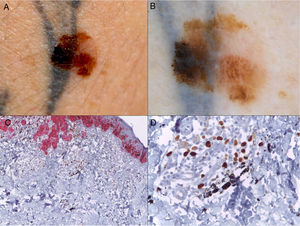
A 35-year-old man came to the clinic after noticing changes in a pigmented lesion on his right arm, where he had had a tattoo some 2 years previously. When the tattoo was placed, the tattooist avoided a pre-existing nevus, although during recent months this had grown until it reached the tattoo and came to the patient's attention (Fig. 1 A and B). Clinical suspicion led us to remove the lesion. Histopathology showed it to be a superficial melanoma (Breslow depth, 0.35mm) that had developed from a dysplastic nevus (Fig 1 C and D).
A, Melanoma over a recent tattoo on the right arm. B, Dermoscopic image showing striking asymmetry of colors and structures and highlighting the presence of an atypical pigment network, pseudopods, and irregularly distributed globules and spots. C, Histopathology based on HMB45-Ki67 immunohistochemistry showing the presence of nests of neoplastic cells in the dermis (red), as well as black granules of tattoo ink inside macrophages and free in the dermis (HMB45-Ki67, original magnification ×4). D, Detail of the black granules of tattoo ink (HMB45-Ki67, original magnification ×40).
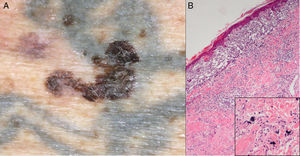
Another patient (82 years) was referred by his family doctor with a suspected melanoma, which took the form of a pigmented lesion on a tattoo on the left arm that was observed during an examination for other reasons. The tattoo was more than 60 years old and the patient had not noticed the lesion for which he was referred, namely, an asymmetrical pigmented macule with irregular borders and various colors, with areas suggestive of regression (Fig. 2 A). Histopathology confirmed the lesion to be a superficial, partially regressing melanoma (Breslow depth, 0.4mm) with no associated lesions.
A possible pathogenic association between tattoos and melanoma has been the subject of speculation in the literature, with potential causes including local trauma, the carcinogenic potential of the ink, and even a possible increase in absorption of ultraviolet radiation.1 However, this finding is now considered a mere coincidence.1–3 In recent years, we have seen a marked increase in the popularity of permanent tattoos in Spain, especially among young people. The estimated prevalence of tattoos in Europe is 10%, which increases to 25% in adults aged 20-35 years.3 However, cases of melanoma on tattoos are still rare,2 as demonstrated by the fact that only 28 cases have been reported in the literature to date (30 counting the 2 cases reported here).1–10 Together with the lack of cases of multiple melanoma over a single tattoo, this supports the notion that the association between tattoos and melanoma is merely casual.1–3 Nevertheless, the finding of melanoma on a tattoo has several relevant implications.
On the one hand, the presence of a tattoo usually masks pigmented lesions and hampers early diagnosis of a potential melanoma on the part of both the patient and the dermatologist, thus leading to a delay in diagnosis.1–8 It is essential to raise awareness among the population in general and among tattooists in particular that a tattoo should never be placed over pre-existing pigmented lesions.1,6 Similarly, when examining a patient with tattoos, the dermatologist should pay special attention to tattooed skin in order to avoid overlooking a hidden suspicious lesion.2,8 Of note, in the first patient we report and in 2 cases in the literature,9,10 the cosmetic alteration in the tattooed image caused by the melanoma made it easy for the patient to notice it, thus making for earlier detection than if the lesion had appeared at another site. Although these cases are exceptions to what we report above, there is no doubt that if tattooists adopted the practice of leaving an area of healthy skin around pre-existing nevi, any changes these could subsequently undergo would be more easily detected.9
On the other hand, there is a risk that if a tattoo is placed on a pigmented lesion, this may already be a melanoma, and multiple metastatic deposits could be seeded during placement, as occurred in a recently published case,7 thus highlighting the importance of avoiding previously pigmented lesions. Therefore, in specific cases with a risk of melanoma (patients with atypical nevus syndrome, multiple nevi, or a family history of melanoma), the individual should undergo a dermatological assessment before having the tattoo.3
Finally, before a tattoo is eliminated by laser, the tattooed skin should be carefully examined—both clinically and dermoscopically4—to detect potentially hidden pigmented lesions and avoid applying laser therapy over the areas affected (since this can alter their characteristics and lead to subsequent diagnostic errors). Alternatively, the lesions should be removed before laser therapy if they are suspected of being melanomas. Therefore, laser removal of tattoos should only be performed by dermatologists.4
In conclusion, we present 2 new cases of melanoma on a tattoo. Although the association appears to be casual, it has several implications: the need for close attention during examination of the tattooed skin, the importance of raising awareness among tattooists and users that pigmented lesions should not be tattooed, and the importance of the fact that laser removal of a tattoo should always be performed by a dermatologist.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to Dr. Josefa San Juan and to Dr. José Ferrando from the Histopathology Department of Hospital Arnau de Vilanova, Valencia, Spain for providing us with access to the sections in the second case.
Please cite this article as: Armengot-Carbó M, Barrado-Solís N, Martínez-Lahuerta C, Gimeno-Carpio E. Melanomas sobre tatuajes: una asociación casual con implicaciones prácticas. Actas Dermosifiliogr. 2017;108:678–680.