To the Editor:
Marjolin ulcer is an invasive neoplasm that arises from chronic wounds of any etiology, including traumatic wounds, chronic ulcers, and partial or total skin grafts.1,2 Squamous cell carcinoma, although rare, is the most frequently produced neoplasm.3 Here, we present 2 representative cases.
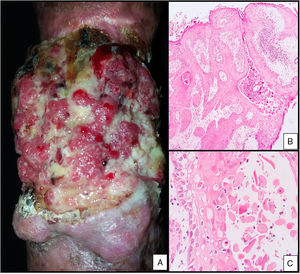
Case DescriptionsCase 1The patient was a 56-year-old man with a history of soft-tissue trauma caused by crushing of the left leg, for which he had undergone allograft reconstruction 38 years earlier. He was seen for a progressively enlarging verrucous, ulcerated lesion on the left leg that had appeared 1 year earlier (Fig. 1A). A biopsy was performed on suspicion of malignancy and revealed an infiltrating squamous cell carcinoma (Fig. 1B and C). Imaging studies showed bone infiltration, which necessitated amputation of the affected limb.
Case 2The patient was a 51-year-old man with a history of soft-tissue trauma with circumferential compromise and tissue avulsion caused by a crush injury received in a traffic accident 30 years earlier. He was seen for a progressively enlarging verrucous, ulcerated lesion, located on the scar on his right forearm that had appeared 1 year earlier (Fig. 2A). A biopsy was performed on suspicion of malignancy and revealed an infiltrating squamous cell carcinoma (Fig. 2B and C). The patient underwent chemotherapy and radiation therapy, after which tumor recurrence necessitated amputation of the affected limb.
DiscussionSquamous cell carcinoma is the second most common cutaneous neoplasm after basal cell carcinoma. This tumor type can occur de novo or can arise from precancerous lesions or from lesions caused by prior trauma.4 Tumors that arise from chronic wounds, including chronic ulcers, are known as Marjolin ulcers, and have an estimated incidence of 1.3%–2.2%, which increases with the chronicity of the pre-existing lesion.1 Development of Marjolin ulcer has been reported up to 65 years after the appearance of the initial lesion, although the mean latency is approximately 40 years.5 In our 2 cases the mean latency to lesion appearance was 34 years after the initial trauma. The inflammatory environment of ulcers (large amounts of cytotoxic products derived from macrophage activity within the wound, cells with a high mitotic capacity, an ischemic environment, and poor lymphatic drainage) favors carcinogenesis and the formation of tumors such as Marjolin ulcer.1,4,5 In cases of clinical suspicion of this tumor type histology should be performed to confirm the diagnosis. Histology reveals findings compatible with squamous cell carcinoma. The degree of tumor differentiation is the primary long-term prognostic factor; greater degrees of differentiation, ulceration, and dermal infiltration by tumor cells are associated with a higher rate of recurrence.4 Tumor staging should be performed to evaluate lymph node involvement distant from the tumor and to determine the appropriate therapeutic approach. Surgery is the treatment of choice, with reported 2-year survival rates of 66%–80%.5 Adjuvant treatments such as radiotherapy or chemotherapy may be useful in patients with inoperable tumors or those who refuse surgery.
ConclusionLesion chronicity, clinical findings, and clinical-pathological correlation are key to the diagnosis of Marjolin ulcer. A high index of suspicion is necessary to establish an early diagnosis and thereby provide patients with timely treatment.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Dávila Osorio VL, Méndez Gaviria L, Amador Patarroyo JR, González MI. Úlcera de majorlin: 2 casos de carcinoma escamoso sobre cicatriz por trauma en tejidos blandos. Actas Dermosifiliogr. 2020;111:81–82.