Although alopecia areata (AA) is a common autoimmune alopecia, its most severe forms (alopecia areata totalis (AAT) and alopecia areata universalis (AAU)) are a therapeutic challenge given the need to use systemic treatment such as corticosteroids, methotrexate, azathioprine or the recent JAK inhibitors to control the disease.1
Recent publications have highlighted the possible relationship between alopecia areata and the gut microbiome, detecting differences in the gut bacterial biodiversity of AA patients compared with controls2 and improvement of their disease after faecal microbiota transplant.3 In addition, during alopecia areata flare-ups there is a decrease in the population of circulating regulatory T lymphocytes (Tregs).1 Peripheral maturation of Tregs directly involves the intestinal microbiome, enterocytes and short-chain fatty acids (SCFA) such as butyrate.4,5 These SCFA are organic acids mainly produced by colonic gut bacteria via fermentation of dietary fibre, resistant starches, and proteins. Although SCFA are involved in the correct homeostasis of human gut and its healthy relationship with local resident microbiome, butyric acid has pleiotropic immunomodulatory effects including histone deacetylase (HDAC) inhibition of gut and immune cells or downregulation of the NF-κB signalling pathway which results in an anti-inflammatory effect.6
Twenty patients with a clinical diagnosis of AAT and AAU were recruited. Exclusion criteria were age<18 years, pregnancy, use of any topical or systemic medication in the last 24 weeks, coeliac disease, a recent (less than 1 year) or old diagnosis (more than 10 years) of AA. Local ethics committee approval was not needed as the study consisted in a dietary recommendation. Patients were instructed to follow a modified Mediterranean diet with anti-inflammatory characteristics (Table 1) with added daily oral butyrate in the form of 900mg microencapsulated tributyrin (Butycaps®) with the aim of analysing if it had any effectiveness in improving alopecia areata (decrease in SALT score) and BMI in patients with AAT and AAU after 6 months of diet.
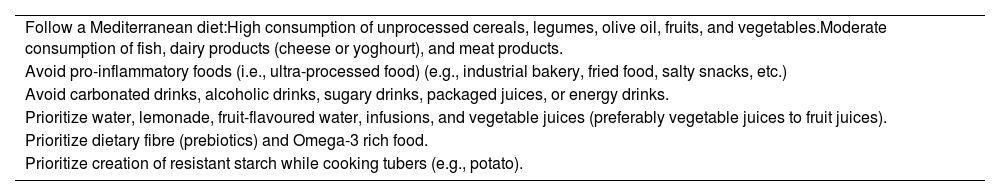
Anti-inflammatory diet guidelines.
| Follow a Mediterranean diet:High consumption of unprocessed cereals, legumes, olive oil, fruits, and vegetables.Moderate consumption of fish, dairy products (cheese or yoghourt), and meat products. |
| Avoid pro-inflammatory foods (i.e., ultra-processed food) (e.g., industrial bakery, fried food, salty snacks, etc.) |
| Avoid carbonated drinks, alcoholic drinks, sugary drinks, packaged juices, or energy drinks. |
| Prioritize water, lemonade, fruit-flavoured water, infusions, and vegetable juices (preferably vegetable juices to fruit juices). |
| Prioritize dietary fibre (prebiotics) and Omega-3 rich food. |
| Prioritize creation of resistant starch while cooking tubers (e.g., potato). |
In total, 20 patients diagnosed with AAT or AUU (SALT score of 100) followed the study diet for a minimum of 6 months (range 6–25 months) with a follow-up period of 12 months (range 12–30 months). Mean age of patients was 37.6 years (range 21–63 years). Sixty percent of the patients were female.
After 6 months of diet, one patient showed mild improvement (SALT 90) of her disease. Globally, there was a significant decrease in weight (74.3kg vs. 71.4kg, p=0.05) and statistical trend towards body mass index (BMI) improvement (26.9kg/m2 vs. 25.4kg/m2). The diet was easily tolerable and 25% of the patients maintained it after 12 months even if there was no SALT improvement.
Although the role of a gluten-free diet as an adjuvant treatment for AA has been studied in the past with inconclusive results7; to date, the impact of an anti-inflammatory diet in patients with AA without celiac disease had not been investigated. Our data suggest that a dietary intervention does not seem to have significant clinical effectiveness in patients with advanced alopecia areata, despite hypothetically acting on its etiopathogenesis. This result is not unexpected as the management of AAU/AAT is notoriously complex due to its high risk of recurrence, probably due to the existence resident memory T cells in the patients’ skin. In addition, it is known that changes in diet or the use of prebiotics, probiotics, symbiotics or antibiotics have a fundamentally transitory effect on the gut microbiota, as it has a very low plasticity and tends to return to its basal state after the end of the intervention. In spite of this, faecal transplant is the only intervention that has been shown to modify the intestinal microbiota in the long term and should be further explored in alopecia areata.8
Nevertheless, as there is rising evidence that patients affected by AA may be subjected to an increased cardiovascular risk1 due to a hypothetical increased systemic inflammatory status, these patients could benefit from a healthy diet to decrease their weight and improve cardiovascular function.
Conflict of interestsThe authors declare that they have no conflict of interest.