A 47-year-old woman with no past history of interest visited our department with a paranasal papule on the left side of the nose, which had appeared more than 15 years earlier. The lesion had grown in recent months and was itchy.
Physical ExaminationPhysical examination revealed a papule measuring 4×6mm, with a whitish central region and slightly erythematous edges (Fig. 1). Nonpolarized light contact dermatoscopy revealed a lesion with telangiectasis, linear vessels (upper region) and peripheral polymorphic vessels on a yellowish-pink background, with a central milky-white spherical area, with no ulceration (Fig. 2).
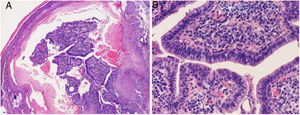
HistopathologyThe excisional biopsy showed epidermal invagination with proliferation of papillary elements, which presented a double layer of epithelial cells. The stroma of these papillae revealed an inflammatory infiltrate with abundant plasma cells (Fig. 3).
[[?]]What is your Diagnosis?
DiagnosisSyringocystadenoma papilliferum (SCAP).
CommentSCAP is a rare benign adnexal tumor derived from the sweat glands. It is present from birth in half of cases and appears during puberty in between 15% and 30% of cases. It may occur de novo in cases of sebaceous nevus, although it may also be associated with many benign and malignant lesions, such as basal cell carcinoma, common warts, and different adnexal tumors. Clinical presentation is variable and nonspecific, and 3 forms are known: nodular, plaque and linear. It generally presents as a solitary papillomatous or verrucous, and sometimes erosive, nodule or plaque of variable size, on the head or neck, but may appear in other locations. It sometimes presents a small fistula with a clear, bloody, foul-smelling exudate. Diagnosis is histologic and characteristic, with numerous cystic invaginations connected to the epidermis and extending into the dermis. They are formed by papillary branches of different sizes, covered by a double-layer epithelium, with cuboidal basal cells and columnar apical cells that may show secretion due to decapitation. A dense inflammatory infiltrate with plasma cells in the stroma is characteristic. The treatment of choice is complete surgical excision, as, although SCAP is benign, cases with metastasis and association with other malignant tumors have been described.
Few dermatoscopic descriptions of this disease exist. Most correspond to SCAP associated with sebaceous nevus, with 14 cases, and only 2 correspond to solitary SCAP. Bruno et al. first published the dermatoscopic findings of SCAP associated with sebaceous nevus, describing a varied vascular pattern (linear, horseshoe-shaped, and glomerular) on a pink-white background.1 In another review of tumors over sebaceous nevus,2 the authors describe 9 SCAP, most of which show a symmetric lesion with exophytic papillary structures, erosions, scabs, ulceration, and different vessels (hairpin, polymorphous and comma-shaped); in another SCAP, also over sebaceous nevus,3 the authors described a yellowish-white lesion with polymorphous vessels and a peripheral ring with hairpin vessels. Those authors speculate that the vascular structures may be related to manipulation or trauma. Recently, in 3 other lesions, the main findings were pinkish-white exophytic papillary structures and polymorphous vessels.4 In the cases of SCAP without sebaceous nevus, one lesion showed milky-white amorphous spherical structures (corresponding histologically to tumor luminal cells) and peripheral telangiectasia,5 and another showed milky-red papillomatous projections with central ulceration and yellowish areas within the ulcerated areas (secretion sites) and polymorphous vessels.6 It thus appears that the pinkish-white exophytic papillary structures and polymorphous and linear vessels are key to diagnosing SCAP, but is appears that milky-white spherical structures, as in our case, may also be key. The role of dermatoscopy in diagnosing adnexal tumors is not currently well known and histopathology provides the definitive diagnosis.
Please cite this article as: García-Arpa M, Lozano-Masdemont B, Flores-Terry MÁ, Delgado Portela M. Pápula solitaria nasal de larga evolución. Actas Dermosifiliogr. 2019;110:857–858.