrome calculator (Fig. 3). According to the definition of the ATP-III. Sex, waist circumference, HDL cholesterol, blood pressure, and fasting glucose are entered. The screen displays abnormal parameters in red, and metabolic syndrome is diagnosed when 3 or more positive criteria are present.
- -
Cardiovascular risk calculator (Fig. 4). The application uses the REGICOR tables (validated in the Spanish population), which calculate the 10-year risk of experiencing a coronary event (whether or not the outcome is death). The parameters of sex, blood pressure, and HDL cholesterol are preloaded from previous entries for calculating metabolic syndrome. We therefore only have to enter age, diabetes, tobacco use, total cholesterol, LDL cholesterol, and family history of premature cardiovascular death. In addition to the corresponding risks, we can access a list of therapeutic goals for each case.
Links to the Different Versions of the Application.
| System | Version | Internet Address |
| iPhone, iPod Touch | http://itunes.apple.com/es/app/calculadora-para-sindrome/id445852426?mt=8 | |
| iPad | http://itunes.apple.com/es/app/calculadora-para-sindrome/id445872017?mt=8 | |
| Android | https://market.android.com/details?id=com.ec_europe.calculadoramedica&feature=search_result | |
| AEDV Psoriasis Group Website | http://www.aedv.es/grupo_psoriasis/ |
The results can be sent by e-mail, either to the patients themselves or to ourselves for printing or incorporation into the electronic medical records if available.
The aim of this tool is not to label patients as ill when they are not, but rather to identify those with a high cardiovascular risk who would not otherwise visit their physician. It can also act as a stimulus for fundamental lifestyle changes related to changes in smoking habit, improving diet, and doing more physical exercise.
FundingThe project was developed in partnership with EC-Europe, with funding from Laboratorios Janssen. The author did not receive any fees for the design of the application.
Conflicts of InterestThe author declares no conflicts of interest.
Please cite this article as: Taberner R. Calculadora multiplataforma para síndrome metabólico y riesgo cardiovascular en pacientes con psoriasis. Actas Dermosifiliogr. 2012;103:111–9.