Deep penetration of the skin by dermatophytic agents may provoke a granulomatous inflammatory skin reaction. This was first described by Majocchi.1 Majocchi granuloma is characterized clinically by papular, pustular, or nodular inflammatory lesions occurring typically on the limbs or face,2 though isolated cases affecting the vulva or scrotum have been published.3 We report a unique presentation of Majocchi granuloma in the breast; there are no previous reports of involvement of this location.
A 28-year-old female presented with a slightly painful, raised reddish lesion that had developed in her left breast over the previous 3 months. She gave no history of trauma and did not describe constitutional symptoms. The lesion had increased in size after the repeated application of mud to the area over 2 months. Treatment with a potent topical corticosteroid (betamethasone valerate, 0.122% wt/wt) was then applied twice daily for a month.
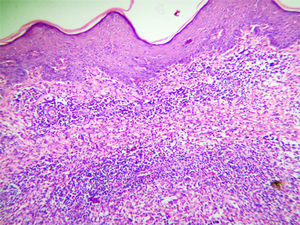
Clinical examination revealed a single erythematous plaque with areas of scarring. A yellowish discharge emanated from multiple openings in an area beneath the left nipple measuring approximately 5×4cm (Fig. 1). On palpation the plaque was firm and indurated and was slightly tender; there was no underlying breast lump. Diascopy findings were nonspecific. Gram stain of the discharge showed the presence of gram-positive cocci and abundant neutrophils. No acid-fast bacilli (AFB) were seen on direct smear. Potassium hydroxide (KOH) mount and fungal culture of skin scrapings and of the discharge was negative. Ultrasonography of the breasts was normal, though a single lymph node of 20×8mm with a preserved hilum was observed in the left axilla. Chest X-ray was normal and the Mantoux skin test produced a wheal of 8×6mm. Routine blood tests were within normal limits. The patient was treated with oral cefuroxime 500mg twice a day plus topical 2% mupirocin cream but showed no improvement after 2 weeks of treatment. We performed skin biopsy based on a differential diagnosis of hidradenitis suppurativa, lupus vulgaris, or subcutaneous fungal infection. Hematoxylin and eosin staining of the sample revealed a mixed cell, granulomatous inflammatory reaction in the dermis (Fig. 2). Ziehl-Neelsen and periodic acid Schiff (PAS) stains to detect AFB and fungi were both negative. Mycobacterial culture of the tissue sample was negative, but fungal culture on Sabouraud dextrose agar with chloramphenicol produced growth of heaped up, folded violaceous colonies of waxy consistency after 3 weeks, suggestive of Trichophyton violaceum. Lactophenol cotton blue mount showed the presence of tangled, irregular branched hyphae with chlamydospores. With a final diagnosis of Majocchi's granuloma, the patient was treated with 250mg of oral terbinafine once daily plus topical 2% sertaconazole cream twice daily. The lesion resolved completely within 8 weeks and there was no evidence of recurrence after 6 months of follow-up (Fig. 3).
In 1883, Majocchi1 described a phenomenon in which dermatophytes, which usually remain limited to the stratum corneum, become more aggressive and invade the superficial dermis. Majocchi granuloma typically develops when a dermatophyte infection extends down a hair follicle in the setting of localized immunosuppression (most commonly a potent topical steroid) or systemic immunosuppression. The result is a granulomatous response in the dermis.2 The commonly implicated organisms are Trichophyton species (rubrum, mentagrophytes complex, violaceum) as well as some nondermatophyte species such as Aspergillus and Phoma.4 Although historically T. violaceum has been the most commonly identified organism, Majocchi granuloma now a days is usually due to T rubrum.
Two clinical forms of Majocchi granuloma, follicular and subcutaneous nodular, have been described.4 The follicular type usually develops after trauma, repeated shaving of hair-bearing areas, or topical corticosteroid treatment, and in cases of long-standing immunosuppression.5,6 The subcutaneous nodular type occurs in immunocompromised hosts. Our patient developed the follicular type, probably caused by endothrix-type infection due to anthropophilic T. violaceum secondary to the use of a potent topical steroid under occlusion, which could have led to deep penetration of the fungus. In modern medicine, systemic antifungals such as griseofulvin,7 itraconazole,8 and terbinafine9 are the mainstays of therapy as they are safe and effective. The duration of therapy should be of at least 4–8 weeks, and treatment should be continued until all lesions have cleared. In the reports in literature, nearly all lesions resolve without scarring within 6 weeks of starting antifungal. The response of Majocchi granuloma to oral terbinafine can be explained on the basis of its pharmacokinetics.10 Terbinafine is the preferred oral therapy for treating Majocchi granuloma not only for its superior efficacy in eliminating dermatophytes, but also because of its greater selectivity for the skin structures involved in Majocchi granuloma and fewer drug interactions than azole antifungals like itraconazole.9 We used terbinafine for its good antidermatophyte activity, adequate penetration into common sites of dermatophyte infection (stratum corneum and the hair follicle), lower rates of recurrence, low rate of drug interactions (its metabolism does not involve cytochrome P450), and its cost effectiveness when long-term therapy is warranted to prevent relapse.8 A diagnosis of Majocchi granuloma should always be considered in papular-pustular plaques, especially when the patient describes factors associated with local or systemic immunosuppression. Negative results of KOH examination or fungal culture of skin scrapings or of the purulent discharge do not exclude a diagnosis of Majocchi granuloma, which should be confirmed either by tissue culture or by PAS staining of histopathology samples. Although the detection of fungal spores or hyphae using special stains on histopathology samples will confirm the diagnosis, these structures may sometimes escape detection, as in our case.11 Fungal spores and hyphae are usually detected within hairs or hair follicles and in dermal granulomas. Our inability to detect the fungal elements may have been due to the absence of hair follicles and the poorly defined granulomas in our biopsy specimen. To the best of our knowledge, this is the first reported case of Majocchi granuloma of the breast.
Conflict of interestsThe authors declare no conflict of interest.