The safety and efficacy profile of dupilumab in the management of atopic dermatitis (AD) are established in clinical trials. However, long-term real-world persistence data in Spain are limited.
ObjectiveThe primary endpoint of the study was to assess the 4-year persistence of dupilumab in routine clinical practice in patients with moderate-to-severe AD. Secondary endpoints included the analysis of safety and efficacy profile during the same period of time.
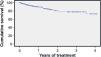
MethodsWe conducted a retrospective cohort study of dispensation registries and health records from 5 hospitals. Adults with moderate-to-severe AD starting on dupilumab treatment were followed for 4-years. Dupilumab persistence was estimated using Kaplan–Meier analysis. Efficacy was measured by changes in EASI and IGA scores. Significant adverse events (AEs) leading to discontinuation were recorded.
ResultsA total of 251 patients included (mean age, 46 years; 59.4%, men; 64.5% with at least 1 atopic comorbidity; mean time from AD diagnosis, 14.5 years). Of these, 196 (78.1%) had been on ≥2 systemic therapies before starting dupilumab. Baseline EASI and IGA values averaged 27.9 and 4.0, respectively. Persistence rates were 90%, 80%, 78%, and 73% after 1, 2, 3, and 4-years, respectively. By 16 weeks, 47.8% and 54.7% of patients achieved EASI ≤3 or IGA ≤1, increasing to 76.3% and 77.2% by 52 weeks, and reaching 90.9% in the group followed for >3 years. A total of 38 patients (13.5%) discontinued dupilumab, mainly due to inefficacy (5.6%) and AEs (1.2%).
ConclusionDupilumab effectively reduced AD severity within the first few weeks, with most patients achieving mild/minimal disease activity or complete clearance by year 1. The observed safety profile was consistent with known data. High persistence rates up to 4-years suggest satisfaction with dupilumab long-term safety and efficacy profile in managing moderate-to-severe AD.
Dupilumab (Dupixent®) is a fully human IgG4 monoclonal antibody that inhibits both IL-4 and IL-13 by antagonizing the IL-4 receptor. It has been the first biologic approved by the EMA for the treatment of moderate-to-severe Atopic dermatitis (AD) in adults and adolescents (≥12 years) and severe AD in children aged 6 months–11 years who are eligible for systemic therapy.1 EMA approval was based on clinical trials showing significant reductions in clinical signs and symptoms and improvements in patient-reported outcomes, including sleep and QoL.1 Furthermore, the 5-year long-term safety and efficacy profile has been demonstrated.2–4 Current European clinical practice guidelines include dupilumab as an option for adults and adolescents with moderate-to-severe AD.5 However, real-world patients often differ from those in clinical trials, and treatment persistence can be influenced by various clinical and behavioral factors that reflect the balance of safety, efficacy, tolerability, and adherence, and is a useful measure of therapeutic value.6 Data on dupilumab persistence in Spain remain scarce, with only 1 study reporting 80% persistence at 2 years.7 This study evaluates the long-term persistence, safety, and efficacy of dupilumab in adult patients with moderate-to-severe AD treated in 5 centers across Valencian Community (Spain).
MethodsStudy design and populationThis retrospective observational study included AD patients treated with dupilumab at 5 hospitals in Valencian Community (Spain). Inclusion criteria were: (1) ≥18 years old; (2) diagnosis of moderate-to-severe AD; (3) at least 1 dispensation of dupilumab treatment. Patients who met these criteria and initiated dupilumab at any date (first dispensation was the index date) were followed until December 31st, 2021, or disenrollment.
Primary endpoints and measuresBaseline demographics and clinical characteristics, including age, sex, AD onset, atopic comorbidities, and previous treatment, were collected. Disease severity was assessed using the Eczema Area and Severity Index (EASI) and Investigator's Global Assessment (IGA) scores at baseline, 16 weeks, 24 weeks, 52 weeks, and the last visit during follow-up.
The primary endpoint included an assessment of the real-world persistence of dupilumab in adults with moderate-to-severe AD. Persistence, defined as the duration from initiation to discontinuation, was measured as the last day of dispensation plus the interval until the next scheduled administration. Kaplan–Meier analysis estimated persistence at 1, 2, 3, and 4 years.
Secondary endpoints included characterizing patients who initiated dupilumab, reasons for discontinuation, safety and efficacy. Efficacy was assessed by changes in EASI and IGA scores from baseline to each assessment date over 4 years. Safety was estimated by the percentage of patients reporting intolerance or AEs and discontinuing treatment.
Subgroup analyses were performed according to age (18–35, 36–65, and >65 years) to assess variations in disease presentation and treatment response across life stages; dosing regimen (SmPC vs adapted) to evaluate real-world needs for dose intensification or interval extension and their effects on outcomes; and total population vs high responders (defined as achieving EASI ≤3 at week 16), as evaluating high responders helped identify characteristics associated with robust efficacy and inform personalized treatment strategies and resource optimization. Adherence was assessed using the medication possession ratio (MPR), calculated from pharmacy dispensing records.
Statistical analysisChi-square and Fisher's exact tests assessed associations across variables. Group comparisons used ANOVA, Student's t test, and non-parametric Mann–Whitney and Wilcoxon tests. Multivariate analysis, including principal component analysis, identified patient subgroups and defining variables. Hierarchical group analysis identified patterns of association between variables. Correlations between canonical variables and derived algorithms integrated clinical and analytical variables to classify patients by their response to the drug.
ResultsClinical characteristics of the study populationThe baseline characteristics of the study population are shown in Table 1. The study included a total of 251 adult patients (59.4%, men; mean age, 43.6 years). The average time since disease onset was 14.5 years, with 51.4% being diagnosed in adulthood. Almost two-thirds (64.5%) had at least 1 coexisting T2 inflammatory disease (41% and 19% had at least 2 or 3, respectively). Allergic rhinitis was most common (52%), followed by asthma (35%) and allergic conjunctivitis (26%). At baseline, patients had a mean EASI of 27.9 and a median IGA score of 4, indicating predominantly severe AD. On average, patients had used 2.5 systemic treatments prior to dupilumab, with 78.1% having received >2 systemic treatments and 21% having received >4. Widely used systemic drugs included corticosteroids (91.6%), cyclosporine (70.9%), and methotrexate (27.9%). There were no differences in baseline characteristics across age or regimen subgroups.
Demographics characteristics and baseline parameters of the study population.
| Total sample, n (%) | 251 (100) |
| Age, mean±SD | 43.6±18.9 |
| 18–35 years, n (%) | 101 (40.2) |
| 36–65 years, n (%) | 109 (43.4) |
| >65 years, n (%) | 41 (16.3) |
| Sex (male), n (%) | 149 (59.4) |
| Years since AD diagnosis, mean±SD | 14.5±14.8 |
| Number of atopic comorbidities | |
| ≥1 atopic comorbidity, n (%) | 162 (64.5) |
| ≥2 atopic comorbidity, n (%) | 103 (41.0) |
| ≥3 atopic comorbidity, n (%) | 48 (19.1) |
| Type of atopic comorbidity | |
| Allergic rhinitis, n (%) | 130 (51.8) |
| Asthma, n (%) | 87 (34.7) |
| Food allergy, n (%) | 40 (15.9) |
| Allergic conjunctivitis, n (%) | 66 (26.3) |
| Chronic rhinosinusitis or nasal polyposis, n (%) | 7 (2.8) |
| Eosinophilic esophagitis, n (%) | 1 (0.4) |
| Baseline EASI, mean±SD | 27.9±8.3 |
| Baseline IGA, median±SD | 4.0±0.5 |
| No. of prior treatments (average) | 2.5 |
| ≥1 previous treatment, n (%) | 242 (96.4) |
| ≥2 previous treatments, n (%) | 196 (78.1) |
| ≥3 previous treatments, n (%) | 93 (37.1) |
| Treatment history | |
| Oral corticosteroids, n (%) | 230 (91.6) |
| Cyclosporine, n (%) | 178 (70.9) |
| Methotrexate, n (%) | 70 (27.9) |
| Azathioprine, n (%) | 50 (19.9) |
| Phototherapy, n (%) | 46 (18.3) |
| Off-label biologics therapy, n (%) | 37 (14.7) |
| Mycophenolate, n (%) | 15 (6.0) |
| Immunoglobulins, n (%) | 5 (2.0) |
EASI: Eczema Area and Severity Index; IGA: Investigator's Global Assessment; SD: standard deviation.
Patients were followed for a mean of 1.5 years; 51.4% (129 patients) had at least 1 year of follow-up, with a maximum exposure of 211 weeks (4 years). A total of 87.6% (220 patients) followed the SmPC dosing regimen, while 12.4% (31 patients) had customized dosing adjustments. Of these, 2% (5 patients) intensified treatment to 300mg every 7 days, and 10% (26 patients) optimized it to 300mg every 21 to 42 days. Notably, 95% of patients were fully adherent to dupilumab, as measured by the MPR.
Reasons for discontinuationAt data lock, 86.4% (217 patients) remained on dupilumab, whereas 13.5% (34 patients) had discontinued treatment. When discontinuations were categorized by reason (Table 2), 5.6% were due to lack of efficacy, 2.8% to patient decision, 2.4% to loss to follow-up, and 1.6% to adverse events or intolerance. Most discontinuations (62%) occurred before week 52 and were attributed to inadequate efficacy. No differences in discontinuation rates were observed across age groups or dosing regimen subgroups.
Reasons for treatment discontinuation.
| Treatment discontinuation, n (%) | Total34 (13.5) | Year 121 (8.4) | >Year 114 (5.6) |
|---|---|---|---|
| Lack of efficacy | 14 (5.6) | 9 (3.6) | 5 (2.0) |
| Patient's decision | 7 (2.8) | 3 (1.2) | 4 (1.6) |
| Loss of follow-up | 6 (2.4) | 3 (1.2) | 4 (1.6) |
| Adverse events | 4 (1.6) | 3 (1.2) | 1 (0.4) |
| Conjunctivitis | 1 (0.4) | 1 (0.4) | 0 |
| Liver cirrhosis decompensation and death unrelated to dupilumab | 1 (0.4) | 1 (0.4) | 0 |
| Death due to kidney failure, unrelated to dupilumab | 1 (0.4) | 1 (0.4) | 0 |
| Death due to prostate cancer, unrelated to dupilumab | 1 (0.4) | 0 | 1 (0.4) |
| Intolerance | 1 (0.4) | 1 (0.4) | 0 |
| Diagnostic change | 1 (0.4) | 1 (0.4) | 0 |
| Not recorded | 1 (0.4) | 1 (0.4) | 0 |
The persistence of dupilumab was 90%, 80%, 78%, and 73% at 1, 2, 3, and 4 years, respectively (Fig. 1 and Supp. Table 1). Persistence in patients with high response to dupilumab (EASI ≤3 at 16 weeks) remained >85% throughout the 4 years (94%, 86%, 86%, and 86%, respectively) (Supp. Table 1). No differences in persistence were observed among age or regimen subgroups.
EfficacyTreatment with dupilumab resulted in a rapid and significant reduction in EASI/IGA scores from baseline (EASI 27.9; IGA 4) to week 16 (EASI 5.9; IGA 1.5) (p<0.0001). EASI/IGA scores continued to decrease progressively until nearly complete clearance with ongoing treatment (Fig, 2A and B). At 16 weeks, 67.2% of patients achieved EASI-75, increasing to >80% at week 24. EASI-90 was achieved in 44.4% at 16 weeks, increasing to 63.5%, 76.3%, 74.1%, 86.2%, and 90% at 24, 52, 53–104, 105–156, and >156 weeks, respectively (Fig. 2C).
Efficacy of dupilumab during follow-up. (A) Mean EASI progression; (B) median IGA progression; (C) percentage of patients achieving EASI-50, EASI-75 and EASI-90 during the follow-up; (D) percentage of patients with EASI ≤7 and EASI ≤3 at 16 and 52 weeks, respectively; (E) percentage of patients with IGA ≤1 and IGA=0 at 16 and 52 weeks, respectively.
The proportion of mild AD (EASI ≤7) was 70.6% at 16 weeks and 94.8% at 52 weeks (Fig. 2D). At 16 weeks, minimal or no disease (EASI ≤3 or IGA ≤1) was achieved in 47.8% and 54.7% of patients, respectively. These values increased to 76.3% and 77.2% at 52 weeks and continued to rise to 90.9% in patients followed >156 weeks. Complete AD clearance (IGA=0) was achieved in 17.6% at 16 weeks, 38.2% at 52 weeks, and 72.7% in those followed >156 weeks (Fig. 2E). The reduction in EASI and IGA scores was consistent across all age and regimen subgroups (Supp. Fig. 1).
SafetyIn the overall cohort, 1.6% of patients discontinued for safety reasons: 1 due to intolerance and 4 due to AEs, with only 1 drug-related discontinuation (conjunctivitis) (Table 2). No differences in the safety profile were observed among age or regimen subgroups.
DiscussionLong-term control of moderate-to-severe AD was extremely challenging with conventional therapies. Dupilumab has revolutionized AD management, showing long-term remission in many patients.2 However, conditions in clinical trials often differ from real-world settings, necessitating evaluation in clinical practice.
This study revealed that nearly half of patients with AD had adult-onset, challenging the notion of AD as solely a childhood disease. More than 64% had at least atopic comorbidity, emphasizing the link between AD and other T2 inflammatory diseases.8–12 Dupilumab has proven safe and effective for several T2 conditions, offering this versatility a therapeutic advantage for patients with multiple conditions.13–15 A total of 14% had previously used off-label biologics, highlighting the limited number of treatments available before dupilumab. In this study, the rate of dupilumab discontinuation was 13.5%, with 5.6% due to lack of efficacy and 1.2% due to AEs, which is consistent with its established safety profile and real-world studies in The Netherlands, Italy, and Spain, reporting similar discontinuation rates (4%–14%) at the 2–4-year follow-up.7,16,17 These findings support dupilumab as a valuable treatment option, with low discontinuation due to ineffectiveness or side effects.
In routine clinical practice, long-term safety and efficacy are related to treatment persistence. Overall, dupilumab showed good persistence rates of 90%, 80%, 78%, and 73% at 1, 2, 3, and 4 years, respectively. Previous real-life studies reported 2-year survival rates ranging from 77% to 89%.16,18 Similar persistence was noted in 2 recent studies: a Dutch cohort of 715 AD patients with survival rates of 90.3%, 85.4%, and 78.6% after 1, 2, and 3 years, respectively12; and an Italian study of 363 patients with AD reporting rates of 91.5%, 82.9%, 78.8%, and 76.4% at 1, 2, 3, and 4 years.17 Long-term efficacy, limited AEs, and no drug-drug interactions or organ toxicity contributed to these high survival rates.16
Regarding treatment efficacy, the mean baseline EASI score was 27.9 and IGA was 4, which is similar to those reported in clinical trials,19 indicating the severity of patients with AD. Our study showed a rapid response to dupilumab, with significant improvement seen early on, as EASI dropped to 5.9 and IGA to 1.5 at 16 weeks. The PROSE registry,20 conducted in real life over 3 years, reported similar short-term results, with EASI around 5.3 after 3–6 months. Since their baseline EASI was ∼16 vs our 28, our short-term results are comparable or better (5.9 in 4 months).
In our study, a total of 70% of patients achieved EASI-75 at 16 weeks, increasing to >85% at 24 and 52 weeks. Clinically, this means some persistent eczema requiring almost continuous topical treatment. However, our stretch target is EASI-90, indicating occasional corticosteroid use, and response rates were 44% at 16 weeks and nearly 80% at 52 weeks, with most patients clear of lesions. These rates were higher than those in a recent meta-analysis, where 59.8% and 26.8% achieved EASI-75 and EASI-90, respectively, after 16 weeks of dupilumab therapy.21
The high burden of AD on patient QoL demands continuous optimization of therapeutic targets, ensuring patients achieve EASI ≤3 or IGA ≤1. Real-world studies report IGA clear/minimal scores in 38%–60% of patients within 3–4 months of dupilumab initiation.22,23 Our study found minimal or complete clearance (IGA 0-1) in 54.7% at 16 weeks, increasing to 77.2% at 52 weeks, with further improvement over time. Long-term data indicated sustained responses, with EASI and IGA score reductions maintained up to 4 years. The percentage of patients achieving IGA 0–1 at 104 weeks (68%) was comparable to open-label extension studies at weeks 76 (57.8%) and 100 (58.1%).3,24
Two other studies on the long-term real-world drug survival of dupilumab have been recently published, further reinforcing its role in managing AD. Barei et al.25 reported a 74.1% drug survival rate at 65 months, highlighting the 5-year dupilumab sustained safety and efficacy profile, while Torres et al.26 demonstrated an 82.0% drug survival rate at 30 months, with significant improvements in EASI (89.3% decrease from baseline). These outcomes are consistent with our findings, including substantial reductions in EASI and persistence rates of 90% and 80% at 1 and 2 years, respectively. Both studies corroborate dupilumab safety and durability, with conjunctivitis being the most common adverse event, consistent with our data. These comparisons strengthen the evidence for dupilumab's long-term utility in diverse populations.
In our study, only 1.2% of patients who discontinued dupilumab treatment did so due to AEs, confirming an excellent long-term safety profile and product value. Conjunctivitis was the only common reported AE although is important to highlight that it was a high percentage of patients with baseline allergic conjunctivitis before starting treatment with dupilumab. In the 4-year open-label study of dupilumab, conjunctivitis appeared in 20% of patients, although only 9.6% were related to dupilumab and most cases were mild with only 0.5% of patients finally discontinuing treatment due to conjunctivitis.4 We have learnt that conjunctivitis appears mainly at the beginning of the treatment and most cases can be prevented with hyaluronic eye drops. In the clinical program of the rest of dupilumab indications (eosinophilic esophagitis, asthma, chronic rhinosinusitis with nasal polyps, prurigo nodularis), the rate of conjunctivitis is very low, so we can assume that it is an AE associated only with AD. The real-world experience reported higher rates of dupilumab discontinuation due to AEs than us (3%–4.9%), but we agree with other real-life studies that conjunctivitis or ocular surface disease is the most common AE associated with dupilumab.16 Of note, several studies have demonstrated that AD, comorbid asthma and rhinitis are risk factors for ocular surface disease.27 Furthermore, several epidemiology studies have revealed that patients with more severe AD have an increased risk of developing conjunctivitis, even in the absence of biologics.27,28
Our study has several strengths, including high therapeutic adherence, conferring robustness and validity to the results. However, there are important limitations to consider, including the limited sample size, particularly at later time points, where fewer patients remained under observation, reducing the generalizability of long-term persistence conclusions. Specifically, while our persistence rates at 3 and 4 years remained high (78% and 73%, respectively), the number of patients at these time points was considerably lower, making these estimates less robust than those obtained within the first 2 years. Therefore, the most reliable persistence data come from the first 2 years, where patient numbers were larger. Additionally, the observational and retrospective design and lack of a control arm further limits the study. The data lock was also set before the introduction of new systemic therapies. Since our study followed patients until December 2021, it does not account for the impact of new systemic therapies introduced afterwards. The availability of alternative treatments may lead to different real-world outcomes for dupilumab if analyzed today. Therefore, future studies should evaluate dupilumab persistence in the context of a broader range of available therapies to better understand treatment retention trends in a competitive therapeutic landscape. This, along with the small number of patients >2 years in our study, highlights the need for future studies with extended follow-up. In this regard, the ongoing SireDupi2 study aims to evaluate dupilumab persistence in a broader population over a longer period, providing more robust data for future analyses and comparisons with new systemic therapies.
ConclusionsThis study corroborates findings from dupilumab clinical trials and other real-world studies, supporting its long-term use in AD patients and confirming its clinical benefits. The results demonstrate that dupilumab is effective in adults with moderate-to-severe AD, offering significant improvements in global AD severity. The observed safety was consistent with the known profile, with no new safety signals identified over 4 years. Dupilumab showed high persistence, suggesting satisfaction among patients and healthcare professionals with its effectiveness, safety, and treatment regimen over time.
Ethical and legal aspectsThis study was governed by the basic ethical principles of the Declaration of Helsinki. Patient data were handled in line with current Spanish legislation on data protection (Organic Law 3/2018 of December 5 on the protection of personal data and guarantees of digital rights and the general regulation of data protection).
FundingStudy sponsored by Sanofi.
Conflicts of interestJuan Francisco Silvestre has received speaking and/or consulting fees from Sanofi, Regeneron, Abbvie, Eli Lilly, Galderma, Leo Pharma, Novartis and Pfizer, and/or research funds from AbbVie, Almirall, Amgen, AstraZeneca, Bristol Meyer Squibb, Eli Lilly, Incyte, Leo Pharma, Novartis, Pfizer and Sanofi. Sergio Santos-Alarcón has received speaking and/or consulting fees and/or research funds from Almirall, Abbvie, Amgen, Pfizer, Novartis, Janssen-Cilag, Lilly, Leo Pharma, UCB Pharma, Pierre Fabre, Isdin and Sanofi. Amando Mengual-Sendra has received honoraria for attending symposia/congresses and/or for speaking and/or consulting, and/or research funds from Abbvie, AstraZeneca, GlaxoSmithKline, Sanofi, Stada and UCB Pharma. María Pilar Ortega-García has received honoraria for attending symposia/congresses and/or for speaking and/or consulting, and/or research funds from Sanofi, Pfizer and Biogen. Emilio Monte-Boquet has received speaking fees, training and/or research funds from Abbott/Abbvie, Amgen, Astellas, AstraZeneca, Baxalta, Bayer, Biogen, Bristol-Myers Squibb, Celgene, Chiesi, Eisai, Fresenius, Gilead, GSK, Ipsen, Janseen, Leo Pharma, Lilly, MSD, Merck-Serono, Novartis, Pfizer, Roche, Sanofi, Shire, Theramex UCB, and y ViiV. Noemí Pérez Prior has received honoraria for attending symposia/congresses and/or speaking and/or consulting fees, and/or research funds from Sanofi-Aventis, S.A. Francisco Javier Miquel has received speaking and/or consulting fees from Sanofi, Regeneron, Abbvie, Eli Lilly, Leo Pharma, Novartis and Pfizer, and has participated as principal investigator in clinical trials sponsored by AbbVie, Amgen, and Sanofi. Joaquín Borras-Blasco has received honoraria for attending symposia/congresses and/or speaking and/or consulting fees, and/or research funds from Sanofi, Janssen, Pfizer and Biogen. The remaining authors declared no other conflicts of interest whatsoever.
Data availabilityThe data that support the findings of this study are available on request from the corresponding author. Data are not publicly available due to privacy or ethical restrictions.
The authors thank the staff of the participant study centers for their contribution to this work. In addition, we thank Anchel González Barriga and Vanessa Marfil Vives of Medical Science Consulting (Spain) for providing editorial support, in the form of medical writing and assembling tables based on authors’ detailed directions, collating author comments, copyediting, fact-checking, and referencing. Sanofi funded this editorial support.