Clinical safety and medical liability are first-order concerns in today's medical practice. It is important to understand the circumstances under which medical acts fail to live up to the accepted standard of care and to recognize the impact that malpractice claims have on physicians. Practitioners must also grasp the concept of medical error, studying malpractice claims in order to identify the areas where improvement is needed. The risk of accusations of malpractice in dermatology is comparatively low, both in Spain and worldwide. However, a great variety of clinical scenarios in dermatology can potentially give rise to a claim, and malignant melanoma is most susceptible to risk. Dermatologists should know which actions during clinical consultation merit particular attention and care. Clinical practice carries inherent risk of malpractice claims, but taking certain recommended precautions can prevent them.
La seguridad clínica y la responsabilidad profesional médica son hoy en día preocupaciones de primer orden en el ejercicio de la medicina. Interesa la valoración de las circunstancias en las que el ejercicio de la medicina no se ajusta a la lex artis, así como el impacto de las reclamaciones sobre los facultativos. Debe existir además un aprendizaje del error médico, identificando, mediante el estudio de reclamaciones, áreas específicas de mejora. La dermatología es una especialidad con bajo riesgo de reclamación a nivel internacional y también en nuestro contexto. Gran variedad de circunstancias clínicas dan lugar a reclamaciones por praxis médica en dermatología, y entre ellas destaca la actuación en caso de melanoma cutáneo maligno. Por otro lado, existen riesgos potenciales en las consultas de dermatología que merecen especial atención. El quehacer clínico está sujeto a un riesgo inherente de reclamación y por tanto son necesarias una serie de recomendaciones para prevenirlas.
The 1999 publication To Err is Human: Building a Safer Health System1 was the first to denounce preventable medical error and gain wide acceptance by the medical community.2 This monograph dealt with the full reach of error, including both harm done to patients as a result of health care and the social and economic repercussions of that harm.
In response, the World Health Organization (WHO) adopted a World Health Assembly resolution (WHA55.18) in 2002 to urge member states to “pay the closest possible attention to patient safety” and “establish and strengthen science-based systems necessary for improving patient safety and the quality of health care.” Following on this resolution, in 2004 the WHO proposed to coordinate and accelerate improvements in patient safety measures and spread news of such efforts. The World Alliance for Patient Safety was established at that time.3
Patient, or clinical, safety — understood as a set of measures to eliminate, reduce, or ameliorate adverse effects of health care processes — has earned a central position among the fundamentals of modern medical practice, at a time when evolving medical, scientific, and technological progress places physicians under constant pressure to keep up with good standards of care.4 In this context, patient safety and professional liability have become first-order concerns for medical practitioners.3
Professional liability in the exercise of medicine is defined by the physician's duty to prevent and correct voluntary and involuntary errors or negligence as well as to give satisfaction when they occur.5 These duties are incumbent upon practitioners in all specialties, and dermatology is no exception.6,7
The concept of malpractice is relevant to any discussion of professional liability. Malpractice occurs when medical acts are in breach of the accepted standard of care (termed lex artis medica in Spanish jurisprudence).8 The notion of an accepted standard, which is a legal concept rather than a medical one,9 is used synonymously with correct technique, or more precisely, medical care that is reasonable, follows protocol, or would be provided by any well trained physician under the same or similar circumstances.10,11 This ad hoc approach to a standard of medical care is the basis for evaluating the correctness of a physician's performance of a concrete medical act.12
Acts that occur during medical practice are associated with different types of professional liability according to the setting and circumstances in which they take place. Thus, liability may be decided within a criminal, civil, or administrative judicial pathway, or a claim may be handled out of court. Issues of professional or collegial ethics and obligations may also be brought to bear. In addition, 3 levels of health care liability can be identified.13 The first level is the physician's own liability. The second pertains to health care institutions or facilities with reference to their clinical organization, coordination and the chain of command. The third refers to the responsibilities of administrators who are in charge of proper health care planning and who are also obligated to provide it without increasing risk. Available research also stresses the great impact that allegations have on physicians. This research urges us to adopt measures to prevent malpractice suits and address their effects on the individual practitioner's health, which begins to suffer the moment a process begins (with a summons and charges) and continues through its subsequent stages (mediation, trial, ruling) and/or after resolution —unleashing manifestations known as the clinical-judicial syndrome in its direct translation from Spanish.14 This syndrome encompasses all the physical, psychological, and moral injuries that may occur.
We should bear in mind that the Spanish constitution recognizes the right to protection of health. Noteworthy components of this protection are the patient's fundamental right under law to make care decisions (the principle of autonomy) and the physician's duty to ensure autonomy by informing and obtaining consent, which a competent patient must give by choosing freely among the available clinical alternatives. Law 41/2002 provides the regulatory basis for patient autonomy and the rights and obligations regarding clinical information and documentation.15 This law establishes that consent can generally be given verbally but that it must be written in certain cases, which are described generically as involving “surgical procedures, invasive diagnostic and therapeutic procedures, and in general any procedures in which notable risk, discomfort or negative effects on the patient's health can be expected.”
It has been pointed out that current practices and standards for obtaining informed consent are often of little use to the patient and that they can expose the professional to unnecessary risk.16 Nonetheless, the courts have used informed consent as the appropriate standard of information.17 Since patients must receive individualized information, informed consent templates developed by experts and meant to be tailored according to individual needs have been suggested as a way to aid both patients and professionals.18 To that end, informed consent should be understood as a process rather than a specific act, and the use of templates developed by medical societies are highly recommended. One such template was developed by the Spanish Academy of Dermatology and Venereology (AEDV) for use in this specialty. Informed consent may be even more critical in cosmetic dermatology, which falls under the heading of satisfactive medicine. Voluntary or satisfactive medicine is understood to be only optional. This is to say, the interested party approaches the physician not to seek treatment for a disease but rather to improve some physical characteristic for aesthetic reasons, to effect a transformation, or to control a biologic function.19 Such contexts involve greater liability and imply that outcomes must be satisfactory.20 In other words, these situations warrant “precise rather than defective compliance with the contract.”21 The physician must therefore explain the real chances of improvement, not a hypothetical improvement that both parties desire.
It is also wise to know how to face the consequences when unexpected and involuntary medical errors occur for any reason.22 It has been postulated that accidents occur as the result of multiple factors and that even though systems to prevent them may be in place, such accidents or adverse events will happen when a series of defects line up.23 However, physicians must also learn from their errors. Specific areas of patient care under the essential standards of care must be identified by analyzing cases, including those that occur in dermatology,24 in order to guide the development of programs to improve quality of care and patient safety.25
Professional Liability in DermatologyDermatology has been shown to be at low risk for malpractice claims in other countries,6,26–28 although concern for patient safety and physician liability is growing. The settlements awarded in malpractice suits in dermatology have also been found to be much lower than those in other medical specialties.29
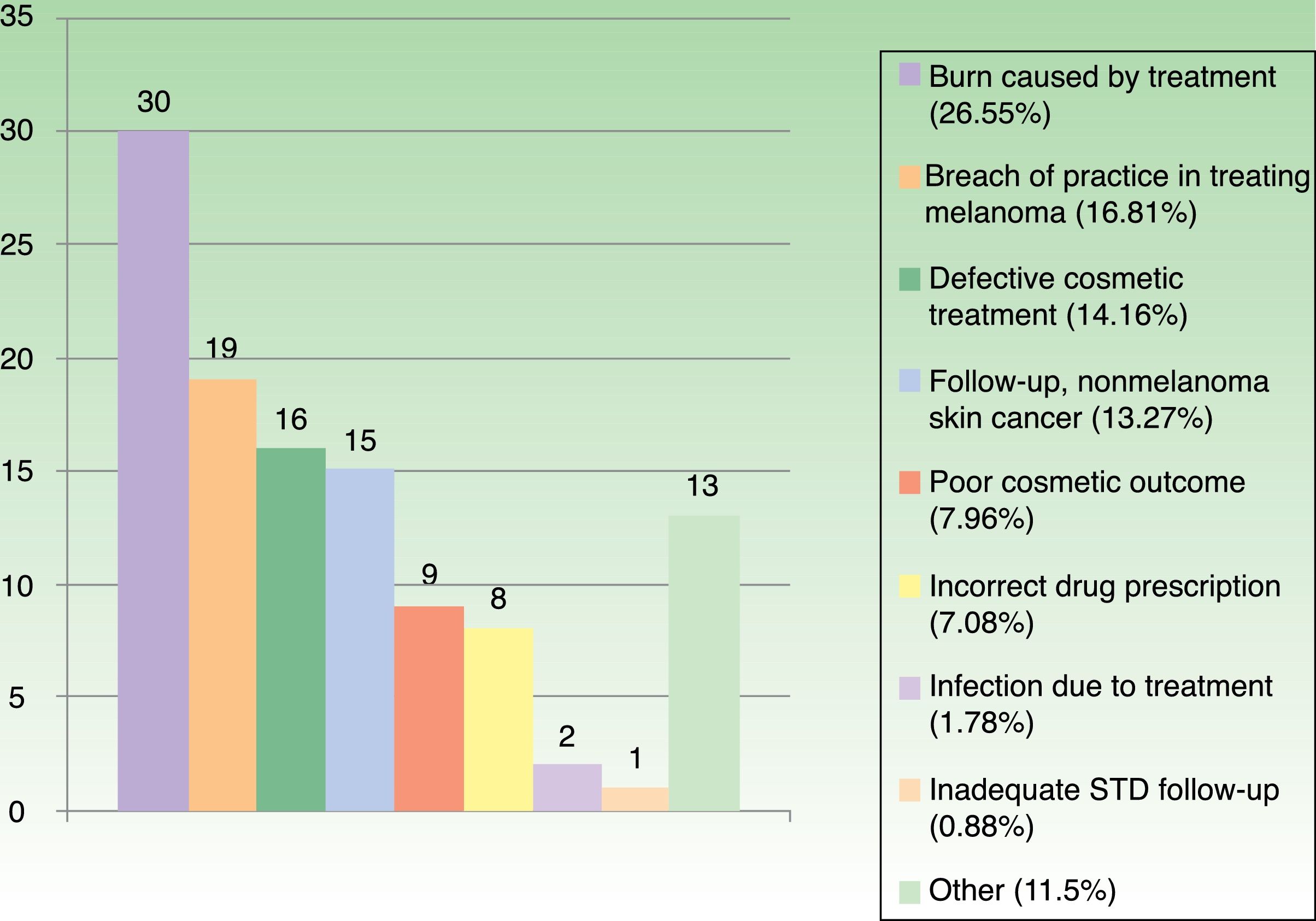
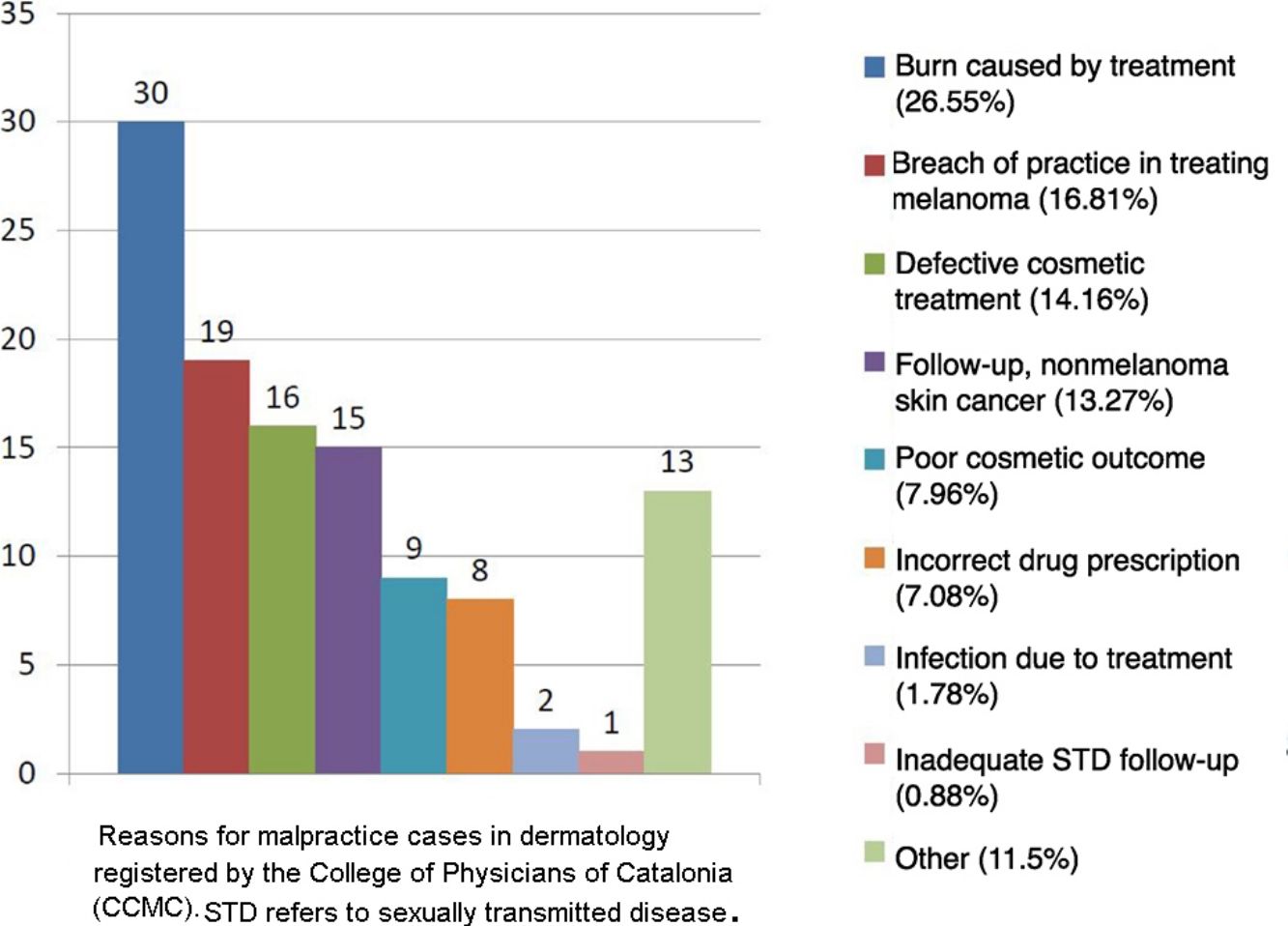
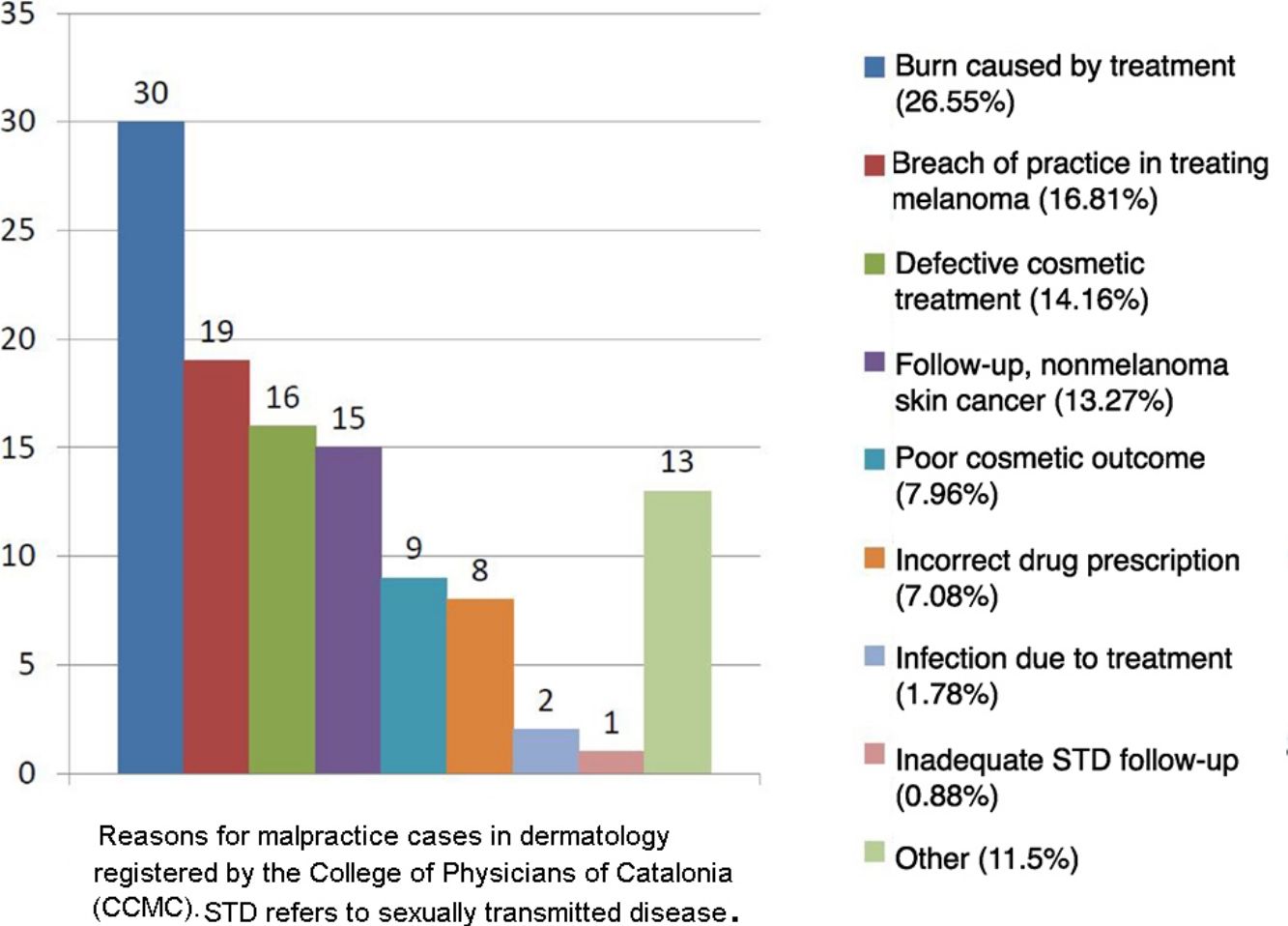
Statistics for Spain confirm those reports from abroad.30,31 The College of Physicians of Catalonia (CCMC), which coordinates all four of the medical associations in this autonomous community, established a professional liability insurance program in 1986. Under this program the insurer delegates management of a policy to the CCMC's professional liability service, which gathers clinical, judicial, and administrative data on all claims. The service registered 9115 allegations between 1986 and 2017. An average of 318 cases per year were handled in the last 10years, and the recent trend is toward fewer charges brought to bear (316 in 2016 and 273 in 2017) and for more to be settled outside court. In the same 31-year period, 113cases concerned dermatology, which therefore accounted for 1.24% of all complaints handled by the CCMC's service. The reasons for the 113cases (Fig. 1) were similar to those reported for other countries.
Medical acts performed in dermatology outpatient clinics accounted for 84 (74.34%) of the Catalan cases. Twenty-one (18.58%) were acts in operating theaters, 4(3.54%) were in an emergency department, 2(1.77%) were in primary care clinics, and 2(1.77%) were on hospital wards.
Clinical malpractice claims can arise from a wide variety of acts in dermatology. However, procedures related to cutaneous melanoma stand out as being associated with higher risk32 because of the difficulty of diagnosis even in the hands of experts.33,34
The 2 main reasons for malpractice allegations in melanoma are delayed clinical diagnosis or wrong diagnosis of lesions with similar morphologic or histologic characteristics. The histopathology of some atypical melanocytic lesions can be very difficult to interpret. The dermatopathologist must distinguish between these lesions (which accounted for 33% of all dermatology claims found in a UK study35) and a true melanoma. Over the years atypical melanocytic lesions have been given diverse classifications and various names, such as atypical melanocytic hyperplasia, atypical Spitz tumor, atypical blue nevus, deep penetrating nevus, melanocytoma, melanocytic tumor of uncertain malignant potential, and Spitzoid melanocytic tumor of uncertain malignant potential. The nomenclature will continue to shift over time, contributing to confusion and controversy.36–38
Other scenarios have given rise to dermatology malpractice claims. One example is burns occurring during phototherapy (UV-A or psoralen plus UV-A),39 which accounted for 23% of the dermatology claims identified in the aforementioned UK study.35 Another is complications during drug treatment.28 In one large US study, diagnostic error in melanoma ranked second as a cause of malpractice suits after the use of inappropriate procedures in skin surgery.27 Furthermore, courts ordered compensation in 42.2% of the cases related to melanoma.
Potential Risks in Dermatology ClinicsVarious factors, including physician gender,40 merit special attention when weighing the possibility of risk of future malpractice suits in dermatology. A full-body examination, for example, may still be problematic because some patients may feel violated and even “injured” by the examiner. However, such an examination is medically justified for a patient who has sun-damaged skin, precancerous or melanocytic lesions to be evaluated, or a history of skin cancer. To avoid full nudity, examinations can be done in stages and are best carried out in the presence of a nurse or assistant. Above all, communication with the patient is critical, as is informed consent under the situations stipulated in Law 41/2002.15
Dermatology also requires routine use of photographs. Patients who might be identifiable in clinical photographs should first give their informed consent for them. It is sometimes advisable to show the photograph to the patient so that he or she can grasp the medical interest of keeping it on record.
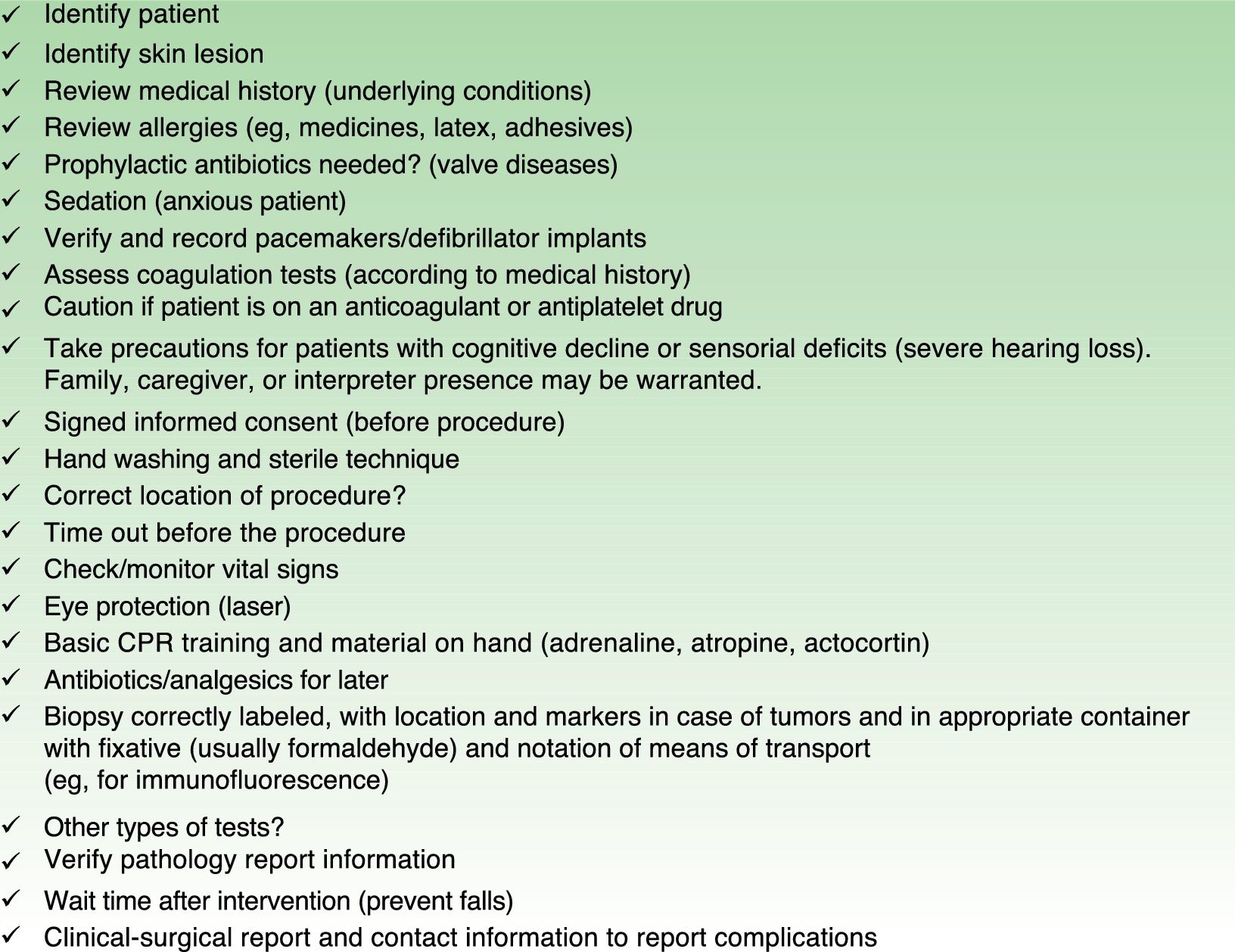
Medication is another potential source of error. Drugs associated with risk (such as methotrexate, antimalarial agents, biologics, retinoids, corticosteroids, sulfones, or propranolol) should be prescribed with extra care. Patient safety recommendations should also be followed when surgical or laser treatments are provided, and checklists to guide the physician are available. We propose a checklist for dermatologic surgery (Fig. 2), although the excellent surgical checklist of the WHO should not be undervalued.
Another concept currently of interest in Spanish jurisprudence is lost opportunity to benefit from treatment, which commonly occurs as the result of a diagnostic error or delay if a disease leads to serious lesions or death. From the point of view of professional liability, all instances of breach of care, or negligence, occur in reference to a concrete act, the one expected of the physician or the one that was the physician's duty to perform according to the standard of care.41
The use of teledermatology is supported by the AEDV provided it is an element of ongoing medical care (a medical act). However, it has been suggested that diagnosis is less certain and the rate of diagnostic error is higher when this technology is used in specialty medicine. Precautions should therefore be taken to regard teledermatology as an emergent technology that has legal issues still to be resolved42 and that should be used carefully in accordance with guidelines set by medical associations.43
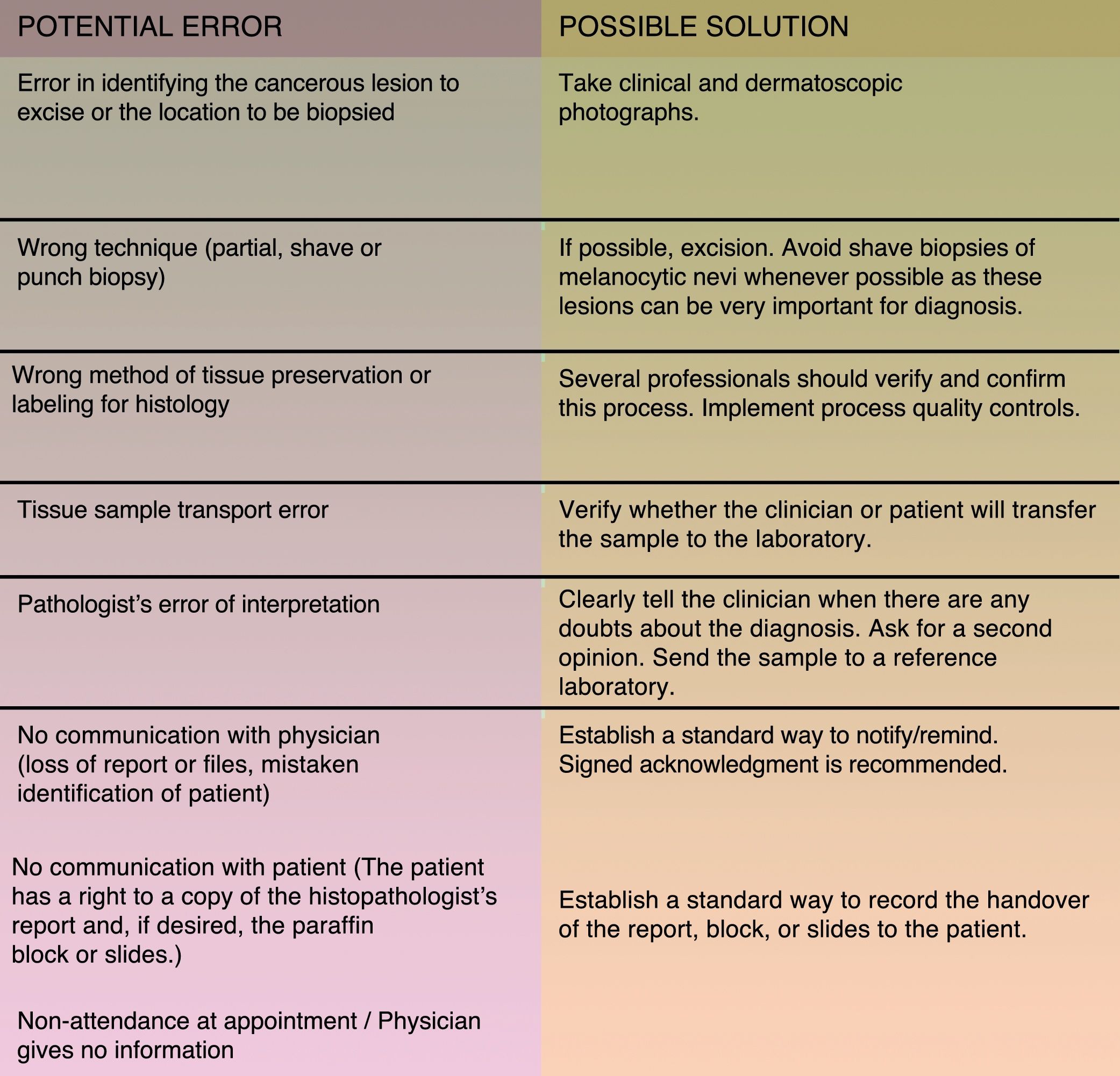
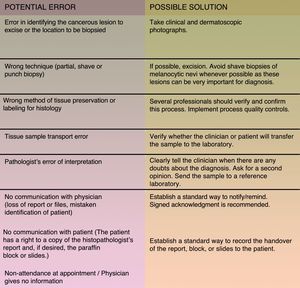
Besides the abovementioned situations 2 others stand out as involving a high level of risk of malpractice claims: cutaneous melanoma and skin biopsies. Patient safety requires that a skin biopsy sample should be reserved for histopathologic examination whenever a lesion is removed.44,45Fig. 3 shows the most common errors that can occur in this situation and their possible solutions. Surgical procedures done under local anesthesia in outpatient clinics are also of concern. A medical history is essential for detecting risk of possible adverse reactions.46
The most common potential errors involving skin biopsies and how to solve them. Source: Adapted from Hansen et al..45
Finally, we mention that many patients now research their symptoms online, so the physician must be able to manage their interpretations by clarifying notions or demonstrating that internet promises and advice are often incorrect and even contrary to what is appropriate in the patient's particular case. It should also be made clear that the patient should report any complications to the treating physician rather than follow advice found on the internet.
Special Care in Cutaneous MelanomaSetting aside Merkel cell carcinoma, which is quite rare, cutaneous melanoma is the skin cancer with the worst prognosis. It is also one that affects young persons and is the fifth most common cancer in men (6% of all cancers) and sixth most common in women (4% of all cancers).47 The prognosis has improved substantially for patients with metastatic melanoma in the past 5years thanks to targeted systemic therapies and immunotherapies that prolong survival by more than 2years on average.48 Although no prospective longitudinal studies have yet demonstrated that early diagnosis improves overall survival,49 this is not the only desired outcome. Early diagnosis by means of manual or digital dermoscopy and rapid access to proxy predictors of survival (Breslow thickness) currently help the dermatologist arrive at a faster, more accurate diagnosis and support a prognosis of stable survival, distinguishing this cancer from others.
New techniques used in the histopathologic diagnosis of melanoma and melanocytic lesions are also of great help. A melanoma diagnosis is usually based on morphology, but clinical, morphologic, and molecular data complement each other to help establish a definitive diagnosis in difficult or complex cases.50 The Breslow thickness is still the most important prognostic factor in such cases.
The incidence of melanoma has risen in recent years, and a reading of data from the CCMC's professional liability service, the main court cases, and the abundance of literature on claims related to melanoma point to this cancer being among those most frequently named in malpractice suits in Spain. This situation obliges us to try harder to apply individualized strategies to ensure patient safety in medical acts related to this disease. Efforts should be made to provide greater vigilance by using the screening methods recommended in current guidelines, raising awareness in the general population and among dermatologists alike, and encouraging the excision of any clinically or dermoscopically suspicious lesion.
Recommendations for Avoiding Malpractice Claims in DermatologyBecause there is inherent risk of malpractice claims in clinical practice, dermatologists should follow a series of recommendations for preventing them. Among them we highlight the following:
- a)
Use clinical practice guidelines to ensure that the standard of care is being followed, thereby improving safety and, of course, averting claims.
- b)
Keep complete, computerized patient records.51
- c)
Remember that consent based on personalized information must be given in writing by the patient before any surgical or invasive diagnostic procedure commences.52
- d)
Follow the required clinical pathway for skin biopsies all the way through to a final diagnosis.
- e)
Use a clinical checklist (eg, Fig. 2) before all surgical procedures in dermatology.
- f)
Prescribe the medication that carries the least risk whenever alternatives with similar indications are available. Obtain written informed consent whenever medications have potential teratogenic effects.
- g)
Cooperate with hospital risk-management services.
- h)
Discuss complex or controversial cases in clinical sessions and obtain the necessary advice of other specialists, documenting decisions made based on consensus and any disagreements that arise.
- i)
Include dermoscopy as the standard way to examine any skin lesion, whether pigmented or not.
- j)
When proposing satisfactive medical acts in cosmetic dermatology, orient information to the patient's specific case, clarifying beforehand what the real results may be.
To summarize, in any situation in which an allegation of medical malpractice arises, the best line of defense will be in keeping with the principles of patient safety.37 This approach will suppose improving surgical and procedural competence and establishing protocols45; fostering free and honest communication between patient, clinician, and pathologist; applying rigorous controls when handling tissue samples transferred from the clinic to the laboratory; integrating quality control strategies or mechanisms in histopathology laboratories; writing cautious pathologic interpretations that recognize the limitations of the art and science of our discipline; and, finally, adopting a transparent, open, and ongoing review process for clinicians.
The broad recommendations for averting allegations of malpractice in general medicine should not be overlooked in dermatology. We should avoid speaking ill of colleagues; learn from our errors (analyze risks and manage mistakes) by studying malpractice cases; and obtain training in medical–legal issues.53 We should use checklists to assure compliance with safety standards; encourage the use of examinations, procedures, and treatments that involve the least possible risk; and fully inform the patient, keeping their written consent on file. Strategies to improve patient satisfaction should also be included, given that satisfaction influences clinical outcomes and averts medical malpractice claims.54
ConclusionsThe risk of medical malpractice allegations is low in dermatology, probably because surgical risk is low, most procedures are done with local anesthetics, and most skin diseases other than cutaneous melanoma are not life threatening. Diagnostic, clinical, and histopathologic difficulties do arise in melanoma. Care must also be taken when using new approaches to clinical care (such as teledermatology) and in cosmetic dermatology, which falls under the category of satisfactive medicine. New legal concepts, such as a patient's lost opportunity to benefit from treatment, must be borne in mind. In any case, the 2 practices that yield the best results in matters of patient safety and averting malpractice claims are 1) maintaining a good relationship with the patient and significant others and 2) keeping careful records of everything related to the care process and the patient.
Rightly or wrongly, a good doctor may become involved in a malpractice suit due to his or her own medical error or a colleague's. An error may have physical, psychological, or moral effects on the physician (here termed the clinical–judicial syndrome). The case may also be brought to trial, and the physician might be struck off the register. Understanding the reasons for errors and their consequences can be of great value in preventing them. The patient safety policies in place today further that objective.55,56
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Arimany Manso J, Martin Fumadó C, Mascaró Ballester JM. La dermatología y sus aspectos médico-legales: seguridad clínica y dermatología. Actas Dermosifiliogr. 2019;110:20–27.