Lupus panniculitis (LP) is a rare variant of cutaneous lupus erythematosus (CLE) that primarily affects the deep dermis and adipose tissue.1 It develops in 1% to 3% of patients with CLE. Antinuclear antibodies (ANA) are positive in 70% of cases, but only 25% to 50% satisfy the criteria for systemic lupus erythematosus.2 The diagnosis of LP is based on the correlation of clinical, serological, and, most importantly, histopathological findings. Direct immunofluorescence is positive in 70% to 80% of cases and can help to confirm the diagnosis.2 LP with a linear or annular morphology is extremely rare; only 14 cases of linear LP have been described,3–7 and just 1 case of LP with annular lesions8 (Table 1). Of these 15 cases, 9 affected the scalp.
Review of the Published Cases of Lupus Panniculitis With a Linear or Annular Pattern.
| Reference | Age, y/Sex/Country | Site | Lesion morphology | Immunological Study | Treatment | Response |
| Tada et al., 1991 | 9/M/Japan | Left leg | Linear | Negative | TC | Improvement |
| Innocenzi et al., 1997 | 17/M/Italy | Breast, right arm | Linear | ANA 1:40 | Not mentioned | |
| Tamada et al.3; 1999 | 19/M/Japan | Left arm | Linear | Negative | IC | Improvement |
| Nagai et al.4; 2003 | 10/F/Japan | Scalp, forehead | Linear | ANA 1:320 | TC | Improvement, SA |
| Wu et al., 2004 | 21/F/Taiwan | Scalp | Linear | Negative | HCQ | CR |
| [1,0]Marzano et al., 2005 | 21/F/Italy | Scalp, forehead | Linear | ANA 1:280 | OC, Cy, IVC | SLE, SA, skin atrophy |
| 32/F/Italy | Right arm | Linear | ANA 1:640 | OC, HCQ | Skin atrophy | |
| Bacanli et al.8; 2005 | 16/F/Turkey | Scalp, axilla | Annular, linear | ANA 1:320 | HCQ | Improvement, SA |
| Shin et al.5; 2007 | 20/M/Korea | Scalp | Linear | Negative | TC, IC, OC | Improvement, skin atrophy |
| [1,0]Rhee et al., 2009 | 14/M/Korea | Scalp | Linear | Not mentioned | HCQ, OC, IC | CR |
| 21/M/Korea | Scalp | Linear | Not mentioned | DP | CR | |
| Tamiya et al., 2010 | 6/F/Japan | Face | Linear | Negative | OC, TC | CR |
| Lee et al., 2011 | 28/F/Korea | Back, right thigh | Linear | ANA 1:2560 | HCQ | Lipoatrophy |
| Chen et al.6; 2012 | 32/M/Taiwan | Scalp | Linear | Negative | HCQ, IC | CR |
| Tsuzaka et al.7; 2012 | 26/F/Japan | Scalp, forehead | Linear | ANA 1:1280, Anti-Ro+ | OC | CR |
| Present case | 34/M/Spain | Scalp | Annular, linear | ANA 1:320, Anti-Ro+ | HCQ, OC | Improvement |
Abbreviations: ANA, antinuclear antibodies; CR, complete remission; Cy, cyclophosphamide; DP, dapsone; F, female; HCQ, hydroxychloroquine; IC, intralesional corticosteroids; IVC, intravenous corticosteroids; M, male; OC, oral corticosteroids; SA, scarring alopecia; SLE, systemic lupus erythematosus; TC, topical corticosteroids.
We present the case of a 34-year-old man who consulted because of a plaque of alopecia that had been present in the right parietal region for 12 months. Three months earlier he had been diagnosed with alopecia areata but the plaque did not respond to treatment with topical corticosteroids and subsequently had increased in size and had become erythematous and painful. The patient did not report fever, joint pain, oral aphthous ulcers, or other associated symptoms. Physical examination revealed an erythematous, edematous plaque of alopecia in the right parietal region. The plaque had an annular morphology and measured about 6cm in diameter (Fig. 1A). Skin biopsy findings were compatible with lupus panniculitis, and direct immunofluorescence revealed granular deposits of immunoglobulin M in the basement membrane. Complete blood count and serum biochemistry were normal, and immunological study was positive for ANA at a titer of 1:320 and for Anti-Ro.
A, Annular plaque of alopecia situated at the vertex. B, Plaque of alopecia that simulates alopecia areata. C. Arcuate plaque of alopecia that appears to follow the Blaschko lines. D, Distribution of the Blaschko lines on the scalp (pattern proposed by Happle9).
A new plaque of alopecia simulating alopecia areata was observed in the occipital region at subsequent follow-up visits (Fig. 1B).
A diagnosis of LP was made based on the clinical, histological, and serological findings, and a 5-month course of treatment with hydroxychloroquine was started at a dose of 400mg/d. This regimen produced a reduction in the erythema and induration of the plaque and resolution of the alopecia. The patient did not attend the scheduled follow-up, but came to an unscheduled visit at 12 months, at which time he presented multiple firm erythematous nodules and nonscarring alopecia with an annular and linear morphology located in the occipital and both parietal regions (Fig. 1C). Oral prednisone was prescribed at a dose of 30mg/d tapered over 3 weeks; there was an initial improvement, but the lesions recurred after treatment was discontinued.
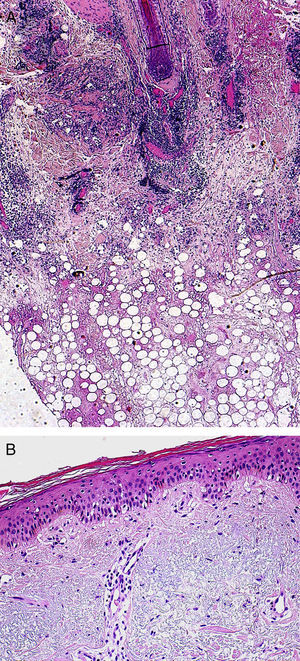
Linear LP localized to the scalp was first described by Nagai et al.4 in 2003. A further 7 cases of LP in a linear pattern on the scalp have been described and 1 case of LP at the same site with an annular pattern.5–8 Most of the cases have been reported in southwest Asia,6 suggesting a genetic or ethnic predisposition; the condition affects both sexes and occurs mainly in young patients. Clinical presentation takes the form of plaques of alopecia; these are usually nonscarring and follow the Blaschko lines,6 which, on the scalp, have a spiral distribution centered on the vertex9 (Fig. 1D). It would appear that inflammatory dermatoses that follow the Blaschko lines are the result of a genetic mosaicism, in which a clone of abnormal cells remains inactive until an environmental factor stimulates its growth.10 The overlying skin may be normal, erythematous, or show signs of discoid lupus. The histopathology findings in linear LP include a predominantly lobular lymphocytic panniculitis with hyaline fat necrosis,7 as observed in other forms of LP. Our patient underwent 2 skin biopsies. The first showed a dense lymphocytic infiltrate mainly affecting the deep dermis and adipose tissue, with areas of fat necrosis (Fig. 2A) and vacuolar damage of the basal layer of the epidermis (Fig. 2B). The second biopsy revealed nodular lymphoid aggregates in which plasma cells were observed.
The main condition to be excluded in the differential diagnosis of linear LP affecting the scalp is alopecia areata. The presence of erythema, edema, and pain supports a diagnosis of LP, although the overlying skin may show no changes in the early stages. Other conditions to be considered in the differential diagnosis are morphea en coup de sabre, lipedematous alopecia, and panniculitis-like T-cell lymphoma. The most widely used drugs have been the antimalarials and topical, intralesional, and oral corticosteroids; these treatments have achieved a good response in most cases.7 In summary, linear LP is a rare clinical variant of LP distributed along the Blaschko lines that presents a linear, annular, or arcuate pattern depending on the site of the lesions.
We have reported the second case of annular LP localized to the scalp. The condition presented clinically as painful erythematous plaques of nonscarring alopecia in a young white man. LP should be included in the differential diagnosis of focal, linear, or annular plaques of alopecia situated on the scalp, particularly if they are erythematous or painful.
Please cite this article as: Mitxelena J, Martínez-Peñuela A, Cordoba A, Yanguas I. Paniculitis lúpica de distribución lineal y anular localizada en el cuero cabelludo. Actas Dermosifiliogr. 2013;104:936–939.