UV radiation is the main etiological agent of skin cancer. Other factors such as pollution, diet and lifestyle are also contributing factors. Our aim was to investigate the association between melanoma and exposome factors in the Spanish population with a prospective multicenter case–control study. Case group included patients with melanoma while the control group included people who attended the consultations as companions without a past medical history of skin cancer. A total of 73 melanoma patients and 126 controls were included. The former group included more outdoor workers, a history of skin cancer, drug use (acetylsalicylic acid, antidepressants and ACE inhibitors, p<0.05), more sun exposure (p<0.001) and more sunburns (p=0.04). Controls used shade (p=0.04) or clothing (p<0.001) and the sun protection factor (SPF) used 15 years earlier was higher (p=0.04). Melanoma-related exposome factors are associated with sun exposure, drug intake and food. Prevention strategies should target specific populations, such as outdoor workers by promoting sun-safe behaviors and healthy lifestyle habits since childhood.
La radiación ultravioleta es el principal agente etiológico del cáncer de piel. Otros factores como la contaminación, la dieta y el estilo de vida también pueden contribuir. Nuestro objetivo fue investigar la asociación del melanoma y los factores del exposoma en la población española con un estudio prospectivo de casos y controles multicéntrico. Se incluyeron 73 pacientes con melanoma y 126 controles. El grupo melanoma tenía más trabajadores al aire libre, antecedentes de cáncer de piel, consumo de fármacos (ácido acetilsalicílico, antidepresivos e IECA, p<0,05), estaba más expuesto al sol (p<0,001) y sufría más quemaduras (p=0,04). Los controles utilizaron la sombra (p=0,04) o la ropa (p<0,001) y el factor de protección solar (FPS) utilizado 15 años antes fue mayor (p=0,04). Los factores del exposoma asociados a melanoma están relacionados con la exposición solar, la toma de fármacos y los alimentos. Las estrategias de prevención deberían dirigirse a poblaciones específicas, como trabajadores al aire libre, promoviendo conductas seguras frente al sol, además de estilos de vida saludables desde la infancia.
The concept of the exposome refers to all environmental exposures and represents a new approach to studying the role of the environment in human health.1 The incidence of skin cancer has increased over the past 20 years, and an exponential rise of nearly 100% is expected within the next 20 years, leading to epidemic levels of prevalence.2 In Spain, the crude incidence rates of melanoma were 8.8 cases per 100,000 person-years in 2015,3 rising to an estimated 13.1 new cases in 2020.4
Ultraviolet radiation (UVR) has been recognized as the primary etiological agent of skin cancer.5 However, there is growing evidence that environmental pollution and contaminants in water, food, or lifestyle may also play a role. On the other hand, from a holistic health perspective, it is increasingly necessary to consider the influence of stress or sleep on the development of cancer.
The objective of this study was to analyze the association between melanoma and exposome variables related to sun exposure, diet, pollution, stress, and lifestyle in the Spanish population.
Participants and methods (Supplementary data S1)A multicenter case–control study conducted by 13 dermatologists from different hospitals in Spain from April 1st, 2020 to August 31st, 2022. The case group consisted of patients diagnosed with melanoma, while the control group included individuals without a past medical history of skin cancer who attended consultations as companions.
Data were collected on age, sex, marital status, income, height, weight, place of residence, occupation, phenotype, phototype, chronic medication, sun exposure, sun protection habits, diet, exposure to pollution, toxic substances, ionizing radiation, stress, hours of exercise, and hours of sleep. Statistical significance was set at p<0.05.
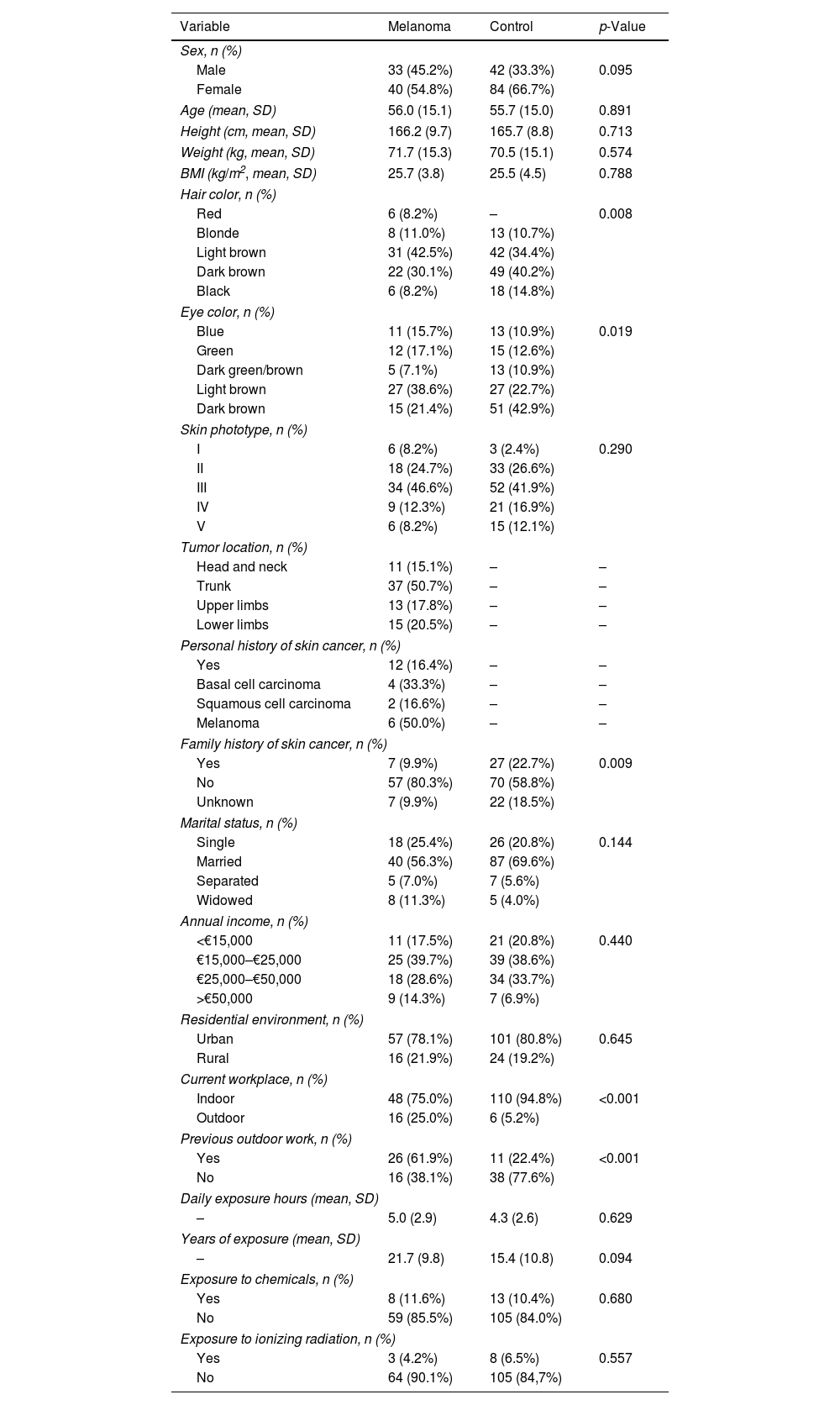
ResultsStudy population, tumor characteristics, and demographics (Table 1)The study included a total of 73 melanoma patients (54.8%, women; mean age, 56 years [SD 15.1]) and 126 controls (66.7%, women; mean age, 55.7 years [SD 15]). The melanoma group had lighter eye and hair color (p<0.001, p=0.01, respectively), but there were no differences in phototype.
Sociodemographic characteristics of the population.
| Variable | Melanoma | Control | p-Value |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 33 (45.2%) | 42 (33.3%) | 0.095 |
| Female | 40 (54.8%) | 84 (66.7%) | |
| Age (mean, SD) | 56.0 (15.1) | 55.7 (15.0) | 0.891 |
| Height (cm, mean, SD) | 166.2 (9.7) | 165.7 (8.8) | 0.713 |
| Weight (kg, mean, SD) | 71.7 (15.3) | 70.5 (15.1) | 0.574 |
| BMI (kg/m2, mean, SD) | 25.7 (3.8) | 25.5 (4.5) | 0.788 |
| Hair color, n (%) | |||
| Red | 6 (8.2%) | – | 0.008 |
| Blonde | 8 (11.0%) | 13 (10.7%) | |
| Light brown | 31 (42.5%) | 42 (34.4%) | |
| Dark brown | 22 (30.1%) | 49 (40.2%) | |
| Black | 6 (8.2%) | 18 (14.8%) | |
| Eye color, n (%) | |||
| Blue | 11 (15.7%) | 13 (10.9%) | 0.019 |
| Green | 12 (17.1%) | 15 (12.6%) | |
| Dark green/brown | 5 (7.1%) | 13 (10.9%) | |
| Light brown | 27 (38.6%) | 27 (22.7%) | |
| Dark brown | 15 (21.4%) | 51 (42.9%) | |
| Skin phototype, n (%) | |||
| I | 6 (8.2%) | 3 (2.4%) | 0.290 |
| II | 18 (24.7%) | 33 (26.6%) | |
| III | 34 (46.6%) | 52 (41.9%) | |
| IV | 9 (12.3%) | 21 (16.9%) | |
| V | 6 (8.2%) | 15 (12.1%) | |
| Tumor location, n (%) | |||
| Head and neck | 11 (15.1%) | – | – |
| Trunk | 37 (50.7%) | – | – |
| Upper limbs | 13 (17.8%) | – | – |
| Lower limbs | 15 (20.5%) | – | – |
| Personal history of skin cancer, n (%) | |||
| Yes | 12 (16.4%) | – | – |
| Basal cell carcinoma | 4 (33.3%) | – | – |
| Squamous cell carcinoma | 2 (16.6%) | – | – |
| Melanoma | 6 (50.0%) | – | – |
| Family history of skin cancer, n (%) | |||
| Yes | 7 (9.9%) | 27 (22.7%) | 0.009 |
| No | 57 (80.3%) | 70 (58.8%) | |
| Unknown | 7 (9.9%) | 22 (18.5%) | |
| Marital status, n (%) | |||
| Single | 18 (25.4%) | 26 (20.8%) | 0.144 |
| Married | 40 (56.3%) | 87 (69.6%) | |
| Separated | 5 (7.0%) | 7 (5.6%) | |
| Widowed | 8 (11.3%) | 5 (4.0%) | |
| Annual income, n (%) | |||
| <€15,000 | 11 (17.5%) | 21 (20.8%) | 0.440 |
| €15,000–€25,000 | 25 (39.7%) | 39 (38.6%) | |
| €25,000–€50,000 | 18 (28.6%) | 34 (33.7%) | |
| >€50,000 | 9 (14.3%) | 7 (6.9%) | |
| Residential environment, n (%) | |||
| Urban | 57 (78.1%) | 101 (80.8%) | 0.645 |
| Rural | 16 (21.9%) | 24 (19.2%) | |
| Current workplace, n (%) | |||
| Indoor | 48 (75.0%) | 110 (94.8%) | <0.001 |
| Outdoor | 16 (25.0%) | 6 (5.2%) | |
| Previous outdoor work, n (%) | |||
| Yes | 26 (61.9%) | 11 (22.4%) | <0.001 |
| No | 16 (38.1%) | 38 (77.6%) | |
| Daily exposure hours (mean, SD) | |||
| – | 5.0 (2.9) | 4.3 (2.6) | 0.629 |
| Years of exposure (mean, SD) | |||
| – | 21.7 (9.8) | 15.4 (10.8) | 0.094 |
| Exposure to chemicals, n (%) | |||
| Yes | 8 (11.6%) | 13 (10.4%) | 0.680 |
| No | 59 (85.5%) | 105 (84.0%) | |
| Exposure to ionizing radiation, n (%) | |||
| Yes | 3 (4.2%) | 8 (6.5%) | 0.557 |
| No | 64 (90.1%) | 105 (84,7%) | |
SD: standard deviation; BMI: body mass index; N: number of subjects.
A total of 16.4% had a personal history of skin cancer (50%, melanoma; 33.3%, basal cell carcinoma; 16.6%, squamous cell carcinoma).
Differences were observed in workplace settings (p<0.001); a total of 25% of the melanoma group worked outdoors vs 5.2% of controls.
Chronic medicationA higher percentage of melanoma patients used acetylsalicylic acid (7.5% vs 0.9%; p=0.01), antidepressants or hypnotics (17.9% vs 7%; p=0.02), and angiotensin-converting enzyme inhibitors (ACEIs) (19.4% vs 6.1%; p=0.005) (Table 1 of the supplementary data).
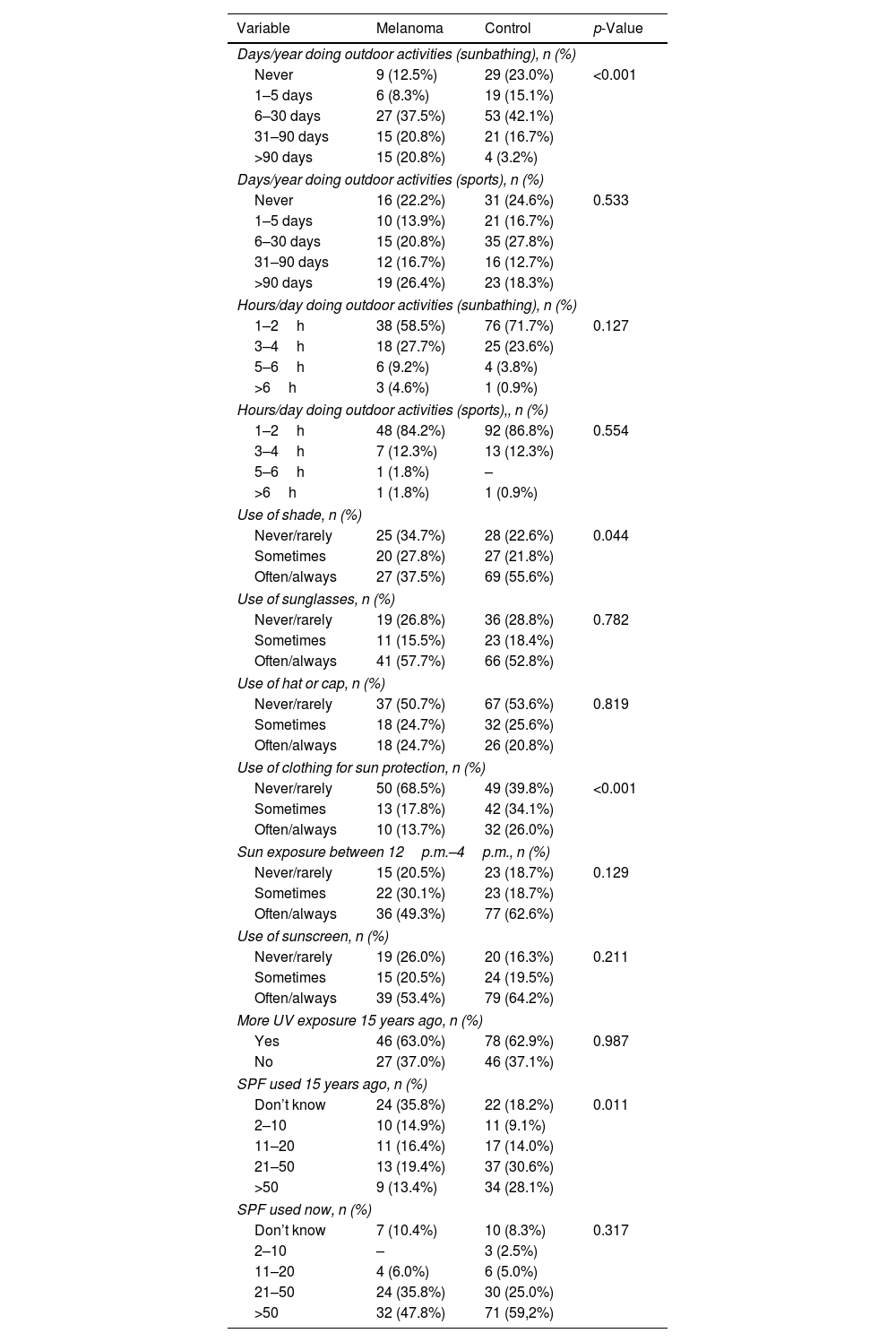
Sun exposure habits and practices (Table 2)Differences were observed in the number of days spent sunbathing per year (p<0.001); 20.8% of the melanoma group sunbathed more than 90 days per year vs 3.2% of controls.
Habits of sun exposure.
| Variable | Melanoma | Control | p-Value |
|---|---|---|---|
| Days/year doing outdoor activities (sunbathing), n (%) | |||
| Never | 9 (12.5%) | 29 (23.0%) | <0.001 |
| 1–5 days | 6 (8.3%) | 19 (15.1%) | |
| 6–30 days | 27 (37.5%) | 53 (42.1%) | |
| 31–90 days | 15 (20.8%) | 21 (16.7%) | |
| >90 days | 15 (20.8%) | 4 (3.2%) | |
| Days/year doing outdoor activities (sports), n (%) | |||
| Never | 16 (22.2%) | 31 (24.6%) | 0.533 |
| 1–5 days | 10 (13.9%) | 21 (16.7%) | |
| 6–30 days | 15 (20.8%) | 35 (27.8%) | |
| 31–90 days | 12 (16.7%) | 16 (12.7%) | |
| >90 days | 19 (26.4%) | 23 (18.3%) | |
| Hours/day doing outdoor activities (sunbathing), n (%) | |||
| 1–2h | 38 (58.5%) | 76 (71.7%) | 0.127 |
| 3–4h | 18 (27.7%) | 25 (23.6%) | |
| 5–6h | 6 (9.2%) | 4 (3.8%) | |
| >6h | 3 (4.6%) | 1 (0.9%) | |
| Hours/day doing outdoor activities (sports),, n (%) | |||
| 1–2h | 48 (84.2%) | 92 (86.8%) | 0.554 |
| 3–4h | 7 (12.3%) | 13 (12.3%) | |
| 5–6h | 1 (1.8%) | – | |
| >6h | 1 (1.8%) | 1 (0.9%) | |
| Use of shade, n (%) | |||
| Never/rarely | 25 (34.7%) | 28 (22.6%) | 0.044 |
| Sometimes | 20 (27.8%) | 27 (21.8%) | |
| Often/always | 27 (37.5%) | 69 (55.6%) | |
| Use of sunglasses, n (%) | |||
| Never/rarely | 19 (26.8%) | 36 (28.8%) | 0.782 |
| Sometimes | 11 (15.5%) | 23 (18.4%) | |
| Often/always | 41 (57.7%) | 66 (52.8%) | |
| Use of hat or cap, n (%) | |||
| Never/rarely | 37 (50.7%) | 67 (53.6%) | 0.819 |
| Sometimes | 18 (24.7%) | 32 (25.6%) | |
| Often/always | 18 (24.7%) | 26 (20.8%) | |
| Use of clothing for sun protection, n (%) | |||
| Never/rarely | 50 (68.5%) | 49 (39.8%) | <0.001 |
| Sometimes | 13 (17.8%) | 42 (34.1%) | |
| Often/always | 10 (13.7%) | 32 (26.0%) | |
| Sun exposure between 12p.m.–4p.m., n (%) | |||
| Never/rarely | 15 (20.5%) | 23 (18.7%) | 0.129 |
| Sometimes | 22 (30.1%) | 23 (18.7%) | |
| Often/always | 36 (49.3%) | 77 (62.6%) | |
| Use of sunscreen, n (%) | |||
| Never/rarely | 19 (26.0%) | 20 (16.3%) | 0.211 |
| Sometimes | 15 (20.5%) | 24 (19.5%) | |
| Often/always | 39 (53.4%) | 79 (64.2%) | |
| More UV exposure 15 years ago, n (%) | |||
| Yes | 46 (63.0%) | 78 (62.9%) | 0.987 |
| No | 27 (37.0%) | 46 (37.1%) | |
| SPF used 15 years ago, n (%) | |||
| Don’t know | 24 (35.8%) | 22 (18.2%) | 0.011 |
| 2–10 | 10 (14.9%) | 11 (9.1%) | |
| 11–20 | 11 (16.4%) | 17 (14.0%) | |
| 21–50 | 13 (19.4%) | 37 (30.6%) | |
| >50 | 9 (13.4%) | 34 (28.1%) | |
| SPF used now, n (%) | |||
| Don’t know | 7 (10.4%) | 10 (8.3%) | 0.317 |
| 2–10 | – | 3 (2.5%) | |
| 11–20 | 4 (6.0%) | 6 (5.0%) | |
| 21–50 | 24 (35.8%) | 30 (25.0%) | |
| >50 | 32 (47.8%) | 71 (59,2%) | |
SPF: sun protection factor; N: number of subjects.
Sunglasses were the most common sun protection measure used by the melanoma group, followed by sunscreen use (57.7% and 53.4%, respectively), while for the control group, sunscreen use was most common, followed by avoiding peak UVR hours (64.2% and 62.6%, respectively). Differences were observed in the use of shade as a sun protection measure (37.5% in melanoma vs. 55.6% in controls, p=0.044) and in the use of clothing, the least used measure in both groups (13.7% in melanoma vs. 26% in controls, p<0.001).
Most participants were more exposed to UVR 15 years prior (63% in melanoma and 62.9% in controls), and differences were observed in the SPF used (p=0.001).
Most controls used SPF 21–49 (30.6%) and SPF>50 (28.1%) vs the melanoma group (SPF 21–49, 19.4% and SPF>50, 13.4%). Currently, both cases and controls used, at least, SPF 21–49, with most using SPF>50 (47.8% cases and 59.2% controls).
DietThe intake of 59 dietary components was calculated using the PREDIMED questionnaire (Table 2 of the supplementary data). Egg consumption was the only variable significantly associated with melanoma. Melanoma patients had a higher egg intake than controls (3.03 vs. 2.75eggs/week; p=0.04).
Lifestyle and stress (Table 3 of the supplementary data)The melanoma group engaged in more weekly hours of exercise (7.7 [6.3] vs. 5.5 [3]; p=0.01), smoked more cigarettes per day (13.20 [5.2] vs. 8.86 [4.2]; p=0.03), and had more sunburns in the past year; nearly 16% had 2 or more sunburns vs 7% of controls (p=0.04).
Multivariate analysis (Table 4 of the supplementary data)Variables for which the statistical association remained in the multivariate analysis included genetic factors such as hair color (p=0.005) and sun exposure-related factors (workplace p<0.001). Screen time was identified as a protective factor (p=0.03). Finally, chronic treatment with drugs such as acetylsalicylic acid (p=0.01), antidepressants (p=0.02), and ACEIS (p=0.005) were identified as risk factors.
DiscussionThe present exposome analysis in melanoma patients corroborates the role of UVR-related variables, specifically chronic occupational sun exposure and past sun protection habits, especially in individuals with light hair and eye color. Meanwhile, screen time, as a potential marker of indoor activity, acted as a protective factor. Some systemic factors, such as exposure to drugs like acetylsalicylic acid, antidepressants, and ACEIs, as well as certain foods like eggs, and smoking habits, were also associated with melanoma development.
The characteristics of our sample patients are similar to previous reports. Melanoma appears to be more frequent in skin phototypes I and II and is associated with light eye and hair color and freckles.6,7
The melanoma group worked outdoors more than controls. In recent years, interest in occupational UVR exposure has increased, and several studies have reported a higher risk of non-melanoma skin cancer in outdoor workers.8
Exposure, particularly in the workplace, to substances such as pesticides increases the risk of melanoma.9 However, other chemicals and ionizing radiation were not found to be statistically associated occupational risk factors after adjusting for known risk factors, such as nevus count and sun exposure, as observed in our study.10
Although some studies confirm the association between acetylsalicylic acid consumption and melanoma development, as in our sample, others suggest it reduces melanoma risk.11 Antidepressant use was associated with a higher risk of melanoma. Vries et al.12 conducted a comprehensive European study finding that stress, traumatic events, and depression were associated with an increased risk of melanoma. Although ACEIs have been associated with a higher risk of non-melanoma skin cancer due to photoinduced reactions,13 they have not been shown to increase melanoma risk.14
Differences in sun protection measures were observed between groups, with controls using them more frequently. Soto et al.15 compared sun protection behaviors of patients before and after melanoma diagnosis, finding that melanoma patients used fewer sun protection measures before diagnosis, with clothing being one of the least used measures.
Regarding sun protection 15 years prior, most respondents reported using lower SPF sunscreens less frequently, possibly due to poorer awareness of sun damage and its implications. However, controls used higher SPF sunscreens than melanoma patients, supporting the importance of unprotected sun exposure in melanoma development. Additionally, the higher number of sunburns in the melanoma group in the past year supports the relationship between sporadic, intense sun exposure and melanoma.16
Of the 59 dietary components, only egg consumption was associated with melanoma. One study concluded that higher egg consumption confers greater risks of all-cause mortality, cardiovascular disease, and cancer in a non-linear dose–response pattern.17 Conversely, Malagoli et al.18 found an inverse correlation between melanoma risk and the consumption of legumes, olive oil, and eggs.
In the multivariate analysis, screen time, associated with indoor activity, turned out to be a protective factor, supporting the importance of outdoor exposure in melanoma development. Additionally, the melanoma group engaged in more weekly hours of exercise. Many studies have reported higher levels of UVR exposure and, consequently, a higher risk of skin cancer among athletes who practice outdoor sports.19
Finally, regarding smoking habits, although smoking-related skin changes have been described, smoking per se has not been proven to be an independent risk factor for melanoma.20
A limitation of this study is its sample size, and since controls were companions, they may have introduced bias by sharing common exposures with cases. The main strength is the simultaneous evaluation of the association between melanoma and all possible exposome factors.
ConclusionsThis analysis confirms that sun exposure, particularly occupational exposure and sunburns, is the exposome variable most strongly associated with melanoma, especially in individuals with light skin and eyes. Insufficient sun protection in the past is a significant risk factor, as is chronic consumption of certain drugs. Specific actions are needed, particularly for outdoor workers, but also for children and individuals engaging in outdoor sports and leisure activities, promoting safe sun behaviors.
Ethics committee approvalReviewed and approved by the Aragón CEIC; approval C.I. PI19/311.
FundingNone declared.
Conflicts of interestNone declared.
To Vichy Laboratories for their support.