The patient was a 66-year-old man with a history of dyslipidemia and inguinal hernioplasty, no known drug allergies, and no relevant past history of skin disease. He was referred to the dermatology department for assessment of asymptomatic papules on the scrotum, which had first appeared 20 years earlier and developed gradually. No relation to any specific causative agent was found (Figure 1). The patient had a stable partner, no past history of sexually transmitted infection, and no family history of similar lesions.
Physical ExaminationPhysical examination revealed more than 25 papules the color of normal skin, approximately 4mm in diameter, on the scrotum.
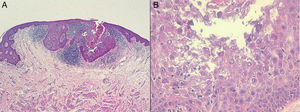
HistopathologyHistologic examination revealed prominent hyperkeratosis and an adjacent lymphocytic inflammatory infiltrate, foci of dyskeratosis and acantholysis, and the appearance of keratinocytes with pyknotic nuclei and clear cytoplasm (Figure 2, A and B).
What Is Your Diagnosis?
DiagnosisGiven the absence of pruritus and similar lesions at other sites, the diagnosis consistent with the histopathologic findings was papular acantholytic dyskeratosis of the anogenital area. Other potentially communicable entities were ruled out.
Clinical Course and TreatmentTreatment was initiated with pimecrolimus cream, twice daily for 8 weeks. The lesions improved slightly and remained stable after withdrawal of the drug.
CommentPapular acantholytic dyskeratosis of the anogenital area is a benign, chronic, noncommunicable entity that is rare in men, although the reason for the difference between the sexes is unknown. Clinically, this entity is characterized by multiple small papular lesions that are whitish or skin-colored and either appear in isolation or form plaques. The lesions can be asymptomatic or cause pruritus. They are located on the anogenital area and do not affect any other part of the body.1–3
As for etiology and pathogenesis, mosaicism of the ATP2A2 gene has been detected,4 specifically p.706D>N mutations, which are also present in Darier disease. ATP2A2 encodes the type 2 sarcoplasmic reticulum calcium pump, and the domain where p.706D>N occurs is responsible for regulating the enzymatic phosphorylation that conditions calcium conductance. This mutation causes aberrant calcium flux that leads to the loss of epidermal integrity. Knopp et al.4 did not find the mutated allele in a sample of normal skin taken from an area adjacent to the lesions, although they did find it in samples of the affected skin. It has been suggested that there may be an etiologic and pathogenic relationship to Hailey-Hailey disease, given that the same mutation in the ATP2C1 gene has been found in affected tissue in some patients, although the exclusive involvement of the anogenital area and the absence of family history contradicts this theory.4
Definitive diagnosis is made by biopsy, which characteristically reveals a pattern of focal acantholytic dyskeratosis that is also typical of entities such as Darier disease, Hailey-Hailey disease, and Grover disease.2–4 The clinical differential diagnosis should include sexually transmitted infections such as genital warts,4 molluscum contagiosum, and the histologic differential diagnosis should include the other entities mentioned above.2,3 Darier disease is clinically characterized by multiple crusted, pruritic papules in seborrheic areas, and there have been no reports of the disease exclusively affecting the genital area. There have been reports of Hailey-Hailey disease affecting only the genital area, but the patients had a family history of the disease. In Grover disease, similar lesions appear on the trunk, the neck, and the proximal region of the limbs, but there is no genital involvement.3
As for therapeutic management, no treatment is needed if the lesions are asymptomatic; in symptomatic cases, various treatments can be used. Treatments include corticosteroids, retinoids, and topical immunomodulators,2 although it is also possible to use physical treatments—which tend to be more effective—such as cryotherapy, electrocoagulation, excision, and carbon dioxide laser therapy.3,5
In conclusion, papular acantholytic dyskeratosis of the anogenital area is a benign entity located exclusively in the genital area. Therefore, it is important to differentiate this entity adequately from genital warts in order to avoid subjecting patients to expensive and unnecessary treatments.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Varela-Veiga A. Lesiones papulosas en el escroto de larga evolución. Actas Dermosifiliogr. 2017;108:155–156.